Abstract
Background
Atherosclerosis leading to cardiovascular disease (CVD) is the main cause of mortality and morbidity in patients with rheumatoid arthritis (RA). Paraoxonase1 (PON1) is the best understood member of plasma paraoxonases with anti-atherogenic properties.
Patients and methods
Spanish RA (n = 549) consecutively recruited from 1 single center and 477 ethnically matched healthy controls were included in a case-control study. The concentration of PON1 was evaluated by means of an enzyme-linked immunosorbent sssay (ELISA). An arylesterase/paraoxonase assay kit was used to evaluate PON1 activity. Sample genotyping was performed by using TaqMan assays-on-demand. All results were expressed as medians ± interquartile range. One-way ANOVA comparisons were done using a nonparametric Kruskall-Wallis test. P values under 0.05 were considered to be significant.
Results
The concentration of PON1 in the RA group was higher than in control group (p = 0.0003), although the differences were not significant when PON1 activities were compared between both groups. No significant differences were found related to distributions of rs662 genotypes in RA patients compared to healthy controls. Among rs854860 polymorphisms, overall genotype was widely distributed between RA patients and controls. Overall PON1 concentration in plasma was not significantly different between individuals carrying any of rs662 (p = 0.8501) or rs854860 (p = 0.2741) polymorphisms. Although PON1 levels were not associated with any of the SNPs in the study, differences appear when enzyme activities are compared for each SNP separately. CVD in RA patients correlate with increased PON1 levels and lower PON1 activity.
Conclusions
Although protective role of PON1 against oxidative damage in vivo could be related to other activities, in our study arylesterase activity was useful to identify phenotypic differences with emphasis placed on two SNPs coding for nonconservative amino acid changes in the functional protein.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Atherosclerosis leading to cardiovascular disease (CVD) is the main cause of mortality and morbidity in patients with rheumatoid arthritis (RA) [1]. Both diseases share their pathophysiology so closely that atherosclerosis can be considered as an extra articular manifestation of RA [2]. Chronic inflammation plays a pivotal role as it is inferred from the lower CVD risk association following treatment with disease-modifying anti-rheumatic drugs (DMARDs) [3].
The synovium is the inflammatory target in RA, the most disabling and prevalent among many forms of inflammatory arthritis [4,5,6]. RA synovitis is histopathologically characterized by a massive immuno-inflammatory cell infiltration and secreted chemical mediators leading to destruction of the adjacent bone and cartilage [7]. RA shows features of an autoimmune-like process affected by multiple factors, including some HLA alleles, age, sex, and environment, but the exact etiology remains still unknown [8, 9].
RA and atherosclerosis have their own risk factors and may exist separately; however, when disease-related risk factors converge in a single individual, the diagnosis worsens. Increased secretion of cytokines in RA-inflamed joints generates increased oxidative stress, mainly due to the presence of reactive oxygen species (ROS) [10]. These intermediaries have harmful effects on the cell membrane lipids, altering cell structure and function, its gene expression, and promoting cell apoptosis that can lead to degenerative diseases [11]. Among plasma lipoproteins, the role of LDL (low-density lipoprotein) in inflammation and atherogenesis has been extensively studied. By itself, LDL is not proinflammatory or proatherogenic, but its chemical alteration has been described to change its properties [12]. The best known of these is the oxidation, both on the lipidic molecule itself or in the apo B-associated protein [13]. In contrast, high-density lipoprotein (HDL) protects at least some anti-inflammatory components [14].
Protection against oxidative damage is carried out by means of antioxidant enzymes, among them paraoxonase (PON) and arylesterase [15]. PON1 is the best understood member of plasma paraoxonases with anti-atherogenic properties. Genes for PON1, PON2, and PON3 are located on the long arm of chromosome 7 (7q21.3-q22.1) [16]. Although PON2 is expressed widely in a number of tissues, including liver, lungs, brain, and heart, it is not present in blood [17]. On the other hand, PON1 and PON3 are expressed in the liver and released to the blood stream where they associate with HDL [18, 19]. Human plasma paraoxonase (HuPON1) is a 354 amino acid calcium-dependent enzyme that hydrolyzes esters, including organophosphates and lactones, but the exact role in vivo is still unclear [20]. It is thought that PON1 contribute to inactivate LDL peroxidation, a key process in the pathophysiology of atherosclerosis and the onset of CVDs [21]. Besides other polimorphysms in the promoter region, there are two interesting coding polymorphisms Q192R and L55M. At least Q192R has been implicated in the different affinities and catalytic activities.
The objective of this study was to analyze the contribution of different single-nucleotide polymorphisms (SNPs) in the coding region of PON1 gene in subjects affected with rheumatoid arthritis. Furthermore, we compared the concentration and activity according to the different genotypes studied.
Methods
Patients and blood samples
Five hundred forty-nine white Spanish RA (69% women) consecutively recruited from a single center (Hospital Clínico San Carlos, Madrid) and 477 ethnically matched healthy controls (51% women), mainly blood donors and staff members, were included in a case-control study. The RA diagnosis was established based on the ACR criteria. The mean age at onset was 53 ± 14, 59% patients carried the shared epitope; 75% were positive for rheumatoid factor and 50% presented anti-CCP antibodies. All patients were included in the study after written informed consent and the study was approved by the institutional Ethics Committee (Hospital Clinico San Carlos).
Blood samples were obtained after 8–12-h fasting. The samples were centrifuged at 3000 r.p.m. for 10 min to obtain plasma that were aliquoted and stored at − 70 °C until the day of analysis.
Genotyping
Sample genotyping was performed by using TaqMan assays-on-demand (Applied Biosystems C_2548962_20 and C_2259750_20 corresponding to rs662 and rs854560 respectively). The 5-μl PCR reaction with 1× TaqMan Universal Master Mix, 1× probe and primers assay mix and 10 ng of genomic DNA was performed using 384 well-plates in a 7900HT Fast Real-Time PCR system, under manufacturer recommended conditions (Applied Biosystems, Foster City, CA, USA).
Genotyping statistical analysis was performed with standard statistical software (Epi Info v. 6.02; World Health Organization, Geneva, Switzerland and SPSS v 12.0). Phenotype and genotype frequencies in patients and controls were compared by chi-square test or Fisher’s exact test. Strength of association was given as odds ratio (OR) with a 95% confidence interval and p values under 0.05 were considered statistically significant. Haplotypic frequencies were estimated using the expectation-maximization algorithm implemented in the Arlequin v2.0 software, with a number of iterations set at 5000 and initial conditions at 50, with an Δ value of 10−7.
Measurement of enzymatic activity of PON1
An arylesterase/paraoxonase assay kit from ZeptoMetrix (Buffalo, New York) Cat# 0801119 was used to measure PON1 activity. In this assay, arylesterase/paraoxonase catalyzes the cleavage of phenyl acetate resulting in phenol formation. The rate of formation of phenol was measured by monitoring the increase in absorbance at 270 nm at 25 °C.
Briefly, PON1 activity was measured at 25 °C by adding 6.7 μl of plasma or standard diluted 1:2 in 20 mM Tris/HCl containing 10 mM CaCl2 to 1000 μl substrate buffer (20 mM Tris/HCl buffer, pH 8.0, containing 1 mM CaCl2 and 4 mM phenyl acetate). The rate of generation of phenol was recorded at 270 nm for 1 min following 20 s of lag time. Enzymatic activity was calculated using the phenol molar extinction coefficient 1310 M−1 cm−1. Each measurement was corrected using a standard of purified paraoxonase and adequate blanks. Experiments were done by duplicate and activities were expressed as U/ml.
Quantification of PON1 by ELISA
The concentration of PON1 in serum samples was evaluated by means of an enzyme-linked immunosorbent assay (ELISA). Briefly, 96-well plates were coated overnight at 4 °C with 50 μL of a dilution 1:100 of capture antibody (Goat IgG) PON1 (N-20). Santa Cruz Biotechnology and then blocked with 5% nonfat dry milk. PON1 Standards (Abnova Corporation) and 1:5 dilutions of plasma samples were incubated overnight in a volume of 50 μl by triplicate. Sandwich was completed incubating with 50 μl of detecting antibody (Mouse IgG1) PON1 (17A12) diluted 1:100 for 4 h at room temperature in a humid atmosphere and after incubated with 50 μl/well of secondary antibody diluted 1:3000 Goat anti-Mouse IgG1-HRP, Santa Cruz Biotechnology, at room temperature for at least 1 h. All washes between incubations were done with several changes of PBS/0.05% Tween 20, and antibodies were diluted in PBS with 1% nonfat dry milk.
Detection was carried out adding 50 μl/well of substrate solution (TMB), and reaction was stopped with 100 μl/well of 2 M H2SO4. Optical densities at 450 nm were measured with a plate.
Statistics
All results were expressed as medians ± interquartile range. Gaussian distributions were not assumed and one-way ANOVA comparisons were done using a nonparametric Kruskall-Wallis test. A p value under 0.05 was considered to be significant.
Results
PON1 concentrations and activities in RA patients and healthy controls
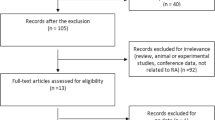
In order to investigate the possible existence of differences between patients with RA and healthy individuals, relative to the enzyme activity of PON1 and/or its plasma concentration; 100 individuals of our cohort, matched by gender and age, were randomly selected (50% RA, 50% healthy controls).
The concentration of PON1 in the RA group was higher than in control group (p = 0.0003), although the differences were not significant when PON1 activities were compared between both groups (Fig. 1). In addition, the concentration range was more widely distributed in the RA group than in controls. The differences were most evident when comparing the groups according to gender. Although in the control group, in accordance with their similar activities, there were no differences in PON1 levels between men and women, in the RA group, PON1 activity was sex dependent with women showing higher plasma concentrations of PON1 Fig. 1.
Distribution of PON1 rs662 and rs854560 genotypes in RA patients and control subjects
In order to evaluate the effect of genetic variants of PON1 in the previous results, two single-nucleotide polymorphisms (SNPs) rs662, encoding the amino acidic changes Q192R, and rs854860 encoding the L55M change of PON1. To obtain greater statistical power, the study was extended to the entire cohort available. The genotypic frequencies between patients and controls for both polymorphisms were in Hardy-Weinberg equilibrium (data not shown).
The data showed no significant differences between the general distributions of rs662 genotypes in RA patients compared to healthy controls. In 91% of the individuals were A carriers of the rs662 (A/A (50.6% vs. 50.5% and A/G (40.6% vs. 41.3%)), however, were equally distributed between AR and control group (Table 1). The G/G genotype was the least common in both groups but, again, it was distributed equally in RA or healthy controls (8.7% vs. 8.2%). Considering the higher prevalence of RA among women, prevalence of RA in the cohort studied, the number of women was three times higher; however, the distributions of genotypes between RA and controls were similar and independent of gender (Table 1).
Among rs854860 polymorphisms, overall genotype was widely distributed A/A (16.9% vs 19.3%), A/T (46.7% vs 48.8%), and T/T (36.5% vs 31.8%) between RA patients and controls respectively (Table 1). In addition, for both SNPs, carrier distribution was similar in RA and control group.
PON1 plasma concentration is independent of (PON1) Q192R or (PON1) L55M polymorphisms
Overall PON1 concentration in plasma was not significantly different between individuals carrying any of rs662 (p = 0.8501) or rs854860 (p = 0.2741) polymorphisms. This was also the case when male and female were analyzed separately or when control or RA groups were compared for each SNP (data not shown).
(PON1) Q192R but not (PON1) L155M is involved in different paraoxonase activities
Although PON1 levels were not associated with any of the SNPs in the study, differences appear when enzyme activities are compared for each SNP separately.
When the enzyme activities were analyzed for polymorphism rs854860, none of the genotypes were associated with differential enzyme activity in either the control group or the RA group (Table 2). The same analysis, however, for rs662 did show differences between RA patients according to genotype (p = 0.0181). In addition, the lower activities were inversely related to the G allele copy numbers: (A/A) = 10.2 (5.4–14.7) > (A/G) = 4.5 (3.2–7.7) > (G/G) = 2.7 (2.0–5.8) U/ml. Although not statistically significant, the trend towards the lower enzyme activity of PON1 among allele G carriers was also present in the control group (Table 2 and Fig. 2).
CVD in RA patients correlate with increased PON1 levels and lower PON1 activity
Only 2 out of 50 patients with RA (4%) used in our cohort to determine the activity and concentration of PON1 showed cardiovascular manifestations in their clinical records. Both episodes were referred to two men of 72 and 68 years with respective diagnoses of angina pectoris, without the need for required revascularization and an acute coronary syndrome, which did require revascularization by coronary angioplasty.
Both patients were heterozygous for SNP rs662 (A/G), while for rs854860, one was (A/T) and the other (T/T). Interestingly, both RA patients with had lower PON1 activities 3.03 (2.90–3.17) vs. 7.11 (4.05–12.65) (p = 0.1173) and higher PON1 concentrations when compared to the remaining RA patients without cardiovascular manifestations. (40.37 (14.14–66.60)) vs. (16.15 (12.52–20.07)) (p = 0.5112).
Discussion
Because of their high prevalence, autoimmune, inflammatory, and CVD generate high socioeconomic costs. Coexistence of both diseases is not uncommon, particularly in the elderly. In the case of RA, CVD is the main cause of death. Atherosclerotic plaque and RA joint share many features, such as infiltration of mononuclear cells, upregulation of cytokines, and matrix-degrading enzymes as well as interactions of immune cells leading to the inflammatory process and tissue destruction. Oxidative stress plays an important role in diseases characterized by chronic inflammation; in particular, ROS are key signaling molecules. Several mechanisms including the enzymatic activity of PON1, in association with HDL, prevent the LDL oxidation and thus promoting anti-atherogenic activities. As other proteins, PON1 expression and activity is largely influenced by SNPs [22,23,24]. In particular, polymorphisms in residues L55M and Q192R have been differentially implicated in substrate dependent activities without conclusive data and Jarvik et al. reported that PON1 phenotype, on the basis of its activity, was a more appropriate predictor of vascular disease than simple genotyping [25], but few studies have measured PON1 activity and concentration. Here, we examined the implication of two PON1 SNPs and their association with PON1 concentration and/or activity in RA patients and control individuals.
Measurement of the PON1 concentrations and activities in RA patients and healthy controls indicate the higher variability and concentration ranges in RA. Interestingly, in our study, PON1 activity was sex dependent with women showing higher plasma concentrations of PON1. These results likely indicate the existence of a compensatory mechanism to restore PON1 activity through the increase of PON1 plasma levels. In our study, both polymorphisms were equally distributed in RA patients and controls, and none of them appear to be differentially associated neither with RA nor in male not female. Genotypic distributions showed similar distributions and are in agreement with hypercontrols, strictly selected on the basis of clinical parameters and nonhereditary AR background a network of Spanish researchers working on the genomic basis of immunomediated diseases [26].
Atherosclerosis induced by LDLs is somehow related to the lesser antioxidant capacity of PON1. Reduction in enzymatic activity could be caused by lower PON1 levels or a reduced catalytic capacity of the enzyme. Mutations at residues L55M and Q192R have been studied with disappointing results about their implication in increased risk for CVD. While the PON1 alleles 192R and 55L have been associated with CVD, the Q192R polymorphism has been described as a risk factor for CVD [27]. On the other hand, a recent study point to the HDL anti-HDL-PON1 axis as a key factor in CVD occurrence in RA [28].
In our study, the plasma concentration of PON1 was independent of both polymorphisms; therefore, the change of L ➔ M in position 55 does not affect the concentration nor the activity of PON1. However, Q192R polymorphisms clearly affect the functionality of PON1, reducing its enzyme activity to a greater extent in patients with RA than healthy controls when allele G is present. In support of this argument, it was also observed that PON1 activity was reduced when haplotypes were studied. Only three out of four possible combinations of alleles, rs662 and rs854860, were presented in our sample: A/T, A/A, and G/A, coding respectively for amino acid changes in positions 192/55 Q/M, Q/L, and L/R. None of them were associated with PON1 concentrations. Although differential activities were only found among patients with RA, lower activity was found in both RA 4.1 (2.7–7.4) and control 5.7 (4.9–8.5) U/ml were from haplotype G/A. These results agree with our previous results, indicating that the activities of minor PON1 are in close correlation with polymorphism Q192R and the absence of association of polymorphisms rs854860 in the activity of PON1.
Although protective role of PON1 against oxidative damage in vivo could be related to other activities, in our study, arylesterase activity was useful to identify phenotypic differences with emphasis placed on two SNPs coding for nonconservative amino acid changes in the functional protein. We performed a complete study of PON1 from genetics to protein function in RA patients. PON1 activity can be affected in many ways, besides age, sex, HDL levels, and several environmental factors, polymorphic residues can also be responsible, affecting both enzyme expression and their promiscuous catalytic properties to hydrolyze aryl esters, phosphate esters, or lactones. In a recent study, authors conclude that contributions of the genetic markers to the PON1 phenotype are stronger than the contributions of the lifestyle determinants [29]. Moreover, genetic implication of noncoding polymorphisms located in the paraoxonase promoter region of paraoxonase gene locus appears to have supporting evidence of lower PON1 activities in the absence of coding polymorphisms association [30,31,32].
Conclusions
Arylesterase activity was useful to identify phenotypic differences with emphasis placed on two SNPs coding for nonconservative amino acid changes in the PON1 functional protein.
Q192R polymorphisms clearly affect the functionality of PON1, reducing its enzyme activity to a greater extent in patients with RA than healthy controls when allele G is present.
The activity of PON1 can be affected in many ways, besides age, sex, HDL levels, and several environmental factors, polymorphic residues can also be responsible, affecting both the enzymatic expression, and its promiscuous catalytic properties to hydrolyze aryl esters, phosphate esters, or lactones, thus determining cardiovascular risk in patients with RA.
Availability of data and materials
We confirm the data and material availability.
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- PON1:
-
paraoxonase1
- RA:
-
rheumatoid arthritis
- CVD:
-
cardiovascular disease
- ELISA:
-
enzyme-linked immunosorbent sssay
- DMARDs:
-
disease-modifying anti-rheumatic drugs
- ROS:
-
reactive oxygen species
- LDL:
-
low-density lipoprotein
- HDL:
-
high-density lipoprotein
- SNPs:
-
single-nucleotide polymorphisms
References
Cavagna L, Boffini N, Cagnotto G, Inverardi F, Grosso V, Caporali R (2012) Atherosclerosis and rheumatoid arthritis: more than a simple association. Mediat Inflamm 2012:147354. https://doi.org/10.1155/2012/147354
Full LE, Ruisanchez C, Monaco C (2009) The inextricable link between atherosclerosis and prototypical inflammatory diseases rheumatoid arthritis and systemic lupus erythematosus. Arthritis Res Ther 11:217. https://doi.org/10.1186/ar2631
van Halm VP, Nurmohamed MT, Twisk JWR et al (2006) Disease-modifying antirheumatic drugs are associated with a reduced risk for cardiovascular disease in patients with rheumatoid arthritis: a case control study. Arthritis Res Ther 8:R151. https://doi.org/10.1186/ar2045
Goronzy JJ, Weyand CM (2005) Rheumatoid arthritis. Immunol Rev 204:55–73. https://doi.org/10.1111/j.0105-2896.2005.00245.x
Firestein GS (2003) Evolving concepts of rheumatoid arthritis. Nature 423:356–361. https://doi.org/10.1038/nature01661
Walsh NC, Crotti TN, Goldring SR, Gravallese EM (2005) Rheumatic diseases: the effects of inflammation on bone. Immunol Rev 208:228–251. https://doi.org/10.1111/j.0105-2896.2005.00338.x
Sharma J, Bhar S, Devi CS (2017) A review on interleukins: the key manipulators in rheumatoid arthritis. Mod Rheumatol 27:723–746. https://doi.org/10.1080/14397595.2016.1266071
Angelotti F, Parma A, Cafaro G et al One year in review 2017: pathogenesis of rheumatoid arthritis. Clin Exp Rheumatol 35:368–378
Klareskog L, Amara K, Malmström V (2014) Adaptive immunity in rheumatoid arthritis: anticitrulline and other antibodies in the pathogenesis of rheumatoid arthritis. Curr Opin Rheumatol 26:72–79. https://doi.org/10.1097/BOR.0000000000000016
Quiñonez-Flores CM, González-Chávez SA, Del Río Nájera D, Pacheco-Tena C (2016) Oxidative stress relevance in the pathogenesis of the rheumatoid arthritis: a systematic review. Biomed Res Int 2016:6097417–6097414. https://doi.org/10.1155/2016/6097417
Le Rossignol S, Ketheesan N, Haleagrahara N (2018) Redox-sensitive transcription factors play a significant role in the development of rheumatoid arthritis. Int Rev Immunol 37:129–143. https://doi.org/10.1080/08830185.2017.1363198
Navab M, Anantharamaiah GM, Reddy ST, van Lenten BJ, Ansell BJ, Fogelman AM (2006) Mechanisms of disease: proatherogenic HDL--an evolving field. Nat Clin Pract Endocrinol Metab 2:504–511. https://doi.org/10.1038/ncpendmet0245
Tsimikas S (2006) Oxidized low-density lipoprotein biomarkers in atherosclerosis. Curr Atheroscler Rep 8:55–61
Schmidt A, Geigenmüller S, Völker W, Buddecke E (2006) The antiatherogenic and antiinflammatory effect of HDL-associated lysosphingolipids operates via Akt -->NF-kappaB signalling pathways in human vascular endothelial cells. Basic Res Cardiol 101:109–116. https://doi.org/10.1007/s00395-005-0582-z
Isik A, Koca SS, Ustundag B, Celik H, Yildirim A (2007) Paraoxonase and arylesterase levels in rheumatoid arthritis. Clin Rheumatol 26:342–348. https://doi.org/10.1007/s10067-006-0300-8
Primo-Parmo SL, Sorenson RC, Teiber J, La Du BN (1996) The human serum paraoxonase/arylesterase gene (PON1) is one member of a multigene family. Genomics 33:498–507
Mochizuki H, Scherer SW, Xi T, Nickle DC, Majer M, Huizenga JJ, Tsui LC, Prochazka M (1998) Human PON2 gene at 7q21.3: cloning, multiple mRNA forms, and missense polymorphisms in the coding sequence. Gene 213:149–157
Mackness MI, Hallam SD, Peard T, Warner S, Walker CH (1985) The separation of sheep and human serum “A”-esterase activity into the lipoprotein fraction by ultracentrifugation. Comp Biochem Physiol B 82:675–677
Reddy ST, Wadleigh DJ, Grijalva V, Ng C, Hama S, Gangopadhyay A, Shih DM, Lusis AJ, Navab M, Fogelman AM (2001) Human paraoxonase-3 is an HDL-associated enzyme with biological activity similar to paraoxonase-1 protein but is not regulated by oxidized lipids. Arterioscler Thromb Vasc Biol 21:542–547
van Himbergen TM, van Tits LJH, Roest M, Stalenhoef AFH (2006) The story of PON1: how an organophosphate-hydrolysing enzyme is becoming a player in cardiovascular medicine. Neth J Med 64:34–38
Mackness MI, Arrol S, Durrington PN (1991) Paraoxonase prevents accumulation of lipoperoxides in low-density lipoprotein. FEBS Lett 286:152–154
Legein B, Temmerman L, Biessen EAL, Lutgens E (2013) Inflammation and immune system interactions in atherosclerosis. Cell Mol Life Sci 70:3847–3869. https://doi.org/10.1007/s00018-013-1289-1
Salisbury D, Bronas U (2014) Inflammation and immune system contribution to the etiology of atherosclerosis: mechanisms and methods of assessment. Nurs Res 63:375–385. https://doi.org/10.1097/NNR.0000000000000053
Tajbakhsh A, Rezaee M, Rivandi M, Forouzanfar F, Afzaljavan F, Pasdar A (2017) Paraoxonase 1 (PON1) and stroke; the dilemma of genetic variation. Clin Biochem 50:1298–1305. https://doi.org/10.1016/j.clinbiochem.2017.08.001
Jarvik GP, Rozek LS, Brophy VH, Hatsukami TS, Richter RJ, Schellenberg GD, Furlong CE (2000) Paraoxonase (PON1) phenotype is a better predictor of vascular disease than is PON1(192) or PON1(55) genotype. Arterioscler Thromb Vasc Biol 20:2441–2447
Julià A, Domènech E, Chaparro M, García-Sánchez V, Gomollón F, Panés J, Mañosa M, Barreiro-de Acosta M, Gutiérrez A, Garcia-Planella E, Aguas M, Muñoz F, Esteve M, Mendoza JL, Vera M, Márquez L, Tortosa R, López-Lasanta M, Alonso A, Gelpí JL, García-Montero AC, Bertranpetit J, Absher D, Myers RM, Gisbert JP, Marsal S (2014) A genome-wide association study identifies a novel locus at 6q22.1 associated with ulcerative colitis. Hum Mol Genet 23:6927–6934. https://doi.org/10.1093/hmg/ddu398
Chen H, Ding S, Zhou M et al (2018) PON1 L55M and Q192R gene polymorphisms and CAD risks in patients with hyperlipidemia : clinical study of possible associations. Herz 43:642–648. https://doi.org/10.1007/s00059-017-4611-0
Rodríguez-Carrio J, López-Mejías R, Alperi-López M, López P, Ballina-García FJ, González-Gay MÁ, Suárez A (2016) Paraoxonase 1 activity is modulated by the rs662 polymorphism and IgG anti-high-density lipoprotein antibodies in patients with rheumatoid arthritis: potential implications for cardiovascular disease. Arthritis Rheumatol (Hoboken, NJ) 68:1367–1376. https://doi.org/10.1002/art.39609
Roest M, van Himbergen TM, Barendrecht AB, Peeters PHM, van der Schouw YT, Voorbij HAM (2007) Genetic and environmental determinants of the PON-1 phenotype. Eur J Clin Investig 37:187–196. https://doi.org/10.1111/j.1365-2362.2007.01769.x
Deakin S, Leviev I, Brulhart-Meynet M-C, James RW (2003) Paraoxonase-1 promoter haplotypes and serum paraoxonase: a predominant role for polymorphic position - 107, implicating the Sp1 transcription factor. Biochem J 372:643–649. https://doi.org/10.1042/BJ20021670
Mackness B, Davies GK, Turkie W, Lee E, Roberts DH, Hill E, Roberts C, Durrington PN, Mackness MI (2001) Paraoxonase status in coronary heart disease: are activity and concentration more important than genotype? Arterioscler Thromb Vasc Biol 21:1451–1457
Ayub A, Mackness MI, Arrol S, Mackness B, Patel J, Durrington PN (1999) Serum paraoxonase after myocardial infarction. Arterioscler Thromb Vasc Biol 19:330–335
Funding
This work was supported by the following grants: Fondo de Investigaciones Sanitarias FIS 04/1698 and RD16/0012/0004.
Author information
Authors and Affiliations
Contributions
AM. DNA bank. ELISA and SNPs performance
BFG. Coordination of the study. Data analysis. Manuscript generation
EH. DNA bank
LRR. Statistics analysis
JV. DNA bank
EU. DNA bank
JRL. Coordination of the study. Data analysis. Manuscript generation
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients were included in the study after written informed consent and the study was approved by the institutional Ethics Committee (Hospital Clinico San Carlos).
Disclosures
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mucientes, A., Fernández-Gutiérrez, B., Herranz, E. et al. Functional implications of single nucleotide polymorphisms rs662 and rs854860 on the antioxidative activity of paraoxonase1 (PON1) in patients with rheumatoid arthritis. Clin Rheumatol 38, 1329–1337 (2019). https://doi.org/10.1007/s10067-018-4394-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4394-6