Abstract
Introduction
The purpose of this study is to compare the tissue incorporation of a novel fenestrated and non-fenestrated crosslinked porcine dermal matrix (CPDM) (CollaMend™, Davol Inc., Warwick, RI) in a porcine model of ventral hernia repair.
Methods
Bilateral abdominal wall defects were created in 12 Yucatan minipigs and repaired with a preperitoneal or intraperitoneal technique 21 days after hernia creation. Animals were randomized to fenestrated or non-fenestrated CPDM for n = 6 pieces of each graft in the preperitoneal or intraperitoneal location. All animals were sacrificed at 1 month. Adhesion characteristics and graft contraction/growth were measured by the Garrard adhesion grading scale and transparent grid overlay. Histological analysis of hematoxylin and eosin (H&E)-stained slides was performed to assess graft incorporation. Tissue incorporation strength was measured by a T-peel tensile test. The strength of explanted CPDM alone and de novo CPDM was measured by a uniaxial tensile test using a tensiometer (Instron, Norwood, MA) at a displacement rate of 0.42 mm/s. Statistical significance (P < 0.05) was determined for histological analysis using a Kruskal–Wallis non-parametric test with a Bonferroni correction, and for all other analyses using a two-way analysis of variance (ANOVA) with a Bonferroni post-test or a Kruskal–Wallis non-parametric test with a Dunn’s post-test.
Results
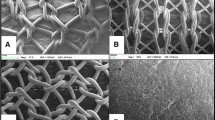
Intraperitoneal placement of fenestrated CPDM resulted in a significantly higher area of adhesions and adhesion score compared to the preperitoneal placement of fenestrated CPDM (P < 0.05). For both preperitoneal and intraperitoneal placement, histological findings demonstrated greater incorporation of the graft due to the fenestrations. No significant differences were detected in the uniaxial tensile strengths of the graft materials alone, either due to the graft type (non-fenestrated vs. fenestrated) or due to the placement location (preperitoneal vs. intraperitoneal). The incorporation strength (T-peel force) was significantly greater for fenestrated compared to non-fenestrated CPDM when placed in the preperitoneal location (P < 0.01). The incorporation strength was also significantly greater for fenestrated CPDM placed in the preperitoneal location compared to fenestrated CPDM placed in the intraperitoneal location (P < 0.05).
Conclusions
Fenestrations in CPDM result in greater tissue incorporation strength and lower adhesion area and score when placed in the preperitoneal location. Fenestrations in CPDM allow for greater tissue incorporation without accelerating graft degradation. Fenestrations may be placed in CPDM while still allowing adequate graft strength for intraperitoneal and preperitoneal hernia repairs at 1 month in a porcine model.











Similar content being viewed by others
References
Stone HH, Fabian TC, Turkleson ML, Jurkiewicz MJ (1981) Management of acute full-thickness losses of the abdominal wall. Ann Surg 193(5):612–618
Mathes SJ, Stone HH (1975) Acute traumatic losses of abdominal wall substance. J Trauma 15(5):386–391
Szczerba SR, Dumanian GA (2003) Definitive surgical treatment of infected or exposed ventral hernia mesh. Ann Surg 237(3):437–441
Mathes SJ, Steinwald PM, Foster RD, Hoffman WY, Anthony JP (2000) Complex abdominal wall reconstruction: a comparison of flap and mesh closure. Ann Surg 232(4):586–596
Parker DM, Armstrong PJ, Frizzi JD, North JH Jr (2006) Porcine dermal collagen (Permacol) for abdominal wall reconstruction. Curr Surg 63(4):255–258
Trabuco EC, Klingele CJ, Gebhart JB (2007) Xenograft use in reconstructive pelvic surgery: a review of the literature. Int Urogynecol J Pelvic Floor Dysfunct 18(5):555–563
Badylak S, Kokini K, Tullius B, Simmons-Byrd A, Morff R (2002) Morphologic study of small intestinal submucosa as a body wall repair device. J Surg Res 103:190–202
Gandhi S, Kubba LM, Abramov Y, Botros SM, Goldberg RP, Victor TA, Sand PK (2005) Histopathologic changes of porcine dermis xenografts for transvaginal suburethral slings. Am J Obstet Gynecol 192:1643–1648
Record RD, Hillegonds D, Simmons C, Tullius R, Rickey FA, Elmore D, Badylak SF (2001) In vivo degradation of 14C-labeled small intestinal submucosa (SIS) when used for urinary bladder repair. Biomaterials 22(19):2653–2659
Abolhoda A, Yu S, Oyarzun JR, McCormick JR, Bogden JD, Gabbay S (1996) Calcification of bovine pericardium: glutaraldehyde versus No-React biomodification. Ann Thorac Surg 62:169–174
Courtman DW, Errett BF, Wilson GJ (2001) The role of crosslinking in modification of the immune response elicited against xenogenic vascular acellular matrices. J Biomed Mater Res 55:576–586
Taylor DF (1972) Porosity in silver-tin amalgams. J Biomed Mater Res 6:289–304
Wilkins ES (1991) Tissue reaction to intraperitoneally implanted catheter materials. J Biomed Eng 13:173–175
Wake MC, Patrick CW Jr, Mikos AG (1994) Pore morphology effects on the fibrovascular tissue growth in porous polymer substrates. Cell Transplant 3:339–343
Bezuidenhout D, Davies N, Zilla P (2002) Effect of well defined dodecahedral porosity on inflammation and angiogenesis. ASAIOJ 48:465–471
Matthews BD, Pratt BL, Pollinger HS, Backus CL, Kercher KW, Sing RF, Heniford BT (2003) Assessment of adhesion formation to intra-abdominal polypropylene mesh and polytetrafluoroethylene mesh. J Surg Res 114:126–132
Otterburn D, Losken A (2009) The use of porcine acellular dermal material for TRAM flap donor-site closure. Plast Reconstr Surg 123(2):74e–76e
Garrard CL, Clements RH, Nanney L, Davidson JM, Richards WO (1999) Adhesion formation is reduced after laparoscopic surgery. Surg Endosc 13(1):10–13
Valentin JE, Badylak JS, McCabe GP, Badylak SF (2006) Extracellular matrix bioscaffolds for orthopaedic applications. A comparative histologic study. J Bone Joint Surg Am 88(12):2673–2686
Cobb WS, Harris JB, Lokey JS, McGill ES, Klove KL (2003) Incisional herniorrhaphy with intraperitoneal composite mesh: a report of 95 cases. Am Surg 69(9):784–787
Voyles CR, Richardson JD, Bland KI, Tobin GR, Flint LM, Polk HC Jr (1981) Emergency abdominal wall reconstruction with polypropylene mesh: short-term benefits versus long-term complications. Ann Surg 194(2):219–223
Karakousis CP, Volpe C, Tanski J, Colby ED, Winston J, Driscoll DL (1995) Use of a mesh for musculoaponeurotic defects of the abdominal wall in cancer surgery and the risk of bowel fistulas. J Am Coll Surg 181(1):11–16
Mayberry JC, Burgess EA, Goldman RK, Pearson TE, Brand D, Mullins RJ (2004) Enterocutaneous fistula and ventral hernia after absorbable mesh prosthesis closure for trauma: the plain truth. J Trauma 57(1):157–162 (discussion 163–163)
Tremblay LN, Feliciano DV, Schmidt J, Cava RA, Tchorz KM, Ingram WL, Salomone JP, Nicholas JM, Rozycki GS (2001) Skin only or silo closure in the critically ill patient with an open abdomen. Am J Surg 182(6):670–675
Hiles M, Record Ritchie RD, Altizer AM (2009) Are biologic grafts effective for hernia repair?: a systematic review of the literature. Surg Innov 16(1):26–37
Diaz JJ Jr, Conquest AM, Ferzoco SJ, Vargo D, Miller P, Wu YC, Donahue R (2009) Multi-institutional experience using human acellular dermal matrix for ventral hernia repair in a compromised surgical field. Arch Surg 144(3):209–215
Cobb GA, Shaffer J (2005) Cross-linked acellular porcine dermal collagen implant in laparoscopic ventral hernia repair: case-controlled study of operative variables and early complications. Int Surg 90(3 Suppl):S24–S29
Misra S, Raj PK, Tarr SM, Treat RC (2008) Results of AlloDerm use in abdominal hernia repair. Hernia 12(3):247–250
Sandor M, Xu H, Connor J, Lombardi J, Harper JR, Silverman RP, McQuillan DJ (2008) Host response to implanted porcine-derived biologic materials in a primate model of abdominal wall repair. Tissue Eng Part A 14(12):2021–2031
Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Ottinger AP, Schumpelick V (1998) Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg 164:951–960
Acknowledgments
We would like to acknowledge the efforts of Michael Brodt M.S., Department of Orthopedic Surgery, Washington University School of Medicine, St. Louis, Missouri, USA, for the mechanical testing of the 1 month uniaxial and T-peel samples. Experiments were funded by a research grant from Davol Inc. (Warwick, RI).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jenkins, E.D., Melman, L., Deeken, C.R. et al. Evaluation of fenestrated and non-fenestrated biologic grafts in a porcine model of mature ventral incisional hernia repair. Hernia 14, 599–610 (2010). https://doi.org/10.1007/s10029-010-0684-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-010-0684-x