Abstract
Background
The patient’s own repair of a body wall defect would be enhanced by a mechanically robust, physically tailorable, bioresorbable mesh scaffold that: (1) supports rapid host tissue ingrowth and development, while (2) reducing the complications associated with permanent synthetic and allogenic and xenogenic biological implants.
Methods
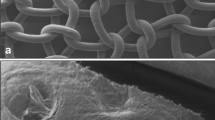
A full-thickness 1-cm-diameter abdominal wall defect was made in 36 Sprague–Dawley rats, which were divided according to the implant material used; SeriFascia surgical mesh (test) and Mersilene mesh (control). Histopathology, histomorphometry, tissue ingrowth, and biomechanical analysis were performed 30 and 94 days post-implantation.
Results
The biological response to the test and control groups were equivalent, with significantly greater tissue ingrowth observed in the test group (P < 0.05). A significant 33 and 57% reduction of test device mass was observed at 30 and 94 days, respectively. The ultimate burst load for the test group defect decreased after 30 days to the initial strength of the control mesh and remained constant for the duration of the study.
Conclusion
SeriFascia surgical mesh initially bioresorbed at an ideal rate that supported the transfer of load-bearing responsibility to developing host repair tissue. The results indicate the development of functional native tissue that could potentially minimize any long-term complication associated with presently available mesh implants.








Similar content being viewed by others
References
Badylak S, Kokini K, Tullius B, Simmons-Byrd A, Morff R (2002) Morphologic study of small intestinal submucosa as a body wall repair device. J Surg Res 103:190–202
Cosson M, Debodinance P, Boukerrou M, Chauvet MP, Lobry P, Crépin G, Ego A (2003) Mechanical properties of synthetic implants used in the repair of prolapse and urinary incontinence in women: which is the ideal material? Int Urogynecol J Pelvic Floor Dysfunct 14:169–178
Dietz HP, Vancaillie P, Svehla M, Walsh W, Steensma AB, Vancaillie TG (2003) Mechanical properties of urogynecologic implant materials. Int Urogynecol J Pelvic Floor Dysfunct 14:239–243
Dikranian AH, Chang JH, Rhee EY, Aboseif SR (2004) The male perineal sling: comparison of sling materials. J Urol 172:608–610
Tyrell J, Silberman H, Chandrasoma P, Niland J, Shull J (1989) Absorbable versus permanent mesh in abdominal operations. Surg Gynecol Obstet 168:227–232
Alponat A, Lakshminarasappa SR, Teh M, Rajnakova A, Moochhala S, Goh PM, Chan ST (1997) Effects of physical barriers in prevention of adhesions: an incisional hernia model in rats. J Surg Res 68:126–132
Baptista ML, Bonsack ME, Felemovicius I, Delaney JP (2000) Abdominal adhesions to prosthetic mesh evaluated by laparoscopy and electron microscopy. J Am Coll Surg 190:271–280
Klinge U, Klosterhalfen B, Müller M, Schumpelick V (1999) Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg 165:665–673
Basoglu M, Yildirgan MI, Yilmaz I, Balik A, Celebi F, Atamanalp SS, Polat KY, Oren D (2004) Late complications of incisional hernias following prosthetic mesh repair. Acta Chir Belg 104:425–428
Vrijland WW, van den Tol MP, Luijendijk RW, Hop WC, Busschbach JJ, de Lange DC, van Geldere D, Rottier AB, Vegt PA, IJzermans JN, Jeekel J (2002) Randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg 89:293–297
Butler CE (2006) The role of bioprosthetics in abdominal wall reconstruction. Clin Plast Surg 33:199–211
Altman GH, Diaz F, Jakuba C, Calabro T, Horan RL, Chen J, Lu H, Richmond J, Kaplan DL (2003) Silk-based biomaterials. Biomaterials 24:401–416
Meinel L, Hofmann S, Karageorgiou V, Kirker-Head C, McCool J, Gronowicz G, Zichner L, Langer R, Vunjak-Novakovic G, Kaplan DL (2005) The inflammatory responses to silk films in vitro and in vivo. Biomaterials 26:147–155
Panilaitis B, Altman GH, Chen JS, Jin HJ, Karageorgiou V, Kaplan DL (2003) Macrophage responses to silk. Biomaterials 24:3079–3085
Chen JS, Altman GH, Karageorgiou V, Horan RL, Collette A, Volloch V, Colabro T, Kaplan DL (2003) Human bone marrow stromal cell and ligament fibroblast responses on RGD-modified silk fibers. J Biomed Mater Res A 67:559–570
Sofia S, McCarthy MB, Gronowicz G, Kaplan DL (2001) Functionalized silk-based biomaterials for bone formation. J Biomed Mater Res 54:139–148
Horan RL, Antle K, Collette AL, Wang Y, Huang J, Moreau JE, Volloch V, Kaplan DL, Altman GH (2005) In vitro degradation of silk fibroin. Biomaterials 26:3385–3393
Altman GH, Horan RL, Lu HH, Moreau J, Martin I, Richmond JC, Kaplan DL (2002) Silk matrix for tissue engineered anterior cruciate ligaments. Biomaterials 23:4131–4141
Junge K, Klinge U, Prescher A, Giboni P, Niewiera M, Schumpelick V (2001) Elasticity of the anterior abdominal wall and impact for reparation of incisional hernias using mesh implants. Hernia 5:113–118
Wolloscheck T, Gaumann A, Terzic A, Heintz A, Junginger T, Konerding MA (2004) Inguinal hernia: measurement of the biomechanics of the lower abdominal wall and the inguinal canal. Hernia 8:233–241
Cerise EJ, Busuttil RW, Craighead CC, Ogden WW 2nd (1975) The use of Mersilene Mesh in repair of abdominal wall hernias: a clinical and experimental study. Ann Surg 181:728–734
Zhang F, Zhang J, Lin SY, Oswald T, Sones W, Cai Z, Dorsett-Martin W, Lineaweaver WC (2003) Small intestinal submucosa in abdominal wall repair after TRAM flap harvesting in a rat model. Plast Reconstr Surg 112:565–570
National Research Council (1996) Guide for the care and use of laboratory animals. National Academy Press, Washington, DC
Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Ottinger AP, Schumpelick V (1998) Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg 164:951–960
Klinge U, Schumpelick V, Klosterhalfen B (2001) Functional assessment and tissue response of short- and long-term absorbable surgical meshes. Biomaterials 22:1415–1424
Bos I, Johannisson R, Löhrs U, Lindner B, Seydel U (1990) Comparative investigations of regional lymph nodes and pseudocapsules after implantation of joint endoprostheses. Pathol Res Pract 186:707–716
Walker PS, Bullough PG (1973) The effects of friction and wear in artificial joints. Orthop Clin North Am 4:275–293
O’Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G (2005) Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg 92:166–170
Klosterhalfen B, Junge K, Klinge U (2005) The lightweight and large porous mesh concept for hernia repair. Expert Rev Med Devices 2:103–117
Ortiz-Oshiro E, Villalta GCL, Furió-Bacete V, Martínez JM, Ortega López D, Fdez-Represa JA (1999) Non-absorbable prosthetic meshes: which is the best option in the repair of abdominal wall defects? Int Surg 84:246–250
Acknowledgments
We gratefully acknowledge contributions from the following individuals: Enrico Mortarino for the mesh design and assistance with in-life mechanical analysis, Jason Prudom for assistance with the histomorphological analysis, Ivan Toponarski for time 0 mechanical analysis test execution, Adam Collette for assistance during the surgical implantation, and Rachel Pratt for assistance in manuscript preparation. We thank the National Institute of Standards and Technology (NIST, 70NANB4H3009) and Serica Technologies, Inc., for their support in this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horan, R.L., Bramono, D.S., Stanley, J.R.L. et al. Biological and biomechanical assessment of a long-term bioresorbable silk-derived surgical mesh in an abdominal body wall defect model. Hernia 13, 189–199 (2009). https://doi.org/10.1007/s10029-008-0459-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-008-0459-9