Abstract
Introduction
The aim of this systematic review is to establish the clinical impact of open (mesh and/or without mesh) and laparoscopic hernia repair (transabdominal pre-peritoneal (TAP) and/or totally extra-peritoneal (TEP)) on male fertility. The incidence of male infertility following various types of inguinal hernia repair is currently unknown. The lack of high-quality evidence has led to various speculations, suggestions and reliance on anecdotal experience in the clinical practice.
Methods
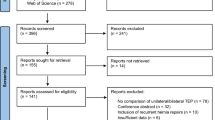
An electronic search of the literature in Medline, Scopus, Embase and Cochrane library from 1966 to October 2015 according to PRISMA checklist was conducted. Quality assessment of articles was conducted using the Oxford Critical Appraisal Skills Programme (CASP) and their recommendation for practice was examined through National Institute for Health and Care Excellence (NICE). This resulted in ten studies (n = 10), comprising 35,740 patients.
Results
Sperm motility could be affected following any type and/or technique of inguinal hernia repair but this is limited to the immediate postoperative period (≤48 h). Obstructive azoospermia was noted in 0.03% of open and 2.5% of bilateral laparoscopic (TAP) hernia repair with mesh. Male infertility was detected in 0.8% of the open hernia repair (mesh) with no correlation to the type of mesh (lightweight vs. heavyweight).
Conclusion
Inguinal hernia repair without mesh has no impact on male fertility and obstructive azoospermia. However, the use of mesh in bilateral open and/or laparoscopic repair may require the inclusion of male infertility as the part of informed consent in individuals that have not completed their family or currently under investigations.

Similar content being viewed by others
References
Jenkins JT, O’Dwyer PJ (2008) Inguinal hernias. BMJ 336(7638):269–272
Wantz EG (1984) Complications of inguinal hernia repair. Surg Clin North Am 64(2):287–298
The International Committee for Monitoring Assisted Reproductive Technology (ICMART) (2009) The World Health Organization (WHO) Revised Glossary on ART Terminology
Moher D, Liberati A, Tetzlaff J et al (2009) PRISMA group preferred reporting items for systematic reviews and meta analysis: the PRISMA statement. J clin Epidemol 62(10):1006–1012
CASP critical Appraisal Skills Programme OXFORD UK found at: http://media.wix.com/ugd/dded87_e37a4ab637fe46a0869f9f977dacf134.pdf
Weightman A, Ellis I, Cullum A et al. (2006) Grading evidence and recommendation for public health interventions: developing ad piloting a framework. http://www.nice.org.uk/guidance/ph1/resources/methodsfor-development-of-nice-public-health-guidance2
Schafer M (2011) Bilateral endoscopic total extraperitoneal (TEP) inguinal hernia repair does not induce obstructive azoospermia: data of a retrospective and prospective trial. World J Surg 35:1649–1650
Brendsen FH, Bjursten LM, Simanaitis M et al (2004) Does mesh implantation affect the spermatic cord structure after inguinal hernia surgery? Eur Surg Res 36:318–322
Uzzo RG, Lemack GE, Morrissey KP et al (1999) The effect of mesh bioprosthesis on the spermatic cord structures: a preliminary report in canine model. J Urol 161:1344–1349
Shah NR, Mikami DJ, Cook C et al. (2011) A comparison of outcomes between open and laparoscopic surgical repair of recurrent inguinal hernias. Surg Endosc 25(7):2330–2337
Perko Z, Rakic M, Pogorelic Z et al (2011) Laparoscopic trans abdominal preperitoneal approach for inguinal hernia repair: a five year experience at a single center. Surg Today 41:216–221
Stula I, Druzijanic N, Srsen D, Capkun V, Perko Z, Sapunar A et al (2012) Influence of inguinal hernia mesh repair on testicular flow and sperm autoimmunity. Hernia 16(4):417–424
Yavetz H, Harash B, Yogev L, Homonnai ZT, Paz G (1991) Fertility of men following inguinal hernia repair. Andrologia 23(6):443–446
Aydede H, Erhan Y, Sakarya A, Kara E, Ilkgul O, Can M (2003) Effect of mesh and its localisation on testicular flow and spermatogenesis in patients with groin hernia. Acta Chir Belg 103(6):607–610
Peeters E, Spiessens C, Oyen R, De Wever L, Vandeschueren D, Penninckx F et al (2014) Sperm motility after laparoscopic inguinal hernia with lightweight meshes: 3 year follow up of a randomised clinical trial. Hernia 18:361–367
Shin D, Lipshultz LI, Goldstein M, Barme GA, Fuchs EF, Nagler HM et al (2005) Herniorrhaphy with polypropylene mesh causing inguinal vasal obstruction: a preventable cause of obstructive azoospermia. Ann Surg 241(4):553–558
Kiladze M, Gvenetadze T, Giorgobiani G (2009) Modified Lichtenshtein hernioplasty prevents male infertility. Ann Ital Chir 80(4):305–309
Skawran S, Weyhe D, Schmitz B, Belyaev O, Bauer KH (2011) Bilateral endoscopic total extraperitoneal (TEP) inguinal hernia repair does not induce obstructive azoospermia: data of a retrospective and prospective trial. World J Surg 35(7):1643–1648
Hallen M, Sandblom G, Nordin P, Gunnarsson U, Kvist U, Westerdahl J (2011) Male infertility after mesh hernia repair: a prospective study. Surgery 149(2):179–184
Hallen M, Westerdahl J, Nordin P, Gunnarsson U, Sandblom G (2012) Mesh hernia repair and male infertility: a retrospective register study. Surgery 151(1):94–98
Stula I, Druzijanic N, Sapunar A, Perko Z, Bosnjak N, Kraljevic D (2014) Antisperm antibodies and testicular blood flow after inguinal hernia mesh repair. Surg Endosc 28(12):3413–3420
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AK declares no conflict of interest. ML declares no conflict of interest. NVR declares no conflict of interest.
Funding
None.
Ethical approval
Not applicable.
Rights and permissions
About this article
Cite this article
Kordzadeh, A., Liu, M.O. & Jayanthi, N.V. Male infertility following inguinal hernia repair: a systematic review and pooled analysis. Hernia 21, 1–7 (2017). https://doi.org/10.1007/s10029-016-1560-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1560-0