Abstract
Purpose
Ventral hernia repair is one of the most frequently performed surgical procedures, though recurrences are common. Recurrence can be caused by impaired collagen formation or maturation; hence, patients with Ehlers-Danlos syndrome (EDS) are potentially at increased risk for hernia recurrence. EDS causes altered collagen metabolism, though little is known about the influence of EDS on ventral hernioplasty outcomes. This study aims to analyze these patients to report complication rates, recurrence rates, and, if possible, to give recommendations for surgical intervention.
Methods
A retrospective analysis between January 2000 and January 2017 was performed in a university hospital Belgium (UZ Ghent). Data on baseline characteristics, primary surgery, and hernias were extracted from patients’ medical charts. Noted endpoints were postoperative complications and recurrences.
Results
Fourteen patients (50% males) were included. Ten (71%) had an incisional hernia and four (29%) had a primary ventral hernia. Median age was 45 years (IQR 37.75–52.75), median BMI was 24.82 (IQR 22.43–26.87). Four patients (29%) smoked, one patient (7.1%) had diabetes mellitus, and five patients (36%) had an aneurysm of the abdominal aorta. All patients underwent elective open hernioplasty with mesh reinforcement. Three patients (21%) had a postoperative complication (two infections, one seroma). Recurrence rate was 7.1% (one patient).
Conclusions
This series describes 14 patients with a median follow-up of 50 months and a recurrence rate of 7.1%. The low recurrence rate could be explained by the use of large meshes that reinforce the entire midline to compensate for the reduced collagen strength in EDS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incisional hernia formation is one of the most frequent complications after abdominal surgery with midline laparotomy, occurring in 11–20% of all laparotomies in the general population [1]. When patients have risk factors (obesity, smoking or abdominal aortic aneurysm), this rate can increase up to 35% [2].
It is hypothesized that a disturbed balance between mature and immature collagen can be part of the underlying mechanism leading to incisional hernia formation. Klinge et al. explain recurrent hernia formation as a combined problem of biology and technique [3]. The human extracellular matrix consists of twenty different types of collagen, of which 95% is type I and III collagen [4]. Patients with recurrent ventral hernias have a decreased collagen I/III ratio. Collagen type I is mature, mechanically stable collagen, whereas collagen type III is immature, mechanically instable collagen [3]. Alongside the previously mentioned collagens, it has been hypothesized by Schumpelick et al. that tenascin, a family of glycoproteins, could be linked to hernia formation [5]. Given this mechanism, patients with an underlying connective tissue disease, such as Ehlers-Danlos syndrome (EDS), can be at risk for a higher recurrence rate after both ventral and incisional hernia repair [5,6,7]. EDS was first described in 1901 and the syndrome characterizes itself by a triad of skin hyperextensibility, joint hypermobility, and tissue fragility. Originally, EDS was divided into numbered subtypes. In 1998, the Villefranche classification scheme divided EDS into six subtypes, based on clinical features, biochemical and genetic findings, and mechanism of inherence: classic (type I and II), hypermobility (type III), vascular (type IV), kyphoscoliosis (type VI), arthrochalasia (type VIIA and VIIB), and dermatosparaxis (type VIIC) [8, 9]. Because of overlapping symptoms in these different subtypes, categorizing EDS is no easy task. Including all subtypes of EDS, the incidence is approximately one in 5000 people, of which the hypermobility subtype is most common [8].
The recently published international classification of the Ehlers-Danlos Syndrome describes the genetic basis for each type of EDS. The classical, vascular, and arthrochalasia types have been linked to either type I or type III collagen disorders [4, 10]. The hypermobility type is linked to tenascin X alterations. Although not all types of EDS have been linked to a specific protein disorder, many surgeons fear a high recurrence rate following hernia repair in EDS patients because of similar collagen disorders associated with both EDS and hernia recurrence [5,6,7].
EDS can potentially influence every part of the body where connective tissue is present. The literature on the relationship between EDS and hernia development is scarce and only includes a few case reports. Despite the lack of evidence, many surgeons believe that EDS may have a negative effect on the clinical outcome of ventral hernioplasty in terms of both higher postoperative complication and recurrence rates. The aim of this retrospective case series is to evaluate outcomes of ventral hernioplasty in patients with Ehlers-Danlos syndrome, the primary outcome is hernia recurrence and the secondary outcome is postoperative complications.
Methods
A retrospective analysis of hospital registries between January 2000 and January 2017 was performed in a large university hospital in Ghent, Belgium (Ghent University Hospital). Before commencement of the study, ethical approval and approval of the Institutional Review Boards was obtained. The hospital central registry was searched using either ICD-10/ICD-9-CM or Diagnosis Treatment Codes (DBC) for collagen disorder (Q79.6/756.83) and ‘hernioplasty’ (0303.123/0303.124). Any patient with a history of EDS (any type) and a ventral abdominal hernioplasty was eligible for inclusion in this study. Patients who registered an objection for participation in scientific research in their medical chart were excluded. Follow-up was obtained from patients’ medical charts. All EDS patients were seen 3 weeks postoperatively, as well as every 6 months hereafter.
Data collection
The following data were extracted from patients medical charts: baseline characteristics (age, sex, body mass index (BMI), smoking, medical history and type of Ehlers-Danlos), information about the hernia (date of diagnosis, type of hernia, size, primary/recurrent hernia, complaints), details regarding the surgical procedure (date of operation, elective/emergency procedure, type of procedure, mesh type and size and drain placement), postoperative data (postoperative complications (seroma, hematoma, surgical site infection, other infection, mesh explantation, and recurrence)), and follow-up (duration, number of outpatient clinic visits, readmissions, reoperations, and complaints). Hernia characteristics were reported using the European Hernia Classification of the European Hernia Society (EHS) [11]. All data were stored and analyzed in SPSS® for windows version 24, IBM corp. Armonk, NY, released 2013.
Results
A total of 14 patients (seven males, seven females), with a median age of 45 years (range 24–60 years) were included with diagnosis dates between June 2009 and July 2016. Median BMI was 24.82 (IQR 22.43–26.87). Four patients smoked (29%), one patient (7.1%) had diabetes mellitus, and five patients (36%) had an aneurysm of the abdominal aorta. Ten patients (71%) were ASA Class II and three patients (21%) were ASA Class III.
Two patients (7.1%) had the classic type Ehlers-Danlos, six patients (43%) had the hypermobility type, and four patients (29%) had the vascular type. Patient baseline characteristics are shown in Table 1.
Hernia characteristics
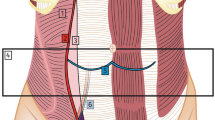
Ten patients (71%) had an incisional hernia and four patients (29%) had a primary hernia (see Fig. 1 for hernia characteristics). One of the incisional hernias was a recurrent hernia, previously treated with a Marlex® mesh. The median hernia length of the primary hernias was 2.5 cm (range 2.0–5.0 cm), and the median width was 2.0 cm (range 1.5–3.0 cm). The median hernia length of the incisional hernias was 5.0 cm (range 0.6–25 cm), and the median width was 3.5 cm (range 0.8–15 cm). None of the patients underwent any concomitant procedures, nor had they concomitant hernias in other locations.
Hernia characteristics. Hernia characteristics of all included patients. Characteristics are reported according to the European Hernia Society (EHS) guidelines for hernia classification. Width for incisional hernias (W1 = < 4 cm; W2 ≥ 4–10 cm; W3 ≥ 10 cm), width for primary hernias (W1 < 2 cm; W2 ≥ 2–4 cm; W3 ≥ 4 cm)
Surgical characteristics
All hernia repair procedures were elective (see Table 2 for operation details). In all patients, open surgery was performed, one procedure (a recurrent hernia repair) was planned as a laparoscopic procedure, but converted into an open procedure because of severe adhesions in the abdominal cavity. All patients received mesh reinforcement in either onlay (n = 1, 7%), sublay (n = 9, 64%), preperitoneal (n = 3, 21%), or intraperitoneal (n = 1, 7%) position. The onlay procedure was performed using an Adhesix® mesh, sublay repairs were performed with UltraPro® (n = 7), Adhesix® (n = 1), or Rebound® (n = 1) mesh. Preperitoneal repairs were performed using the Ultrapro® (n = 1, 33%), or Rebound® (n = 2, 67%) mesh, and the intraperitoneal procedure was performed using a Dualmesh®. Average mesh size was 399 cm2 (range 63–900 cm2), with an average length of 23 cm (range 7.0–35 cm), and width of 16 cm (range 8.0–30 cm). All sublay repairs could be closed in the midline using the Rives-Stoppa technique without the need for additional procedures (component separation or other). Eleven patients (79%) received a drain at the end of the procedure.
Perioperative outcomes
No intra-operative complications were recorded. Postoperative complications occurred in three patients (21%) (Table 3). Mean hospital stay was 3.4 days (± 1.04 days). One patient (7%) had a seroma and two patients (14%) had a surgical site infection. One of the patients with a surgical site infection had a BMI of 30.4 kg/m2; the other patient had a relatively large hernia (25 × 15 cm). One of the patients with a surgical site infection required antibiotic treatment and was, therefore, classified as a Clavien-Dindo Grade II complication [12]. The remaining two complications were Grade I. No other complications were recorded in the 30-day postoperative period.
Long-term outcomes
Median follow-up after surgery was 50 months (IQR 18–82, range 6–152 months). Patients visited the outpatient clinic a mean of three times (range 1–4 times). During this follow-up period, recurrences were assessed using clinical examination (n = 3, 29%), or clinical examination combined with ultrasonography (n = 10, 71%). One patient (7%) developed a hernia recurrence diagnosed by clinical examination. This patient was a 37-year-old female with EDS type III without relevant comorbidity or medical history (no diabetes, no aortic aneurysm, no smoking). The patient’s BMI was 25.7. She presented with a primary umbilical hernia of 2 × 2 cm (EHS Primary Abdominal wall Hernia Class: Midline Epigastric Medium hernia). She underwent an elective open repair with a preperitoneal mesh placement (Rebound® 9 × 8 cm) in August 2009. The procedure was without any complication. She developed a clinical recurrence after approximately 24-month follow-up, which resulted in esthetic complaints. The patient did not seek medical attention for her recurrence until 89-month follow-up, as she does not wish to undergo reoperation for the recurrence. No readmissions were performed. During follow-up, one patient died due to brain hemorrhage, unrelated to the hernioplasty procedure. For this patient, no long-term follow-up was available.
Discussion
This case series of 14 patients with Ehlers-Danlos syndrome (EDS) undergoing ventral hernia repair shows a 7.1% recurrence rate after a median follow-up period of 50 months. Current literature on ventral hernioplasty in EDS patients is scarce with only a hand full of case reports. Girotto et al. describes two patients with EDS and recurrent ventral abdominal wall hernias [13]. He treated these patients with a components separation technique and an onlay Marlex® mesh. Follow-up in this study is not described clearly. Fogel et al. describes a series of six ventral hernia repairs, of which two patients got a recurrent hernia, though important details regarding the surgical procedure and follow-up are not described as the focus of the article is on EDS and not on ventral hernia repair.
The current series is the first study that looks at patients with EDS as a specific risk group for developing hernia recurrence. Even though the detailed pathophysiology of incisional hernia formation is still illusive, many factors influence surgical wound healing and ultimately hernia formation [14]. One important factor is collagen synthesis and maturation. Given the well-established collagen impairment in EDS patients, a high recurrence rate in this population was anticipated. However, the 7% recurrence rate after open mesh repair in this study is lower than the 12% found in literature in the general patient population after elective open ventral hernioplasty with mesh reinforcement, after a median follow-up of 59 months [15]. The low recurrence rate can potentially be explained by the large mesh size. The average mesh size in this series was 16 × 23 cm, for an average hernia size of 3 × 5 cm. The ‘oversized’ mesh ensured a large surface for tissue ingrowth, which could compensate for the reduced collagen quality. Additionally, all patients were known to be diagnosed with EDS preoperatively. This might lead to a higher awareness of the surgeon. More conservative choices could have been made and more attention to the suturing technique could have been given. These factors, however, are hard to objectify.
During the 17-year inclusion period of this consecutive case series, only 14 patients were identified. There are several explanations for the relatively low number of EDS patients with ventral hernias. The most obvious one would be the low prevalence of EDS (1:5000). Another, more troubling, explanation would be identification failure of EDS in the outpatient hernia clinic. Since this case series is one of the first articles to discuss the potential influence of EDS on ventral hernia surgery outcomes, the problem may be underestimated or overlooked. Since EDS may be ‘diagnosed’ by one of many physicians either inside, or outside the hospital, central hospital registries may not always be up-to-date concerning the patient history. Hence, the treating physician must actively acquire information regarding EDS symptoms to not overlook the disease in the outpatient hernia clinic.
Limitations
A retrospective case series is methodologically unsuitable to determine the recurrence rate of ventral hernias in EDS patients accurately; hence, the percentages reported in this series must be interpreted with caution. Furthermore, because of the small sample size, detailed analysis of the relations between different types of EDS and clinical outcomes could not be made. Additionally, only two of the fourteen patients (14%) had the classic EDS type. Although no in-depth analyses exist on the different subtypes of EDS and hernia recurrence, it could be hypothesized that the classic type would be more prone to recurrence than other types. This could partially explain the relatively low recurrence rate found in this study.
Finally, some patients had a relatively short follow-up period. This could potentially lead to an underreported recurrence rate.
Despite the abovementioned limitation, it is the authors’ opinion that the following conclusions can be made based on the results of this article.
Recommendations for hernioplasty in EDS patients
-
Establishing the diagnosis Ehlers-Danlos syndrome is the first step in providing tailored care for this complex patient population. If the family history or physical examination suggests Ehlers-Danlos syndrome, further examination is advised before attempting ventral abdominal wall hernioplasty.
-
Treat ‘small’ ventral abdominal wall hernias as if they were bigger. The patients described in this series presented with relatively ‘small’ ventral hernias, though they were treated with a large (oversized) mesh and an extensive repair (most often Rives-Stoppa) with reinforcement along the entire midline or previous incision. Using large meshes provides a large surface for tissue ingrowth, which could compensate for the collagen impairment in EDS patients.
Conclusion
Patients with EDS are prevalent in the ventral abdominal wall hernia population. Identifying these patients is the first step towards tailored care. This series describes 14 patients with a median follow-up of 50 months and a recurrence rate of 7.1% (one patient). The low recurrence rate observed in this series might be explained by the use of a large mesh and reinforcement of the entire midline to compensate for the reduced collagen strength in EDS.
References
Deerenberg EB, Harlaar JJ, Steyerberg EW, Lont HE, van Doorn HC, Heisterkamp J, Wijnhoven BP, Schouten WR, Cense HA, Stockmann HB, Berends FJ, Dijkhuizen FP, Dwarkasing RS, Jairam AP, van Ramshorst GH, Kleinrensink GJ, Jeekel J, Lange JF (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet 386(10000):1254–1260. https://doi.org/10.1016/s0140-6736(15)60459-7
Muysoms FE, Detry O, Vierendeels T, Huyghe M, Miserez M, Ruppert M, Tollens T, Defraigne JO, Berrevoet F (2016) Prevention of incisional hernias by prophylactic mesh-augmented reinforcement of midline laparotomies for abdominal aortic aneurysm treatment: a randomized controlled trial. Ann Surg 263(4):638–645. https://doi.org/10.1097/sla.0000000000001369
Klinge U, Binnebosel M, Rosch R, Mertens P (2006) Hernia recurrence as a problem of biology and collagen. J Minim Access Surg 2(3):151–154
Radu P, Bratucu M, Garofil D, Goleanu V, Popa F, Strambu V (2015) The role of collagen metabolism in the formation and relapse of incisional hernia. Chirurgia (Bucur) 110(3):224–230
Rosch R, Junge K, Knops M, Lynen P, Klinge U, Schumpelick V (2003) Analysis of collagen-interacting proteins in patients with incisional hernias. Langenbecks Arch Surg 387(11–12):427–432. https://doi.org/10.1007/s00423-002-0345-3
Henriksen NA (2016) Systemic and local collagen turnover in hernia patients. Dan Med J 63(7):7
Antoniou GA, Georgiadis GS, Antoniou SA, Granderath FA, Giannoukas AD, Lazarides MK (2011) Abdominal aortic aneurysm and abdominal wall hernia as manifestations of a connective tissue disorder. J Vasc Surg 54(4):1175–1181. https://doi.org/10.1016/j.jvs.2011.02.065
Beighton P, De Paepe A, Steinmann B, Tsipouras P, Wenstrup RJ (1998) Ehlers-Danlos syndromes: revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK). Am J Med Genet 77(1):31–37. https://doi.org/10.1136/ard.29.3.332
Callewaert B, Malfait F, Loeys B, De Paepe A (2008) Ehlers-Danlos syndromes and Marfan syndrome. Best Pract Res Clin Rheumatol 22(1):165–189. https://doi.org/10.1016/j.berh.2007.12.005
Malfait F, Francomano C, Byers P, Belmont J, Berglund B, Black J, Bloom L, Bowen JM, Brady AF, Burrows NP, Castori M, Cohen H, Colombi M, Demirdas S, De Backer J, De Paepe A, Fournel-Gigleux S, Frank M, Ghali N, Giunta C, Grahame R, Hakim A, Jeunemaitre X, Johnson D, Juul-Kristensen B, Kapferer-Seebacher I, Kazkaz H, Kosho T, Lavallee ME, Levy H, Mendoza-Londono R, Pepin M, Pope FM, Reinstein E, Robert L, Rohrbach M, Sanders L, Sobey GJ, Van Damme T, Vandersteen A, van Mourik C, Voermans N, Wheeldon N, Zschocke J, Tinkle B (2017) The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet 175(1):8–26. https://doi.org/10.1002/ajmg.c.31552
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RK, Simons MP, Smietanski M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414. https://doi.org/10.1007/s10029-009-0518-x
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Girotto JA, Malaisrie SC, Bulkely G, Manson PN (2000) Recurrent ventral herniation in Ehlers-Danlos syndrome. Plast Reconstr Surg 106(7):1520–1526
Franz MG (2008) The biology of Hernia formation. The Surgical clinics of North America 88(1):1–7. https://doi.org/10.1016/j.suc.2007.10.007
Kokotovic D, Bisgaard T, Helgstrand F (2016) Long-term recurrence and complications associated with elective incisional hernia repair. JAMA 316(15):1575–1582. https://doi.org/10.1001/jama.2016.15217
Acknowledgements
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
LK designed the study, analyzed and interpreted data and wrote the report. EM designed the study, analyzed and interpreted data and wrote the report. CR collected and interpreted data and revised the report. NB designed the study, interpreted data and wrote the report. JL designed the study, interpreted data and wrote the report. FB designed the study, interpreted data and wrote the report.
Corresponding author
Ethics declarations
Conflict of interest
LK, EM, CR, NB, JL, and FB declare that they have no conflict of interest.
Ethical approval
This study was approved by the local ethical committee.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of article informed consent is not required.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kroese, L.F., Mommers, E.H., Robbens, C. et al. Complications and recurrence rates of patients with Ehlers-Danlos syndrome undergoing ventral hernioplasty: a case series. Hernia 22, 611–616 (2018). https://doi.org/10.1007/s10029-018-1739-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1739-7