Abstract
Background
The Onze Lieve Vrouwe Gasthuis (OLVG) hospital is a large district teaching hospital with a residency programme for general surgery. Since 1998, inguinal hernia (IH) repairs in this hospital were performed according to the preliminary “evidence-based guidelines” concerning IH repair. The aim of this study was to analyse whether the use of the guidelines improves the quality of IH repair measured by a reduction of the operated recurrences, especially from the patients who underwent the previous repair in this hospital.
Methods
A retrospective study was performed which included all male adults (>18 years of age) undergoing IH surgery in the OLVG hospital for a primary or recurrent inguinal hernia from 1994 until 2004.
Results
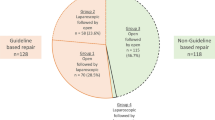
The use of mesh for primary hernia increased significantly from 0.6% in 1994 to 100% in 2004 (P < 0.001). The number of operations performed for recurrent IH fluctuated between 7% and almost 18%. However, the tendency towards a decrease in recurrence is clearly demonstrated by comparing the average recurrence rates of two time periods, namely, 1994–1998 (15.8%) and 2002–2004 (10.6%), proving a significant decrease (P < 0.002). The decreasing portion of recurrences previously operated in the study hospital from 64.3% (1994) to 14.3% (2004) was striking (P < 0.001). The prior operation performed before the recurrence was mesh-based in an average of 42/273 (15.4%) patients and increased each year.
Conclusions
Between 1994 and 2004, a significant increase in the use of mesh-based techniques for the treatment of IH, influenced by the Dutch evidence-based guidelines, probably resulted in a significant decrease in the number of operations performed for recurrent IH.
Similar content being viewed by others
References
Association of Surgeons of the Netherlands (2003) Guideline: treatment of the inguinal hernia (in Dutch). van Zuiden Communications B.V., Alphen aan den Rijn. ISBN: 90-8523-001-2
de Lange DH, Aufenacker TJ, Roest M, Simmermacher RK, Gouma DJ, Simons MP (2005) Inguinal hernia surgery in The Netherlands: a baseline study before the introduction of the Dutch Guidelines. Hernia 9:172–177
Aufenacker TJ, de Lange DH, Burg MD, Kuiken BW, Hensen EF, Schoots IG, Gouma DJ, Simons MP (2005) Hernia surgery changes in the Amsterdam region 1994–2001: decrease in operations for recurrent hernia. Hernia 9:46–50
Atkinson HDE, Nicol SG, Purkayastha S, Paterson-Brown S (2004) Surgical management of inguinal hernia: retrospective cohort study in southeastern Scotland, 1985–2001. BMJ 329:1315–1316
Wilkiemeyer M, Pappas TN, Giobbie-Hurder A, Itani KM, Jonasson O, Neumayer LA (2005) Does resident post graduate year influence the outcomes of inguinal hernia repair? Ann Surg 241:879–882
[No authors listed] (1999) Laparoscopic versus open repair of groin hernia: a randomised comparison. The MRC Laparoscopic Groin Hernia Trial Group. Lancet 354:185–190
Knook MTT, Weidema WF, Stassen LPS, Boelhouwer RU, van Steensel CJ (1999) Endoscopic totally extraperitoneal repair of bilateral inguinal hernias. Br J Surg 86:1312–1316
Grant AM; EU Hernia Trialists Collaboration (2002) Laparoscopic versus open groin hernia repair: meta-analysis of randomised trials based on individual patient data. Hernia 6:2–10
Vale L, Ludbrook A, Grant A (2003) Assessing the costs and consequences of laparoscopic vs. open methods of groin hernia repair: a systematic review. Surg Endosc 17:844–849
Kawji R, Feichter A, Fuchsjäger N, Kux M (1999) Postoperative pain and return to activity after five different types of inguinal herniorrhaphy. Hernia 3:31–35
Song D, Greilich NB, White PF, Watcha MF, Tongier WK (2000) Recovery profiles and costs of anesthesia for outpatient unilateral inguinal herniorrhaphy. Anesth Analg 91:876–881
Jarrett PE (2001) Day care surgery. Eur J Anaesthesiol Suppl 23:32–35
Prabhu A, Chung F (2001) Anaesthetic strategies towards developments in day care surgery. Eur J Anaesthesiol Suppl 23:36–42
Amid PK (2003) The Lichtenstein repair in 2002: an overview of causes of recurrence after Lichtenstein tension-free hernioplasty. Hernia 7:13–16
Amid PK (2004) Lichtenstein tension-free hernioplasty: its inception, evolution, and principles. Hernia 8:1–7
Bay-Nielsen M, Nordin P, Nilsson E, Kehlet H; Danish Hernia Data Base and the Swedish Hernia Data Base (2001) Operative findings in recurrent hernia after a Lichtenstein procedure. Am J Surg 182:134–136
Aasvang E, Kehlet H (2005) Surgical management of chronic pain after inguinal hernia repair. Br J Surg 92:795–801
Kehlet H, Bay-Nielsen M, Kingsnorth A (2002) Chronic postherniorrhaphy pain—a call for uniform assessment. Hernia 6:178–181
Acknowledgments
The authors thank the following participants for gathering the data in the previous years: B. van Dijkman, E.F. Hensen, B.W. Kuiken, I.G. Schoots, P.M. Vos.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aufenacker, T.J., Schmits, S.P., Gouma, D.J. et al. Do guidelines influence results in inguinal hernia treatment? A descriptive study of 2,535 hernia repairs in one teaching hospital from 1994 to 2004. Hernia 13, 35–39 (2009). https://doi.org/10.1007/s10029-008-0417-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-008-0417-6