Abstract
Introduction
In severe TMJ ankylosis cases, the lack of growth of the mandible creates an anatomically narrow airway with a reduced pharyngeal airway space [PAS] which predisposes these patients towards obstructive apnoea [OSA]. There is evidence in the literature that such patients experience severe discomfort during physiotherapy if such airway abnormalities are not corrected prior to ankylosis release. This eventually leads to non-compliance towards physiotherapy and increases the risk of re-ankylosis.
Objective
In our study, pre-arthroplastic mandibular distraction osteogenesis [DO] was used to increase the PAS and resolve the underlying OSA prior to releasing the ankylosis.
Materials and methods
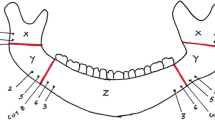
Twenty-five cases of TMJ ankylosis with micrognathia and OSA were included in this prospective observational sleep study. They were further divided into a paediatric group [14 subjects] and an adult group [11 subjects]. All cases presented with a history of onset of ankylosis during childhood [before the completion of craniofacial growth] as result of which there was a lack of forward growth of the mandible. Subjects included in our study underwent initial DO of the mandible followed by a second procedure for distractor removal and ankylosis release. Questionnaires, lateral cephalograms and sleep studies were taken pre-operatively (T0), immediate post-distraction to the desired length (T1) and 12 months post the distractor removal and ankylosis release (T2). The parameters studied were PAS width, apnoea hypopnea index [AHI], O2 saturation, mouth opening and mandibular advancement.
Results
The paediatric group variables were as follows: mean PAS width which increased from 3.5 mm [T0] to 9 mm [T2], mean AHI which decreased from 48.04 [T0] to 3.60 [T2], mouth opening which increased from 4.5 mm [T0] to 34 mm [T2] and mean O2 saturation which increased from 89.86% [T1] to 96.88% [T2]. The adult group variables were as follows: mean PAS width which increased from 5 mm [T0] to 11 mm [T2], mean AHI which decreased from 31.45 [T0] to 1.43 [T2], mouth opening which increased from 5 mm [T0] to 34 mm [T2] and mean O2 saturation which increased from 92.01% [T0] to 96.84% [T2]. Statistical analysis revealed that DO of the mandible significantly improved OSA by increasing the PAS which was evident by the lower AHI score. Mouth opening was also significantly improved post ankylosis release and maintained at the T2 interval. Ten subjects followed up beyond the T2 interval [mean 28 months post ankylosis release] and their data also revealed positive compliance towards physiotherapy, adequate mouth opening and maintenance of normal AHI.
Conclusion
Pre-arthroplastic mandibular DO has proved to be a successful modality for treatment of OSA in TMJ ankylosis patients with stable results at 12 months. By resolving the narrow airway and OSA, compliance towards physiotherapy was improved thus reducing the risk of re-ankylosis in the long term.






Similar content being viewed by others
References
Movahed R, Mercuri LG (2015) Management of Temporomandibular Joint Ankylosis. Oral Maxillofac Surg Clin North Am 27(1):27–35
Andrade NN, Kalra R, Shetye SP (2012) New protocol to prevent TMJ reankylosis and potentially life threatening complications in triad patients. Int J Oral Maxillofac Surg 41(12):1495–1500
Madani M, Madani F (2007 Sep) The pandemic of obesity and its relationship to sleep apnea. Atlas Oral Maxillofac Surg Clin North Am 15(2):81–88
Al-Moraissi EA, El-Sharkawy TM, Mounair RM, El-Ghareeb TI (2015) A systematic review and meta-analysis of the clinical outcomes for various surgical modalities in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg 44(4):470–482
Dimitroulis G (2011) A critical review of interpositional grafts following temporomandibular joint discectomy with an overview of the dermis-fat graft. Int J Oral Maxillofac Surg 40(6):561–568
Dehlink E, Tan H-L (2016) Update on paediatric obstructive sleep apnoea. J Thorac Dis 8(2):224–235
Madani M, Madani F (2007) Definitions, abbreviations, and acronyms of sleep apnea. Atlas Oral Maxillofac Surg Clin North Am 15(2):69–80
Spicuzza L, Caruso D, Di Maria G (2015) Obstructive sleep apnoea syndrome and its management. Ther Adv Chronic Dis 6(5):273–285
Ephros HD, Madani M, Geller BM, Defalco RJ (2007) Developing a protocol for the surgical management of snoring and obstructive sleep apnea. Atlas Oral Maxillofac Surg Clin North Am 15(2):89–100
Boyd SB (2009) Management of obstructive sleep apnea by maxillomandibular advancement. Oral Maxillofac Surg Clin North Am 21(4):447–457
Weaver TE, Sawyer A (2009) Management of obstructive sleep apnea by continuous positive airway pressure. Oral Maxillofac Surg Clin North Am 21(4):403–412
Bouchard C, Troulis MJ, Kaban LB (2009) Management of obstructive sleep apnea: role of distraction osteogenesis. Oral Maxillofac Surg Clin North Am 21(4):459–475
Wang X, Wang X-X, Liang C, Yi B, Lin Y, Li Z-L (2003) Distraction osteogenesis in correction of micrognathia accompanying obstructive sleep apnea syndrome. Plast Reconstr Surg 112(6):1549–1557 discussion 1558-9
Anantanarayanan P, Narayanan V, Manikandhan R, Kumar D (2008) Primary mandibular distraction for management of nocturnal desaturations secondary to temporomandibular joint (TMJ) ankylosis. Int J Pediatr Otorhinolaryngol 72(3):385–389
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics committee approval
Obtained from the Institutional Ethics Committee [EC/004/2011].
Informed consent
Obtained.
Rights and permissions
About this article
Cite this article
Andrade, N.N., Mathai, P.C., Ganapathy, S. et al. Pre-arthroplastic mandibular distraction osteogenesis for the correction of OSA in TMJ ankylosis: a prospective observational study of 25 cases. Oral Maxillofac Surg 22, 409–418 (2018). https://doi.org/10.1007/s10006-018-0722-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-018-0722-x