Abstract
Capillary refill time (CRT) is an internationally accepted indicator of peripheral circulation. The CRT is measured by applying compression to the fingernail for a few seconds, releasing it, and observing the process of refilling of blood at the fingertip. The international guidelines for the management of sepsis and septic shock 2021 contains an additional new recommendation for CRT measurement to determine the peripheral circulation statuses of adult patients with septic shock. However, the current CRT measurement method lacks objectivity. Previous studies have reported the development of measurement devices and video analysis systems, which involve complex measurement environment construction and assume only in-hospital measurements. In addition, since medical workers are limited in the number of carrying medical devices, devices that can be used to obtain multiple biometric indicators in a single measurement are needed. Hence, a prototype wearable CRT measurement device was developed in this study, and its feasibility was evaluated by comparing the agreement, intra-class correlation coefficient, and coefficient of variation with those of a CRT measurement device developed in the past. The results indicated that mean CRTs between measurement methods were agreement, with moderate or better intra-rater reliability and no difference in coefficient of variation. Therefore, the results indicate the feasibility of the proposed wearable CRT device.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Capillary refill time (CRT) is an internationally accepted indicator of peripheral circulation; it is defined as the time required for a patient’s fingertip to recover to its original pre-compression color after pressure is applied to the nail fold for several seconds and released [1,2,3]. The international guidelines for the management of sepsis and septic shock 2021 contain an additional new recommendation for CRT measurement to determine the peripheral circulation statuses of adult patients with septic shock [4]. Furthermore, it has been reported to be useful for triage in emergency and disaster medicine [3, 5,6,7], the evaluation of dehydration in critically ill children [8], and the evaluation of skin valve condition in plastic surgery [9]. However, the current CRT measurement methods lack objectivity [10, 11]. To this end, previous studies have reported the development of measurement devices [12, 13] and video analysis systems [13, 14]; however, these methods involve complex constructions of the measurement environments and assume only in-hospital measurements. In addition, the development of devices that measure individual vital signs has resulted in an increase in the number of medical equipment as well as increased burden on medical workers. Thus, devices that can obtain multiple biometric indicators in a single measurement are needed.
To quantify CRT measurement, we developed a compression standardization device that mechanically and automatically compresses the fingertips and proposed optimal measurement conditions for CRT measurements [15]. We also developed a portable CRT measurement device with visual feedback function for inducing manual compression to optimal measurement conditions [16,17,18]. Using the portable CRT measurement device, we clarified the relationship between CRT and measurement position [17], and found that the device improved measurement stability over conventional visual CRT measurement [18].
Wearable electronics have achieved remarkable progress in recent years [19]. Monitoring systems have been developed to measure human respiration, pulse, and body movements continuously via highly elastic sensors affixed at multiple locations on the skin [20]. Thus, wearable electronics can obtain simultaneous measurements of multiple biometric data with reduced operator burden.
In this study, we develop a wearable device called the Medic Hand, which extends the functionality of a medical worker’s hand and can be used to measure multiple biometric indicators simultaneously without increasing the number of medical equipment. This study entails the development of a prototype of the Medic Hand for CRT measurement to investigate feasibility. We compare the variation, intra-rater reliability, and agreement of measurements between the proposed device and a portable CRT measurement device developed in the past [18].
2 Methods
2.1 Wearable CRT measurement device
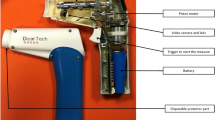
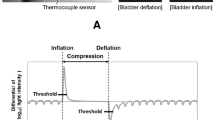
The prototype of the Medic Hand is shown in Fig. 1; it measures the nail bed color and provides visual feedback on the compression strength and time [18]. The measurement unit (Fig. 1a) comprises a force sensor, a color sensor, and an indenter that contacts the fingernail. The measured nail bed color, compression strength, and CRT are stored in an external memory (Micro SD) (Fig. 1b). Translucent bands printed using an optical 3D printer are used for attaching the measurement unit and cable to the hand (Fig. 1c). When measuring the CRT with Medic Hand, a microcontroller with a display is attached to the wrist, and the measurement unit is applied to the index finger. Medic Hand is used to measure the CRT via pinching the subject’s fingertip and by compression and release according to the feedback function (Figs. 2 and 3). The feedback function induces a compression strength of 3–7 N and compression time of 3 s or more, with the nail bed color being measured automatically. In this work, the target compression strength and compression time were set to 5 N and 3 s, respectively [15].
Prototype wearable CRT measurement device: Medic Hand. a The measurement unit for measuring compression strength and nail bed color. b The external memory (Micro SD) for storing measured nail bed color, compression strength, and CRT. c The translucent bands for attaching the measurement unit and cable to the hand
2.2 Portable CRT measurement device
We developed a portable device with the optimal measurement condition feedback function, as shown in Figs. 4 and 5 [18]. The portable device comprises visual feedback for the optimal CRT measurement conditions and a measurement function for the nail bed color. The operator manually presses and releases the subject’s fingertip in the manual method using the portable device with feedback function under the optimal conditions. In this work, the target compression strength and compression time were set to 5 N and 3 s, respectively [15].
2.3 Experimental protocol
The feasibility of Medic Hand was verified by comparing the agreement between the obtained measurement, coefficient of variation, and intra-rater reliability from the portable CRT measurement device (Figs. 4 and 5) [18]. The Institutional Review Board of Chiba University Graduate School of Medicine approved this experimental study (approval number: 4154). In the experiments with human subjects, consent was obtained from all participants. Eleven healthy adults in their 20 s participated as subjects (males: six people, females: five people). One non-medical worker in their 20 s participated as the operator of the Medic Hand and portable CRT measurement device. The operator placed each subject in a supine position. The operator then measured the CRT from the index finger of the left hand for each method.
Each measurement was performed according to the visual feedback function for compression strength and time (Fig. 3) [18]. Each measurement was obtained for five times for each method, and the subject’s fingertip was removed each measurement. The order of trials for each measurement was switched for each subject. The interval between compression release and the subsequent measurement was at 1 min.
2.4 Statistical analysis
We used eleven mean CRT data measured with the Medic Hand and eleven CRT data measured with the portable CRT measurement device for Bland–Altman analysis to evaluate the agreement (Table 1). We also used eleven mean CRT data and standard deviation (SD) measured with the Medic Hand and eleven mean CRT data and SD measured with the portable CRT measurement device for the coefficient of variation (CV) (Table 1). We used 55 CRT data measured with the Medic Hand and 55 CRT data measured with the portable CRT measurement device for the intra-class correlation coefficient (ICC). p < 0.05 was considered significant.
Statistical analyses were performed using R software version 4.2.2, tidyverse version 1.3.2, blandAltmanLeh version 0.3.1, and psych version 2.2.9 packages.
3 Results
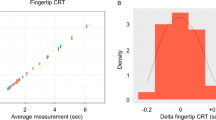
The Bland–Altman plots for the Medic Hand and portable CRT measurement device are shown in Fig. 6 [21]. The solid lines in Fig. 6 indicate the upper and lower permissible limits of agreement (LOA) for the measured values and the mean difference in measured values between the methods. The LOA ranges from 2.69 [95% CIs: 3.75 to 1.63] s to − 0.88 [95% CIs: 0.18 to –1.93] s. The mean difference in measured values between the methods is 0.91 [95% Confidence intervals (CIs): 1.52 to 0.30] s, with a fixed error (one-sample t test assuming zero population mean, p value = 0.0079). The Pearson’s correlation coefficient is –0.26, with no proportional error (Pearson's non-correlation test, p value = 0.45). Figure 6 shows that 11 out of the 11 data are within the acceptable limits of measurement values, thus indicating that the mean CRTs of the Medic Hand and portable CRT measurement device agree with each other.
For each measurement method, the CV was calculated from the mean and SD of the CRT measured five times for each subject. The CV is an indicator of the variation in CRT about the mean. The mean CV for Medic Hand was 0.32 ± 0.20 (mean ± SD) and that for the portable CRT measurement device was 0.24 ± 0.08. There was no difference in the coefficient of variation between Medic Hand and the portable CRT measurement device (Wilcoxon signed-rank test, p = 0.28).
To evaluate the intra-rater reliability of each measurement method, the corresponding ICC was calculated [22]. The portable CRT measurement device’s ICC (1, 5) was 0.92 [95% CIs: 0.97 to 0.80], and Medic Hand’s ICC (1, 5) was 0.60 [95% CIs: 0.88 to 0.065]. Each method showed moderate or better intra-rater reliability compared to the benchmarks noted by Landis et al. [23].
4 Discussion
The mean CRTs obtained with Medic Hand and the portable device show concordance in the Bland–Altman analysis. There is no difference in the coefficient of variation between Medic Hand and the portable device. Each measurement method showed moderate or better intra-rater reliability compared to the benchmarks of Landis et al. [23]. These results indicate the feasibility of Medic Hand. Compared with the portable CRT measurement device, Medic Hand is more difficult to use for compression and release, and this difficulty stems from the indenter made of polylactic acid resin, which slips on the fingernail. Hence, we need to consider a mechanism that prevents the indenter from slipping on the fingernail. In addition, because Medic Hand requires the sensor to continue remaining pinched after release to avoid floating off the nail, the mean compression strength of 0.45 ± 0.17 N (mean ± SD) is measured even after release; the corresponding value for the portable measuring device is 0.14 ± 0.10 N. The compression strength after release is, therefore, significantly different (Mann–Whitney U test, p value < 0.0001) and affect refilling of blood at the fingertip (Fig. 7). In fact, the Bland–Altman analysis showed a fixed error between the Medic Hand and the portable CRT measurement device (one-sample t test assuming zero population mean, p value = 0.0079). The CRT measured by the Medic Hand is longer than that measured by the portable CRT measurement device. The LOA ranges from 2.69 [95% CIs: 3.75 to 1.63] s to –0.88 [95% CIs: 0.18 to –1.93] s, which may affect triage in emergency and disaster medicine. Thus, to realize CRT measurement using Medic Hand in emergency and disaster medicine, we need to consider a solution where the sensor does not float from the fingernail after compression release. The hardware improvements to reduce the fixed error, software improvements are also needed, such as a simple method to subtract the fixed error calculated in this study from the measured values and a correction method to compensate for general fixed errors properly. Concrete methods will be the subject of future research.
The sensor part of the current Medic Hand prototype is thick in the ventral direction of the fingertip, which may interfere with medical procedures that require detailed work. Accordingly, we need to redesign the indenter with reduced thickness in the ventral direction of the fingertip. Another solution is to mount the sensor on the basal phalanx when CRT measurements are not performed, similar to a ring. In the future, we will consider usability improvements using technologies to convert rigid boards and electronic components to flexible ones [19, 20].
In this study, a single operator handles both the portable CRT measurement device and Medic Hand. The current prototype was intended to confirm the principle and feasibility, but the usability as a wearable device cannot be evaluated at present. The total measurement times of the portable device and Medic Hand, including consideration of the time required to switch from another task to the CRT measurement task, are not compared. Hence, we plan to further study the feasibility of and improvements to Medic Hand with more operators. In addition, subjects were limited to adults in their 20 s. Conditions that cause impaired peripheral circulatory status, such as sepsis and heat stroke, are not limited to older adults but also affect children and young adults. Thus, there is no contradiction in asking adults in their 20 s to cooperate as subjects. However, to accurately evaluate the feasibility of Medic Hand, it is necessary to measure CRT in a wide range of age groups rather than restricting the subjects to specific age groups. Therefore, we will design CRT measurement experiments for a wide range of age groups to assess the feasibility of the Medic Hand more accurately.
5 Conclusion
A prototype wearable CRT measurement device called the Medic Hand was developed in this study, and its feasibility was evaluated by comparing the agreement, intra-class correlation coefficient, and coefficient of variation with those of a CRT measurement device developed in the past. The results indicate the feasibility of the proposed wearable CRT device.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lima A, Bakker J (2005) Noninvasive monitoring of peripheral perfusion. Intensive Care Med 31:1316–1326
King D, Morton R, Bevan C (2013) How to use capillary refill time. Arch Dis Child Educ Pract Ed 99(3):111–116
Sansone CM, Prendin F, Giordano G et al (2017) Relationship between capillary refill time at triage and abnormal clinical condition: A prospective study. Open Nurs J 11:84–90
Evans L, Rhodes A, Alhazzani W et al (2021) Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Crit Care Med 49(11):e1063–e1143
Kumar N, Thomas N, Singhal D et al (2021) Triage score for severity of illness. Indian Pediatr 40(3):204–210
Horne S, Vassallo J, Read J et al (2013) UK triage–an improved tool for an evolving threat. Injury 44(1):23–28
Garner A, Lee A, Harrison K et al (2001) Comparative analysis of multiple-casualty incident triage algorithms. Ann Emerg Med 38(5):541–548
Canavan A, Arant BS Jr (2009) Diagnosis and management of dehydration in children. Am Fam Phys 80(7):692–696
Schiltz D, Geis S, Kehrer A et al (2017) Video tutorial for clinical flap-monitoring in plastic surgery. Plast Reconstr Surg Glob Open 5(10):e1478
Pickard A, Karlen W, Ansermino JM (2011) Capillary refill time: Is it still a useful clinical sign? Anesth Analg 113(1):120–123
Lewin J, Maconochie I (2008) Capillary refill time in adults. Emerg Med J 25:325–326
Blaxter LL, Morris DE, Crowe JA et al (2016) An automated quasi-continuous capillary refill timing device. Physiol Meas 37(1):83–99
Shinozaki K, Saeki K, Jacobson LS et al (2021) Evaluation of accuracy of capillary refill index with pneumatic fingertip compression. J Clin Monit Comput 35(1):135–145
John RT, Henricson J, Nilsson GE et al (2018) Reflectance spectroscopy: to shed new light on the capillary refill test. J Biophotonics 11(1):e201700043
Kawaguchi R, Nakada TA, Oshima T et al (2019) Optimal pressing strength and time for capillary refilling time. Crit Care 23(1):4
Shinozaki M, Nakada TA, Kawaguchi R et al (2019) Feedback function for capillary refilling time measurement device. Crit Care 23(1):295
Saito D, Nakada TA, Imaeda T et al (2022) Impact of posture on capillary refilling time. Am J Emerg Med 56:378–379
Shinozaki M, Shimizu R, Saito D et al (2022) Portable measurement device to quantitatively measure capillary refilling time. Artif Life Robot 27:48–57
Qiongfeng S, Bowei D, Tianyiyi H et al (2020) Progress in wearable electronics/photonics—Moving toward the era of artificial intelligence and internet of things. InfoMat 2(6):1131–1162
Niu S, Matsushita N, Beker L et al (2019) A wireless body area sensor network based on stretchable passive tags. Nat Electron 2:361–368
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 327(8476):307–310
Wastell DG, Geoffrey RB (1988) Intraclass correlations: A two-facet case study and some comments on the concept of reliability. Bull Psychon Soc 26:583–586
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Acknowledgements
This work was supported by the JSPS KAKENHI Grant Number JP 22J14138.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Taka-aki Nakada received executive compensation from Smart119 and held stock. Inc. Taka-aki Nakada has a patent related to CRT measurements. Yukihiro Nomura belongs to an endowment department sponsored by HIMEDIC Inc. and Siemens Healthcare K.K.; however, the status is irrelevant to the contents of the paper. The remaining authors have no other conflicts of interest related to this submission.
Institutional review board statement
The Institutional Review Board of Chiba University Graduate School of Medicine approved this experimental study (approval number 4154).
Informed consent statement
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Shinozaki, M., Saito, D., Nakada, Ta. et al. Feasibility study of wearable capillary refill time measurement device. Artif Life Robotics 29, 334–339 (2024). https://doi.org/10.1007/s10015-024-00936-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10015-024-00936-9