Abstract
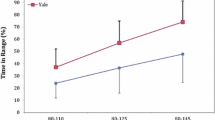
The purpose of this study was to elucidate the relationship between strict control of blood glucose (BG) and mortality reduction with the use of an artificial pancreas (AP). Patients were evaluated in the (1) early phase (E phase: mean 3.3 ± 2.6 days after admission, n = 84) and in the (2) late phase (L phase: mean 9.9 ± 3.3 days, n = 88), and were classified into a (1) group with a higher daily mean BG level (BGm) (BGmXa: BGm above Xmg/dl) and a (2) group with a lower BGm (BGmXb: BGm below Xmg/dl). Each group was classified into a (1) subgroup with a higher daily standard deviation of the BG levels (BGsd) and a (2) subgroup with a lower BGsd. In the E phase, the (1) mortality of the BGm200a group was significantly higher than that of the BGm200b group (56 vs. 29%, p < 0.05), and (2) in the BGm200b group, the mortality of the subgroup with a BGsd above 14 mg/dl was significantly higher than that with a BGsd below 14 mg/dl (46 vs. 17%, p < 0.025). In the L phase, the mortality of the BGm175a group was significantly higher than that of the BGm175b group (50 vs. 28%, p < 0.05). In conclusion, (1) a higher BGm and (2) higher BGsd in the E phase were prognostic risk factors. Based on the findings, it was considered that the target for BG control should be set at (1) BGm below 200 mg/dl and BGsd below 14 mg/dl in the E phase, and (2) BGm below 175 mg/dl in the L phase.




Similar content being viewed by others
References
The Diabetic Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Eng J Med. 1993;329:977–86.
United kingdom Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylurea or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS33). Lancet. 1998;352:837–53.
Malmberg K. Prospective randomized study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus: DIGAMI (Diabetes Mellitus, Insulin Glucose Infusion in Acute Myocardial Infarction) Study Group. B M J. 1997;314:1512–5.
Furnary AP, Zerr KJ, Grunkemeier GL, Starr A. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures. Ann Thorac Surg. 1999;67:352–62.
Van den Berghe G, Wouters P, Weekers F, Werwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Buillon R. Intensive insulin therapy in the critically ill patients. N Eng J Med. 2001;345:1359–67.
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, Van Wijngaerden E, Bobbaers H, Buillon R. Intensive insulin therapy in the Medical ICU. N Engl J Med. 2006;354:449–61.
Finney SJ, Zekveld C, Elia A, Evans TW. Glucose control and mortality in critically ill patients. JAMA. 2003;290:2041–7.
Krinsley JS. Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc. 2004;79:992–1000.
The International Surviving Sepsis Campaign Guidelines Committee. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327.
Taylor JH, Beilman GJ. Hyperglycemia in the intensive care unit: no longer just a marker of illness severity. Surg Infect. 2005;6:233–45.
Baird TA, Parsons MW, Phanh T, Butcher KS, Desmond PM, Tress BM, Colman PG, Chambers BR, Davis SM. Persistent poststroke hyperglycemia is independently associated with infarct expansion and worse clinical outcome. Stroke. 2003;34:2208–14.
Vogelzang M, van der Horst ICC, Nijsten MWN. Hyperglycaemic index as a tool to assess glucose control: a retrospective study. Crit Care. 2004;8:R122–7.
Srinivasan V, Spinella PC, Drott HR, Roth CL, Helfaer MA, Nadkarni V. Association of timing, duration and intensity of hyperglycemia with intensive care unit mortality in critically ill children. Pediatr Crit Care Med. 2004;5:329–36.
Krinsley JS, Jones RL. Cost analysis of intensive glycemic control in critically ill adult patients. Chest. 2006;129:644–50.
Van den Berhge G, Wouters PJ, Kesteloot K, Hilleman DE. Analysis of healthcare resource utilization with intensive Insulin therapy in critically ill patients. Crit Care Med. 2006;34:612–6.
Hirsch IB, Brownlee M. Should minimal blood glucose variability become the gold standard of glycemic control? J Diabetes Complicat. 2005;19:178–81.
Wintergerst KA, Buckingham B, Gandrud L, Wong BJ, Kache S, Wilson DM. Association of hypoglycemia, hyperglycemia, and glucose variability with morbidity and death in the pediatric intensive care unit. Pediatrics. 2006;118:173–9.
Egi M, Bellomo R, Stachowski E, French CJ, Hart G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology. 2006;105:244–52.
Vlasselaers D, Milants I, Desmet L, Wouters PJ, Vanhorebeek I, Van den Heuvel I, Mesotten D, Casaer MP, Meyfroidt G, Ingels C, Muller J, Van Cromphaut S, Van den Berghe G. Intensive insulin therapy for patients in paediatric intensive care: a prospective, randomized controlled study. Lancet. 2009;373:547–56.
Brunkhorst FM, Engel C, Bloos F, Hellmann AM, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K. for the German Competence Network Sepsis (SepNet). Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39.
NICE-SUGAR Study Investigators, Finster S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hebert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ. Intensive versus conventional glucose control in critically ill patients. N Eng J Med. 2009;360:1283–97.
Laver S, Preston S, Turner D, Mckinstry C, Padkin A. Implementing intensive insulin therapy: development and audit of the bath insulin protocol. Anaesth Intensive Care. 2004;32:311–6.
Kanji S, Singh A, Tierney M, Meggison H, McIntyre L, Hebert PC. Standardization of intravenous insulin therapy improves the efficiency and safety of blood glucose control in critically ill adults. Intensive Care Med. 2004;30:804–10.
Van den Berhge G, Wilmer A, Milants I, Wouters PJ, Bouckaert B, Bruyninckx F, Bouillon R, Schetz M. Intensive insulin therapy in mixed medical/surgical intensive care units. Benefit versus harm. Diabetes. 2006;55:3151–9.
Orford NR. Intensive insulin therapy in septic shock. Crit Care Resusc. 2006;8:230–4.
McNay EC, Williamson A, McCrimmon RJ, Sherwin RS. Cognitive and neural hippocampal effects of long-term moderate recurrent hypoglycemia. Diabetes. 2006;55:1088–95.
Mackenzie I, Ingle S, Zaidi S, Buczaski S. Tight glycemic control: a survey of intensive care practice in large English hospitals. Intensive Care Med. 2005;31:1136.
Plank J, Blaha J, Cordingley J, Wilinska ME, Chassin LJ, Morgan C, Squire S, Haluzik M, Kremen J, Svacina S, Toller W, Plasnik A, Ellmerer M, Hovorka R, Pieber TR. Multicentric, randomized, controlled trial to evaluate blood glucose control by the model predictive control algorithm versus routine glucose management protocols in intensive care unit patients. Diabetes Care. 2006;29:271–6.
De Block C, Keenoy BMY, Van Gaal L, Rogiers P. Intensive insulin therapy in the intensive care unit. Diabetes Care. 2006;29:1750–6.
Scalea TM, Bochicchio BV, Bochicchio KM, Johnson SB, Joshi M, Pyle A. Tight glycemic control in critically injured trauma patients. Ann Surg. 2007;246:605–12.
Collier B, Dossett LA, May AK, Diaz JJ. Glucose control and the inflammatory response. Nutr Clin Pract. 2008;23:3–15.
Vriesendorp TM, van Santen S, DeVries H, De Jonge E, Rosendaal FR, Schultz MJ, Hoekstra JBL. Predisposing factors for hypoglycemia in the intensive care unit. Crit Care Med. 2006;34:96–101.
Hoshino M, Haraguchi Y, Kirita M. Nutritional treatment of septic patients with decreased glucose tolerance with the artificial pancreas. In 7th World Congress of the International Society for Artificial Organs [Abstract]. No. G-02-36989 1989; p 308.
Haraguchi Y, Hoshino M, Kirita M. Intravenous hyperalimentation and artificial endocrine pancreas for patients with impaired glucose tolerance. In 25th Congress of European Society for Surgical Research [Abstract]. No. 178 1990; p 84.
Hoshino M, Haraguchi Y, Hirasawa H, Sakai M, Saegusa H, Hayashi K, Horita N, Ohsawa H. Close relationship of tissue plasminogen activator-plasminogen activator inhibitor-1 complex with multiple organ dysfunction syndrome investigated by means of the artificial pancreas. Crit Care. 2001;5:88–9.
Hoshino M, Haraguchi Y, Hirasawa H, Mizushima I, Tanaka C, Morita Y, Yokoi T, Sakai M. Measurement of insulin clearance and factors affecting insulin clearance in septic patients with glucose intolerance—analysis under strict blood glucose control by means of bedside-type artificial pancreas. Chiba Med J. 2006;82:149–61.
Hoshino M, Haraguchi Y, Mizushima I, Kajiwara S, Takagi M. Significance of the suppression of blood glucose variability in acutely ill severe patients with glucose intolerance evaluated by means of bedside-type artificial pancreas [Abstract] Crit Care. 2008;12 Suppl 2:S60.
Hoshino M, Haraguchi Y, Mizushima I, Sakai M, Kajiwara S, Takagi M. High blood glucose variability in acute phase is one of the most important risk factors relating to the outcome in acutely ill severe patients with glucose intolerance. [Abstract] Crit Care. 2009;13 Suppl 1:S49–50.
Hoshino M, Haraguchi Y, Muzushima I, Sakai M. Recent progress in mechanical artificial pancreas. J Artif Organs. 2009;12:141–9.
Bone RC, Balk RA, Cerra FB, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101:1644–55.
Vincent JL, de Mendonca A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units. Crit Care Med. 1998;26:1793–800.
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM. Surviving Sepsis Campaign Management Guidelines Committee. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32:858–73.
Laird AM, Miller PR, Kilgo PD, Meredith JW, Chang MC. Relationship of early hyperglycemia to mortality in trauma patients. J Trauma. 2004;56:1058–62.
Bochicchio GV, Sung Jin, Joshi M, Bochicchio K, Johnson SB, Meyer W, Scalea TM. Persistent hyperglycemia is predictive of outcome in critically ill trauma patients. J Trauma. 2005;58:921–4.
Dossett LA, Cao H, Mowery NT, Dortch MJ, Morris JM Jr, May AK. Blood glucose variability is associated with mortality in the surgical intensive care unit. Am Surg. 2008;74:679–85.
Ali NA, O’Brien JM Jr, Dungan K, Phillips G, Marsh CB, Lemeshow S, Connors AF Jr, Preiser JC. Glucose variability and mortality in patients with sepsis. Crit Care Med. 2008;36:2316–21.
Krinsley JS. Glycemic variability: a strong independent predictor of mortality in critically ill patients. Crit Care Med. 2008;36:3008–13.
Risso A, Mercuri F, Quagliaro L, Damante G, Ceriello A. Intermittent high glucose enhances apoptosis in human umbilical vein endothelial cells in culture. Am J Physiol Endocrinol Metab. 2001;281:E924–30.
Quagliaro L, Piconi L, Assaloni R, Martinelli L, Motz E, Ceriello A. Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells. Diabetes. 2003;52:2795–804.
Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, Colette C. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA. 2006;295:1681–7.
Esposito K, Nappo F, Marfella R, Giugliano G, Giugliano F, Ciotola M, Quagliaro L, Ceriello A, Guigliano D. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation. 2002;106:2067–72.
Holtfreter B, Bandt C, Kuhn SO, Grunwald U, Lehmann C, Schutt C, Grundling M. Serum osmolality and outcome in intensive care unit patients. Acuta Anaesthesiol Scand. 2006;50:970–7.
Otto N, Schindler R, Lun A, Boenisch O, Frei U, Oppert M. Hyperosmotic stress enhances cytokine production and decreases phagocytosis in vitro. Crit Care. 2008;12:R107.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 2.
Rights and permissions
About this article
Cite this article
Hoshino, M., Haraguchi, Y., Mizushima, I. et al. Close relationship between strict blood glucose control, including suppression of blood glucose variability, and mortality reduction in acutely ill patients with glucose intolerance investigated by means of a bedside-type artificial pancreas. J Artif Organs 13, 151–160 (2010). https://doi.org/10.1007/s10047-010-0509-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-010-0509-9