Abstract
Objectives
The root anatomy and position of mandibular third molars are important factors in assessing the level of difficulty of surgical removal procedures. In this light, this study aims to identify the most frequent position and the root anatomy of mandibular third molars.
Methods
The study sample comprised 1205 mandibular third molars from 710 panoramic radiographs evaluated. Regarding the position, all of them were based on Pell and Gregory’s and Winter’s classifications. The root anatomy was classified according to the type and number of roots, as well as the presence of laceration, fusion, or divergence. Gender and the quadrant were also considered. Following an interexaminer analysis, a statistical analysis was performed using the Kappa test.
Results
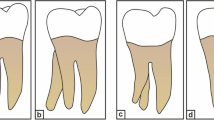
The results showed that the IA (40.3%) and mesioangular (53.8%) position was predominant in mandibular third molars. Regarding the anatomy, the most common were two roots (98.3%), of the conical simple type (88.9%), with absence of laceration (89.2%), divergence (84%), and fusion (80%).
Conclusion
The present study showed that the most prevalent mandibular third molar type in Brazilian patients was the IA and mesioangular position, with simple root anatomy. The result of this study can assist oral surgeons to better plan and assess the level of difficulty of surgical removal procedures.


Similar content being viewed by others
References
Winter GB (1926) Impacted mandibular third molars. Med Book Co, St. Louis
Pell GJ, Gregory GT (1933) Impacted mandibular third molars: classifications and modified technique for removal. Dent Digest 39:330–338
Yuasa H, Sugiura M (2004) Clinical postoperative findings after removal of impacted mandibular third molars: prediction of postoperative facial swelling and pain based on preoperative variables. Brit J Oral Maxillofac Surg 42:209–214
Susarla SM, Dodson TB (2005) Estimating third molar extraction difficulty: a comparison of subjective and objective factors. J Oral Maxillofac Surg 63:427–434
Almendros-Marques N, Alaejos-Algarra E, Quinteros-Borgarello M, Berini-Aytes L, Gay-Escoda C (2008) Factors influencing the prophylactic removal of asymptomatic impacted lower third molars. Int J Oral Maxillofac Surg 37:29–35
Akarslan ZZ, Kocabay C (2009) Assessment of the associated symptoms, pathologies, positions and angulations of bilateral occurring mandibular third molars: is there any similarity? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:26–32
Chiapasco M, De Cicco L, Marrone G (1993) Side effects and complications associated with third molar surgery. Oral Surg Oral Med Oral Pathol 76:412–420
Thangavelu A, Yoganandha R, Vaidhyanathan A (2012) Impact of impacted mandibular third molars in mandibular angle and condylar fractures. Int J Oral Maxillofac Surg 39:136–139
Polat HB, Ozan F, Kara I, Ozdemir H, Ay S (2008) Prevalence of commonly found pathoses associated with mandibular impacted third molars based on panoramic radiographs in Turkish population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:41–47
Pinto DG, Mockdeci HR, Almeida LE, Assis NMSP, Vilela EM (2015) Análise da prevalência e correlações por gênero, faixa etária, raça e classificação dos terceiros molares. HU Rev 41(3):155–162
Santos DR, Quesada GAT (2009) Prevalência de terceiros molares e suas respectivas posições segundo as classificações de Winter e de Pell e Gregory. Rev Cir Traumatol Buco-Maxilo-fac 9(1):83–92
Hattab FN, Ma’amon A, Rawadesh, Fahmy MS (1995) Impaction status of third molars in Jordanian students. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1:24–29
Venta I, Turtola L, Ylipaavalniemi P (2001) Radiographic follow-up of impacted third molars from age 20 to 32 years. Int J Oral Maxillofac Surg 30:54–57
Sandhu S, Kaur T (2005) Radiographic evaluation of the status of third molars in the Asian-Indian students. J Oral Maxillofac Surg 63:640–645
Genú PR, Vasconcelos BCE (2008) Influence of the tooth section technique in alveolar nerve damage after surgery of impacted lower third molars. Int J Oral Maxillofac Surg 37:923–928
Gomes ACA, Vasconcelos ECO, Silva EDO, Caldas AF Jr, Neto ICP (2008) Pantomography for prediction of nerve damage. J Oral Maxillofac Surg 66:256–259
Lübbers HT, Matthews F, Damerau G et al (2011) Anatomy of impacted lower third molars evaluated by computerized tomography: is there an indication for 3-dimensional imaging? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111:447–550
Better H, Abramovitz I, Shlomi B, Kahn A, Levy Y, Shaham A, Chaushu G (2004) The presurgical workup before third molar surgery: how much is enough? J Oral Maxillofac Surg 62:689–692
Carter K, Worthington S (2016) Predictors of third molar impaction: a systematic review and meta-analysis. J Dent Res 95(3):267–276
Patel S, Mansuri S, Shaikh F, Shah T (2017) Impacted mandibular third molars: a retrospective study of 1198 cases to assess indications for surgical removal, and correlation with age, sex and type of impaction—a single institutional experience. J Maxillofac Oral Surg 16(1):79–84
Lee et al (2015) Patients’ satisfaction and prevalence of complications on surgical extraction of third molar. Patient Prefer Adherence 9:257–263
Gulabivala K, Aung TH, Alavi A, Ng Y-L (2001) Root and canal morphology of Burmese mandibular molars. Int End J 34:359–370
Gulabivala K, Opasanon A, Ng Y-L, Alavi A (2002) Root and canal morphology of Thai mandibular molars. Int End J 35:56–62
Stephanie JS, West LA, Liewehr FR, Loushine RJ (2000) Root canal morphology of human maxillary and mandibular third molars. J Endod 26:675–678
Yuasa H, Kawai T, Sugiura M (2002) Classification of surgical difficulty in extracting impacted third molars. Br J Oral Maxillofac Surg 40:26–31
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Bell GW, Rodgers JM, Grime RJ, Edwards KL, Hahn MR, Dorman ML, Keen WD, Stewart DJC, Hampton N (2003) The accuracy of dental panoramic tomographs in determining the root morphology of mandibular third molar teeth before surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 95:119–125
Santamaria J, Artegoitia I (1997) Radiologic variables of clinical significance in the extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 84:469–473
Szalma J, Lemple E, Jeges S, Szabó G, Olasz L (2010) The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:294–302
Rood JP, Shehab AA (1990) The radiological predilection of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg 28:20–25
Maegawa H, Sano K, Kitagawa Y, Ogasawara T, Miyauchi K, Sekine J, Inokuchi T (2003) Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96:639–646
Monaco G, Montevecchi M, Bonetti GA, Gatto MR, Checchi L (2004) Reliablility of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc 135:312–318
Ohman A, Kivijarvi K, Blomback U, Flygare L (2006) Pre-operative radiographic evaluation of lower third molars with computed tomography. Dentomaxillofac Radiol 35:30–35
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional Bauru School of Dentistry research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
da Silva Sampieri, M.B., Viana, F.L.P., Cardoso, C.L. et al. Radiographic study of mandibular third molars: evaluation of the position and root anatomy in Brazilian population. Oral Maxillofac Surg 22, 163–168 (2018). https://doi.org/10.1007/s10006-018-0685-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-018-0685-y