Abstract
Purpose
Hernia recurrence is an important complication following inguinal hernia repair. Primary closure of ventral hernia defects laparoscopically has been shown to reduce the risk of recurrence and seroma formation. The results for ventral hernias may potentially be applied to direct inguinal hernias. Our aim was to evaluate the value of primary closure of direct defects during laparoscopic inguinal hernia mesh repair in reducing the incidence of early recurrence.
Methods
A retrospective, single-center cohort study was conducted on cases performed from August 2016 to February 2018. Patients with direct inguinal hernias undergoing elective laparoscopic mesh repair were included. When performed, the direct hernia defect was primarily closed with extracorporeal non-absorbable interrupted sutures followed by standard placement of a lightweight mesh covering myopectineal orifices. Early recurrence was defined as occurring within 1 year of surgery.
Results
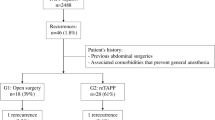
A total of 75 direct inguinal hernias in 53 patients who underwent surgery and completed at least 1 year of follow-up were analyzed. The mean age of patients was 63 years (range 44–82 years); with majority of patients being male (98.1%). There were no significant differences observed between the two patient populations in terms of demographics, mean operative time and risk factors. In 9 (16.9%) patients, the direct hernias were recurrent hernias and all underwent open mesh repair during the index hernia surgery. The majority of hernia repairs (63 hernias in 45 patients, 85%) were performed via the totally extraperitoneal (TEP) approach. 19 patients (35.8%) with 28 direct inguinal hernias underwent primary closure of the direct defect prior to mesh placement; while, 34 patients (64.2%) with 47 direct hernias did not undergo primary closure. There were 3 direct hernia recurrences (6.4%) at 1 year post-operatively, and all occurred in the non-closure group. In comparison, there were no recurrences in the closure group; however, this difference was not statistically significant (p = 0.289) in our study due to the small sample size.
Conclusion
Closure of direct inguinal hernia defects during laparoscopic mesh repair has been shown to reduce the incidence of early hernia recurrence in our retrospective study but future randomized controlled trials with large numbers would enable us to draw more robust conclusions and perhaps change the way we perform laparoscopic inguinal hernia repair.




Similar content being viewed by others
References
Martin-Del-Campo LA, Miller HJ, Elliott HL, Novitsky YW (2018) Laparoscopic ventral hernia repair with and without defect closure: comparative analysis of a single-institution experience with 783 patients. Hernia 22(6):1061–1065
Tandon A, Pathak S, Lyons NJ, Nunes QM, Daniels IR, Smart NJ (2016) Meta-analysis of closure of the fascial defect during laparoscopic incisional and ventral hernia repair. Br J Surg 103(12):1598–1607
Zhu Y, Liu M, Li J, Wang M (2019) Closure of direct inguinal hernia defect in laparoscopic hernioplasty to prevent seroma formation: a prospective double-blind randomized controlled trial. Surg Laparosc Endosc Percutan Tech 29(1):18–21
Li J, Zhang W (2018) Closure of a direct inguinal hernia defect in laparoscopic repair with barbed suture: a simple method to prevent seroma formation? Surg Endosc 32(2):1082–1086
F Usmani, S Wijerathne, S Malik, C Yeo, J. Rao, D Lomanto. Effect of direct defect closure during laparoscopic inguinal hernia repair (“TEP/TAPP plus” technique) on postoperative outcomes. Hernia. 2019 Sep 6. doi: 10.1007/s10029–019–02036–1. [Epub ahead of print]
Group, HerniaSurge (2018) International guidelines for groin hernia management. Hernia 22(1):1–165
Burcharth J (2014) The epidemiology and risk factors for recurrence after inguinal hernia surgery. Dan Med J 61(5):B4846
Bracale U, Melillo P, Pignata G, Di Salvo E, Rovani M, Merola G, Pecchia L (2012) Which is the best laparoscopic approach for inguinal hernia repair: TEP or TAPP? A systematic review of the literature with a network meta-analysis. Surg Endosc 26(12):3355–3366
Li J, Gong W, Liu Q (2019) Intraoperative adjunctive techniques to reduce seroma formation in laparoscopic inguinal hernioplasty: a systematic review. Hernia 23(4):723–731
Berney CR (2012) The Endoloop technique for the primary closure of direct inguinal hernia defect during the endoscopic totally extraperitoneal approach. Hernia 16:301–305
Reddy VM, Sutton CD, Bloxham L, Garcea G, Ubhi SS, Robertson GS (2007) Laparoscopic repair of direct inguinal hernia: a new technique that reduces the development of postoperative seroma. Hernia 11(5):393–396 Epub 2007 Jun 1
Daes J (2014) Endoscopic repair of large inguinoscrotal hernias: management of the distal sac to avoid seroma formation. Hernia 18(1):119–122
Ismail M, Garg M, Rajagopal M, Garg P (2009) Impact of closed-suction drain in preperitoneal space on the incidence of seroma formation after laparoscopic total extraperitoneal inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 19(3):263–266
Gao D, Wei S, Zhai C, Chen J, Li M, Gu C, Wu H (2015) Clinical research of preperitoneal drainage after endoscopic totally extraperitoneal inguinal hernia repair. Hernia 19(5):789–794
Fan JKM, Liu J, Chen K, Yang X, Xu X, Choi HK, Chan FSY, Chiu KWH, Lo CM (2018) Preperitoneal closed-system suction drainage after totally extraperitoneal hernioplasty in the prevention of early seroma formation: a prospective double-blind randomised controlled trial. Hernia 22(3):455–465
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the hospital’s ethics committee and waiver of consent was granted for this retrospective review.
Human and animal rights
The study including human participants has been performed in accordance with the ethical standards of the Declaration of Helsinki and its later amendments.
Informed consent
For this retrospective review, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ng, A.Y., Lin, J., Ching, S.S. et al. Does primary closure of direct inguinal hernia defect during laparoscopic mesh repair reduce the risk of early recurrence?. Hernia 24, 1093–1098 (2020). https://doi.org/10.1007/s10029-020-02257-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02257-9