Abstract
Low activity of the hypothalamic–pituitary–adrenal axis (HPAA) has been found in children with attention deficit hyperactivity disorder (ADHD). The condition may be related to the reduced attention regulation capacity and/or to comorbid oppositional defiant or conduct disorder (ODD/CD). Sex differences are probable but not sufficiently studied. We analyzed the HPAA activity and sympathetic nervous system reactivity (SR) in children with ADHD while accounting for ADHD symptom presentation, comorbidity, and sex differences. The sample comprised 205 children, 98 (61 boys, 37 girls) with ADHD and 107 (48 boys, 59 girls) healthy controls. DSM-5 phenotypic symptom presentation and comorbid ODD/CD were assessed using clinical interviews. Hair cortisol concentration (HCC) was used to assess the long-term, cumulative activity of the HPAA. SR was assessed via skin conductance response (SCR). For control purposes, comorbid internalizing symptoms and indicators of adverse childhood experiences (ACE) were assessed. Children were medication naive. Boys presenting with predominantly inattentive symptoms (ADHD-I) showed lower HCC than healthy boys. Girls presenting with combined symptoms (ADHD-C) showed higher HCC than did healthy girls (p’s < 0.05, sex-by-group interaction, F (2,194) = 4.09, p = 0.018). Boys with ADHD plus ODD/CD showed a blunted SR (p < 0.001, sex-by-group interaction, F (2,172) = 3.08, p = 0.048). Adjustment for ACE indicators led to non-significant differences in HCC but did not affect differences in SR. HCC constitutes an easily assessable, reliable, and valid marker of phenotypic ADHD-related features (i.e. symptom presentation and comorbidity). It indicates more homogenous subgroups of ADHD and might point to specifically involved pathophysiological processes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypothalamic–pituitary–adrenal-axis (HPAA) function has been extensively studied in attention deficit hyperactivity disorder (ADHD) and the broader domain of externalizing disorders (comprising e.g. oppositional defiant disorder (ODD) and conduct disorder (CD)), with meta-analyses of this research revealing a lower basal cortisol level (in serum and saliva samples) in children and adolescents with ADHD. However, considerable heterogeneity in the effects of individual studies has been found [1]. A meta-analysis by Kamradt et al. [2] summarized studies on cortisol reactivity to stress exposure. The authors reported that children/adolescents with ADHD did not differ from healthy controls, but again, heterogeneity was substantial. Reviews focusing on ODD/CD concluded that the blunted cortisol response sometimes observed in children/adolescents with ADHD is most likely due to the often comorbid ODD/CD [3, 4]. Research on HPAA function in ADHD has too seldom considered influences of comorbidity and other potential moderator variables such as past and present medication use, sex differences, phenotypic symptom presentation, and environmental conditions which might explain the observed heterogeneity.
ADHD is a highly heritable but heterogeneous disorder, with high variation in the phenotypic symptom presentation. Accordingly, the DSM-5 distinguishes between the presentation of predominantly inattentive symptoms, predominantly hyperactive/impulsive symptoms, and a combined presentation [5]. In about two-thirds of affected children, ADHD is accompanied by externalizing disorders (e.g. ODD and CD) and/or internalizing disorders (anxiety, depressive disorders) [6]. Moreover, considerable sex differences exist with regard to prevalence rates, symptom presentation, and comorbid disorders [7]. Given that HPAA function also differs between sexes [8], shows heritability [9] and adjusts to environmental conditions [10], and is related to neurocognitive and emotional functions (e.g. [11, 12]), it would be rather surprising to find a uniform pattern of HPAA dysregulation in children with ADHD.
Low HPAA activity and reactivity in externalizing disorders (i.e. ADHD, ODD, and CD) have been explained by different theoretical concepts focusing on low autonomic and cortical arousal (linked via the locus coeruleus and the brain norepinephrine system). Concepts emphasizing low anxiety and low responsivity to rewarding stimuli in externalizing disorders refer to low arousal as an aversive physiological state that the individual attempts to normalize (increase) by seeking sensation through impulsive, risky, and rule-breaking behaviors [13]. Low anxiety has been suggested to lead to inadequate social learning because children do not fear the negative consequences of their behaviors [14, 15]. Accordingly, low sympathetic reactivity (e.g. measured through the skin conductance) has consistently been found to be associated with ODD/CD [16]. Other concepts emphasize cognitive dysfunction and propose that low arousal in ADHD primarily reflects a reduced capacity to adjust activation to environmental demands [17, 18]. Inattention and poor executive functioning have been thought to result from too low and less-regulated energetic state [19]. As the autonomic nervous system and the HPA system adjust to environmental demands by coordinated, mutually supporting action [10], both concepts (i.e. ODD/CD-related low autonomic arousal/reactivity to emotional stimuli and attention deficit-related low capacity to adjust activation to cognitive demands) might explain a reduced HPAA activity. However, it is an open question whether ADHD-related low cortisol secretion actually associates with comorbid ODD/CD and/or attention deficits.
Previous research by our group provided support for the cognitive activation concept. We used the hair cortisol concentration (HCC) to assess the long-term, cumulative activity of the HPAA in medication-naïve 4–5-year-old children. The HCC has proven to validly capture the accumulated, integrated long-term activity of the HPAA [20,21,22]. Compared to blood and salivary cortisol measures, which reflect the cortisol secretion only at a single time point, HCC shows increased stability/reliability of measurement. The non-invasive procedure makes hair samples both independent form acute stress influences and well-acceptable for participating children [23].
We found that low HCC was associated with ADHD-inattentive symptoms in particular, as well as with poor working memory performance [24, 25]. Moreover, HCC at the age of 4–5 years predicted ADHD development by the age of 8 years [26]. These links were more pronounced in boys than in girls or referred exclusively to boys, and the results remained unchanged after controlling for comorbid symptoms of ODD/CD and anxiety/depressive disorders [24,25,26]. Very few studies have analyzed HPAA function in ADHD while accounting both for the phenotypic symptom presentation and for comorbid symptoms of ODD/CD and anxiety/depressive disorders. Isik et al. [27] studied drug-naïve children presenting with combined (inattentive and hyperactive) symptoms. Serum cortisol did not differ between these children and healthy controls. Angeli et al. [28] reported a lower cortisol awakening response and diurnal profile (using saliva samples) in children with ADHD than in healthy controls, irrespective of the presentation of predominantly inattentive symptoms or combined symptoms. The latter study excluded children with comorbid disorders. On the whole, it is currently unclear whether the low cortisol level of children with ADHD indicates low attention regulation capacity and/or low emotional reactivity associated with comorbid ODD/CD. In the present study, we, therefore, consider comorbid ODD/CD and assess the sympathetic reactivity to mildly anxiety-eliciting stimuli.
ADHD is more common in families with a low socioeconomic status [29] and is closely related to psychosocial risk factors including maternal depression/depressive symptoms [30, 31]. As these conditions have sometimes been found to be associated with HCC in the general population [20, 32] it is possible that low HCC in ADHD indicates exposure to environmental adversity. Therefore, we control for influences of indicators of adverse childhood experiences (ACE). Moreover, we aimed to investigate a sample of medication-naïve children with ADHD, as medication (e.g. with stimulants) may affect HPAA function [33]. Given that low HPAA activity can be assumed to be related to a reduced capacity to regulate arousal and attention, we sought to compare children presenting with predominantly inattentive symptoms (ADHD-I type), children with combined inattentive and hyperactive/impulsive symptoms (ADHD-C type), and healthy control children with regard to HCC. We hypothesized a moderator effect by sex of child (i.e. a sex-by-group interaction effect) on HCC, with boys of the ADHD-I type showing the lowest HCC. As low sympathetic reactivity to anxiety-eliciting stimuli of children with comorbid ODD/CD might also explain the low HPAA activity found in children with ADHD, it is further hypothesized that children with ADHD and comorbid ODD/CD show lower HCC and lower sympathetic reactivity than healthy control children.
Methods
Participants
The complete study sample consisted of 290 children aged between 6 and 11 years. Of these children, 130 (92 boys) were diagnosed with ADHD. Children were medication-naïve (i.e. never received any continuous psychotropic medications). Further exclusion criteria were: IQ < 80, motor disabilities, sensory disabilities, chronic physical diseases involving brain functions, any continuous pharmacological treatment in the last three months (including topical and inhaled steroids), and insufficient German language skills of parents or child. Children were recruited via a child and adolescent psychiatry practice and outpatient clinics in Gießen, Marburg, and Butzbach (Middle Hesse, Germany). Healthy control children were from the same district. The control children took part in the school-age assessment wave of a longitudinal study (see e.g. Pauli-Pott et al. [26]) or were recruited through primary schools in Marburg. In addition to the exclusion criteria used for the ADHD group, children with a diagnosis of any mental disorder were excluded.
HCC was analyzed in 205 children (107 healthy control children and 98 children diagnosed with ADHD). The remaining children (n = 75 excluded because parents refused to take part in the hair collection part of the study or the child did not fulfill the criterion of minimum hair length of 3 cm; n = 6 because insufficient hair was collected; n = 4 were outliers in the HCC distributions, see below) did not differ from those with complete data regarding ADHD vs. control group membership (χ2 (1) = 2.38), maternal and paternal education level (χ2 (4) scores were 2.24 and 2.54, respectively), and ODD/CD, anxiety and depressive disorder symptom scores (t-scores between 1.59 and − 1.07). Significantly more boys than girls were excluded from the analysis due to the shorter haircuts of the boys (χ2 (1) = 19.52, p < 0.001). However, in all further analyses, sex is taken into account.
Table 1 contains descriptive data of the samples with complete data. Parents and children gave their written informed consent to participate in the study and received an expense allowance of 30 Euros. The study was approved by the Ethics Committee of the Medical Faculty, University of Marburg.
Variables
ADHD symptom presentation groups
The ADHD diagnostic module of the Child and Adolescent Psychiatric Interview (CAPA) by Angold et al. [34] in the German-language DSM-5 version (translated by Dr. Yvonne Otto, Child and Adolescent Psychiatric Clinic, University of Leipzig) was conducted with the mothers of all children to confirm the presence or absence of an ADHD diagnosis. The CAPA is a well-validated, widely established clinical interview that allows clinical diagnoses to be made according to the DSM-5.
Of the 98 children with ADHD, 59 children (41 boys) presented with combined inattentive and hyperactive/impulsive symptoms according to the DSM-5 (ADHD-C) and 35 children (17 boys) presented with predominantly inattentive symptoms (ADHD-I). The remaining four children (three boys) presented with predominantly hyperactive/impulsive symptoms and were excluded.
Hair cortisol concentration (HCC)
Several thin hair strands were cut from the posterior vertex region of the head. The first proximal scalp-near 3-cm segment was used for the determination of HCC. This 3-cm segment is thought to reflect the cumulative cortisol secretion of the past 3 months. Hair-washing and cortisol extraction procedures were based on a laboratory protocol first described by Stalder et al. [35], with minor modifications [36, 37]. The intra-assay and inter-assay coefficient of variance (CV) of the immunoassay were below 5% (1.9% and 4.6%, respectively). In the whole sample, the HCC showed a skewed distribution. The distributions were therefore normalized by the exclusion of outliers exceeding the mean + 3 SD (four cases) and subsequently log-transformed.
Potential influences of the child’s age, hair wash frequency, BMI z-score, and family socioeconomic status (SES) (indicated by maternal education level) on the HCC scores (see [11, 38]) were checked in the subsamples of ADHD and healthy children. We found no significant correlations of HCC with the age of the child (ADHD group: 0.00; control group: 0.03), the hair-washing frequency (− 0.02; − 0.03), and the BMI z-score (0.07, 0.10). Maternal education level related to HCC in the ADHD group (0.21, p < 0.05) but not in the control group (0.01). We controlled for SES variables in the main analyses.
Sympathetic reactivity
Reactivity of the sympathetic nervous system can be validly measured by indices of electrodermal activity (EDA) [39]. We measured the electrodermal reactivity to six questions from the interview-on-attractive-toys task (measuring withdrawal vs. approach behavior; adapted from Asendorpf, [40]). The child is told that he/she will receive a gift for participating, but that before receiving the gift, he/she will take part in a video-recorded interview, conducted by a colleague, on the attractiveness of a series of toys. After 3 min of waiting, an unfamiliar adult enters the room, places six different toys in front of the child, and asks six questions, with a break of 10 s between the child’s answer and the next question. The procedure was videotaped, and video and EDA recordings were synchronized. The measurement of EDA followed the guidelines by Boucsein et al. [39] using a BioPac MP150 system with two silver-silver chloride (Ag/AgCl) disposable electrodes attached to the middle phalanges of the middle and ring finger of the non-dominant hand. The frequency of the skin conductance responses (SCR; in microsiemens) elicited by the six questions was used as an indicator of the child’s sympathetic reactivity.
Comorbidity
ODD and CD
The ODD and CD diagnostic modules of the CAPA interview were conducted with the mother. Of the 98 children with ADHD, n = 36 (25 boys) children received a diagnosis of ODD and n = 5 (three boys) received an additional diagnosis of CD. Dimensional ODD/CD scores were used to capture the whole range of symptoms in children from the ADHD and the control group.
Furthermore, we used three scales from the German-language Parent Rating Scale for Oppositional Defiant and Conduct Disorder (FBB-SSV) [41]): the oppositional symptoms scale, the conduct disorder symptoms scale, and the callous-unemotional scale. This questionnaire is suitable for the assessment of ODD/CD symptoms and callous-unemotional (CU) traits in line with the DSM-5 and ICD-10 and has shown good psychometric properties.
Anxiety and depressive disorder symptoms
The clinical screening interview of the Diagnostic System of Mental Disorders in Children and Adolescents (DISYPS) [41] was conducted with the mother by a trained psychologist. The interview assesses central symptom criteria (according to the DSM-5) for anxiety and depressive disorders. The anxiety and depressive disorder symptom scores were used to capture symptom expression in each domain.
Adverse childhood experiences
For control purposes, maternal education level, psychosocial risks, and maternal depressive symptoms were assessed. Maternal education level and psychosocial risks (according to Laucht et al. [42], index comprising the presence of: at least one parent without occupational qualification, at least one parent with a broken home background, early parenthood, parental separation, and unwanted pregnancy) were assessed by structured interviews. Maternal depressive symptoms were measured using the German version of the Center for Epidemiologic Studies Depression Scale (CES-D). For this version, good internal consistency (Cronbach’s Alpha = 0.89) and validity (correlations with other depression questionnaires) have been established [43].
Statistical analysis
To test our first hypothesis, analysis of variance (ANOVA, model 1) was conducted with HCC as criterion and sex and group as between-subjects factors. The four ADHD-H-type children were excluded from this analysis. In subsequent analyses, we adjusted for the CAPA ODD/CD symptom interview score and the oppositional symptoms scale, the conduct disorder symptoms scale, and the callous-unemotional scale of the FBB-SSV Parent Rating Scale in model 2, for anxiety and depressive disorder symptom scores of the DISYPS interview in model 3, and for the indicators of ACE (i.e. maternal education, psychosocial risk score, and maternal depressive symptoms) in model 4. To test our second and third hypotheses regarding low HCC and SR of children with ADHD and comorbid ODD/CD analogous ANOVA models were used. We adjusted for anxiety and depressive disorder symptom scores (model 2) and for the indicators of ACE (model 3). Distributions of all psychopathological symptom dimensions were right-skewed in the control and the ADHD groups. As high scores probably represent an extreme expression of symptoms rather than artifacts, outliers (> m + 3 s) were winsorized and the distributions were then log-transformed, leading to sufficiently symmetric distributions with skewness coefficients below 1.0. The hypotheses were tested with an alpha error of 5% (level of significance of 0.05).
Results
ADHD symptom presentation
The analysis of variance (ANOVA) with sex and group (i.e. ADHD-I, ADHD-C, and control group) as between-subjects factors revealed a statistically significant sex-by-group interaction effect on HCC (Table 2, Fig. 1). Consistent with our expectation, boys in the ADHD-I group showed the lowest HCC, with post-hoc comparisons revealing significantly lower HCC in ADHD-I than in control boys. Moreover, girls with ADHD-C showed significantly higher HCC than did girls in the control group (Fig. 1). Results remained after adjusting for the ODD/CD dimensional symptoms scores (Table 2, model 2) and symptoms of anxiety and depressive disorders (Table 2, model 3). Likewise, the exclusion of children with ODD/CD diagnoses from the analysis did not change the significant interaction effect (F (2,160) = 3.15, p = 0.046). Adjusting for the indicators of ACE led to a non-significant interaction effect on HCC (Table 2, model 4). In all models, the main effects were not statistically significant (Table 2). Groups did not differ in the SR measure (main effect sex, F (1,182) = 1.18, main effect group, F (2,182) = 2.15, sex-by-group interaction, F (2,182) = 2.29).
Significant interaction effect between sex and group (ADHD-I, ADHD-C vs. control group). Post hoc comparisons (Scheffé tests): in boys: control group > ADHD-I group; in girls: control group < ADHD-C group (*p < 0.05). Means (height of column) ± 1se are depicted; ADHD, attention deficit hyperactivity disorder, ODD oppositional defiant disorder, CD conduct disorder, ADHD-I ADHD with predominantly inattentive symptoms, ADHD-C ADHD with combined inattentive and hyperactive/impulsive symptoms, HCC hair cortisol concentration
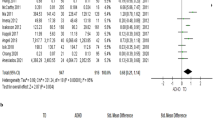
Comorbid ODD/CD
We compared boys and girls with pure ADHD, ADHD plus ODD/CD diagnosis, and healthy control children. The sex-by-group interaction effect on HCC proved to be statistically significant (Table 3, Fig. 2a). Post hoc tests revealed a significantly higher HCC in girls with ADHD + ODD/CD compared to healthy girls. Controlling for anxiety and depressive disorder scores did not change the results of this analysis (see Table 3, model 2). After adjusting for the indicators of ACE, the sex-by-group interaction effect was no longer significant (Table 3, model 3). In most models, the main effects of sex and group were not statistically significant (Table 3).
Significant interaction effect between sex and group (pure ADHD, ADHD + ODD/CD vs. control group) on HCC (a) and SR (b). Post hoc comparisons (Scheffé tests): a for girls: control group < ADHD + ODD/CD group, b for boys: control group > pure ADHD group and control group > ADHD + ODD/CD; *p < 0.05, ***p < 0.001. Means (height of column) ± 1se are depicted, ADHD attention deficit hyperactivity disorder, CD conduct disorder, ODD oppositional defiant disorder, HCC hair cortisol concentration, SR sympathetic reactivity
Regarding the SR measure, the sex-by-group interaction effect was statistically significant (Table 3, Fig. 2b). While no significant group differences emerged for the girls, boys with comorbid ADHD + ODD/CD and boys with pure ADHD showed lower SR than did healthy boys (Fig. 2b). Main effects were not statistically significant (Table 3). Results remained after adjusting for symptoms of anxiety and depressive disorders (Table 3, model 2) and indicators of ACE (Table 3, model 3).
The indicators of ACE explained variance in the HCC measure (i.e. adjustment for maternal education level, maternal depressive symptoms, and psychosocial risks led to non-significant results). To further explore this effect, we calculated the correlation coefficients of the ACE variables with HCC. In the ADHD group, maternal education level (r = 0.21, p = 0.046) and maternal depressive symptoms (r = − 0.22, p = 0.041) were significantly associated with HCC. Children of mothers with a lower education level and higher depressive symptoms showed lower HCC. The psychosocial risks did not correlate with HCC and in the control group of healthy children correlations between the ACE variables and HCC were not significant.
Discussion
The present study aimed to identify phenotypic features associated with low HPAA activity in ADHD. Currently, it is not yet clear which components and associates of ADHD relate to the blunted HPAA activity of children with ADHD. In line with our hypotheses, significant sex differences emerged in the HCC-ADHD association (i.e. a significant sex-by-ADHD group interaction effect). As expected, boys presenting with predominantly ADHD inattentive symptoms (ADHD-I type) showed lower HCC than healthy boys. Girls with ADHD-C showed significantly higher HCC compared to healthy girls. The results remained unchanged after adjusting for comorbid symptom dimensions and after the exclusion of children with comorbid ODD/CD. Analyses of comorbid ODD/CD diagnoses revealed increased HCC in girls with ADHD plus ODD/CD compared to healthy girls. Boys with ADHD, and those with comorbid ADHD plus ODD/CD, showed reduced SR to the anxiety/withdrawal-eliciting stimuli. Adjustment for ACE indicators (i.e. maternal education level, maternal depressive symptoms, family psychosocial risks) led to non-significant HCC differences but did not affect the differences in SR. Taken together, the findings demonstrate that low long-term cortisol secretion is primarily a characteristic of boys with the ADHD-I type, while girls show a different pattern, characterized by relatively high cortisol secretion in those with the ADHD-C and the comorbid ADHD + ODD/CD type. Interestingly, ACE indicators explain these differences.
In general population samples, sex differences in HCC are well established, with females showing lower HCC than males [11]. In our study, the healthy girls showed lower HCC than the healthy boys on a descriptive level. This is well in line with the general population finding and indicates a good validity of our data. The low HCC in boys presenting with predominantly inattentive symptoms in the present study corresponds to previous findings of an association between low cortisol activity/reactivity and neurocognitive deficits [25, 44], the prediction of ADHD development by reduced HCC [26], and with theories suggesting a low capacity to adjust arousal to cognitive demands in children with ADHD [17, 19]. Moreover, attentional, cognitive control, and working memory deficits of children with ADHD involve structural and functional deviations in hippocampal and frontal brain circuitry [45]. Activity in these areas is known to be modulated by glucocorticoid secretion [12]. In cases of hyper- and hypocortisolism, impairing cortisol-mediated effects on cognition have been emphasized [46, 47]. Hence, investigation of the mechanisms linking HPAA dysfunction with ADHD subgroups could be worthwhile.
Low HCC in boys with ADHD was not related to comorbid ODD/CD. However, consistent with well-established models on ODD/CD [14,15,16], boys with comorbid ADHD + ODD/CD showed reduced SR to the anxiety/withdrawal eliciting stimuli. However, in comparison to the healthy boys the boys with pure ADHD also showed reduced SR. The latter result resembles previous findings of our group: in a community-based sample, ADHD symptoms were negatively associated with SR [48]. Other studies found hypoactivation of the sympathetic nervous system not only during cognitive but also during emotional tasks (though less consistent) in children with ADHD [17, 18]. This might explain our result. However, more research is needed to clarify the role of subclinical symptoms of ODD/CD regarding SR to emotional stimuli.
In the present study, girls with ADHD-C and with ADHD plus ODD/CD showed increased HCC compared to children in the control group. It might be speculated that hyperactive/impulsive and ODD/CD symptoms in girls reflect increased irritability and/or emerging depressive disorder symptoms. Irritability/depression is more prevalent in females [49, 50] and has been found to be associated with relative hypercortisolism [51]. However, this effect was not explained by the depressive symptom score in our study (i.e. the interaction effect remained after controlling for depressive and anxiety disorder symptoms). Hence, it might be that a more specific measure of irritability/sensitivity to threat [52] would have revealed an association. For the time being, this issue remains open and needs to be analyzed in future studies.
In our analyses, we considered indicators of ACE which have often been found to be associated with ADHD. The variables explained significant variance in HCC. In the ADHD group, children of mothers with a lower education level and higher depressive symptoms showed lower HCC. This corresponds to the findings of studies by White et al. [21, 53] on children/adolescents with externalizing disorders: low HCC was found in children with externalizing disorders who experienced (emotional) maltreatment. Maternal depressive symptoms may reflect family adversity and indicate less adequate parenting, thus potentially chronic ACE, which in turn leads to low HCC in the child [10]. Recent results of a longitudinal twin study confirmed a mediation process. Iob et al.[54] found basal cortisol to mediate 18% of the total association between dysfunctional parenting/emotional abuse (including maternal depression) and depressive symptoms in adolescence while controlling for genetic effects. Moreover, a twin study on adolescent HCC in particular pointed to non-shared environmental effects (69%) besides moderate heritability (39%) [55]. Hence, it is possible that environmental effects or gene-environment interaction effects explain our results. However, it is also possible that genetic effects, effects of fetal programming of the HPAA system [10, 32, 56], or severity of ADHD explain the association between maternal depressive symptoms and low HCC in the child. It is a limitation of our study that we cannot distinguish between these components. The associations should be analyzed in more detail in future studies as it is possible that specific environmental conditions are implicated in HPA axis dysfunction in ADHD subtypes.
Several strengths of the present study can be noted, including the analysis of medication-naïve children, the detailed assessment of confounders, the use of dimensional scores and diagnoses from well-validated clinical interviews, the use of an indicator of SR, and the use of HCC as a reliable and valid measure of the cumulated long-term activity of the HPAA. Limitations might be seen in the following issues: We found that low HCC relates to specific phenotypic characteristics of ADHD. Though compatible with current theorizing, the biological mechanisms linking HCC to inattentive symptom presentation in boys are largely unknown and should, therefore, be analyzed in the future. Moreover, indicators of ACE could have been analyzed in more detail. Considering maltreatment could be particularly elucidating (see e.g. [21, 53, 57]). Finally, in future studies, it may be illuminating to analyze further hormones (e.g. corticotropin-releasing factor and adrenocorticotropic hormone) and parameters (e.g. diurnal cortisol profile, cortisol reactivity and regulation) of the HPAA to determine which components of the system are affected.
To conclude, our findings underscore the presence of sex differences in the association of HCC with phenotypic features of ADHD. Indicators of ACE were related to low HCC in ADHD while comorbid conditions played an ancillary role. Hence, in the context of ADHD in childhood, HCC constitutes a meaningful marker of homogenous subgroups. It appears worthwhile to further analyze the role of HCC in ADHD in childhood. The marker might help to circumscribe specific developmental pathways and to provide tailored preventive measures and treatment approaches.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Scassellati C, Bonvicini C, Faraone SV, Gennarelli M (2012) Biomarkers and attention-deficit/hyperactivity disorder: a systematic review and meta-analyses. J Am Acad Child Adolesc Psychiatry 51(10):1003–1019
Kamradt JM, Momany AM, Nikolas MA (2018) A meta-analytic review of the association between cortisol reactivity in response to a stressor and attention-deficit hyperactivity disorder. Adhd Attend Deficit 10(2):99–111. https://doi.org/10.1007/s12402-017-0238-5
Bernhard A, Mayer JS, Fann N, Freitag CM (2021) Cortisol response to acute psychosocial stress in ADHD compared to conduct disorder and major depressive disorder: a systematic review. Neurosci Biobehav Rev 127:899–916. https://doi.org/10.1016/j.neubiorev.2021.06.005
Fairchild G, Baker E, Eaton S (2018) Hypothalamic-pituitary-adrenal axis function in children and adults with severe antisocial behavior and the impact of early adversity. Curr Psychiatry Rep. https://doi.org/10.1007/s11920-018-0952-5. (ARTN 84)
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Washington
Gillberg C, Gillberg IC, Rasmussen P, Kadesjo B, Soderstrom H, Rastam M, Johnson M, Rothenberger A, Niklasson L (2004) Co-existing disorders in ADHD - implications for diagnosis and intervention. Eur Child Adoles Psy 13:80–92. https://doi.org/10.1007/s00787-004-1008-4
Faraone SV, Asherson P, Banaschewski T, Biederman J, Buitelaar J, Ramos-Quiroga JA (2015) Attention deficit/hyperactivity disorder. Nat Rev Dis Prim. https://doi.org/10.1038/nrdp.2015.20
Foley P, Kirschbaum C (2010) Human hypothalamus-pituitary-adrenal axis responses to acute psychosocial stress in laboratory settings. Neurosci Biobehav Rev 35(1):91–96. https://doi.org/10.1016/j.neubiorev.2010.01.010
Rietschel L, Streit F, Zhu G, McAloney K, Frank J, Couvy-Duchesne B, Witt SH, Binz TM, McGrath J, Hickie IB, Hansell NK, Wright MJ, Gillespie NA, Forstner AJ, Schulze TG, Wust S, Nothen MM, Baumgartner MR, Walker BR, Crawford AA, Colodro-Conde L, Medland SE, Martin NG, Rietschel M, Consortium CC, Disorder MD (2017) Hair cortisol in twins: heritability and genetic overlap with psychological variables and stress-system genes. Sci Rep-Uk. https://doi.org/10.1038/s41598-017-11852-3. (ARTN 15351)
Koss KJ, Gunnar MR (2018) Annual Research Review: Early adversity, the hypothalamic-pituitary-adrenocortical axis, and child psychopathology. J Child Psychol Psychiatry 59(4):327–346. https://doi.org/10.1111/jcpp.12784
Stalder T, Steudte-Schmiedgena S, Alexander N, Klucken T, Vatera A, Wichmann A, Kirschbaum C, Miller R (2017) Stress-related and basic determinants of hair cortisol in humans: a meta-analysis. Psychoneuroendocrinology 77:261–274
Schwabe L, Joels M, Roozendaal B, Wolf OT, Oitzl MS (2012) Stress effects on memory: an update and integration. Neurosci Biobehav Rev 36(7):1740–1749. https://doi.org/10.1016/j.neubiorev.2011.07.002
Zuckerman M, Neeb M (1979) Sensation seeking and psychopathology. Psychiat Res 1(3):255–264. https://doi.org/10.1016/0165-1781(79)90007-6
Viding E, McCrory EJ (2018) Understanding the development of psychopathy: progress and challenges. Psychol Med 48(4):566–577. https://doi.org/10.1017/S0033291717002847
Raine A (2002) Annotation: The role of prefrontal deficits, low autonomic arousal, and early health factors in the development of antisocial and aggressive behavior in children. J Child Psychol Psychiatry 43(4):417–434. https://doi.org/10.1111/1469-7610.00034
van Goozen SHM, Fairchild G, Snoek H, Harold GT (2007) The evidence for a neurobiological model of childhood antisocial behavior. Psychol Bull 133(1):149–182. https://doi.org/10.1037/0033-2909.133.1.149
Bellato A, Arora I, Hollis C, Groom MJ (2020) Is autonomic nervous system function atypical in attention deficit hyperactivity disorder (ADHD)? A systematic review of the evidence. Neurosci Biobehav Rev 108:182–206. https://doi.org/10.1016/j.neubiorev.2019.11.001
Conzelmann A, Gerdes ABM, Mucha RF, Weyers P, Lesch KP, Bahne CG, Fallgatter AJ, Renner TJ, Warnke A, Romanos M, Pauli P (2014) Autonomic hypoactivity in boys with attention-deficit/hyperactivity disorder and the influence of methylphenidate. World J Biol Psychia 15(1):56–65. https://doi.org/10.3109/15622975.2013.829584
Sergeant JA (2005) Modeling attention-deficit/hyperactivity disorder: a critical appraisal of the cognitive-energetic model. Biol Psychiatry 57(11):1248–1255. https://doi.org/10.1016/j.biopsych.2004.09.010
Khoury JE, Enlow MB, Plamondon A, Lyons-Ruth K (2019) The association between adversity and hair cortisol levels in humans: a meta-analysis. Psychoneuroendocrinology 103:104–117. https://doi.org/10.1016/j.psyneuen.2019.01.009
White LO, Ising M, von Klitzing K, Sierau S, Michel A, Klein AM, Andreas A, Keil J, Quintero L, Muller-Myhsok B, Uhr M, Gausche R, Manly JT, Crowley MJ, Kirschbaum C, Stalder T (2017) Reduced hair cortisol after maltreatment mediates externalizing symptoms in middle childhood and adolescence. J Child Psychol Psychiatry 58(9):998–1007. https://doi.org/10.1111/jcpp.12700
Koss KJ, Mliner SB, Donzella B, Gunnar MR (2016) Early adversity, hypocortisolism, and behavior problems at school entry: a study of internationally adopted children. Psychoneuroendocrinology 66:31–38. https://doi.org/10.1016/j.psyneuen.2015.12.018
Russell E, Koren G, Rieder M, Van Uum S (2012) Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology 37(5):589–601. https://doi.org/10.1016/j.psyneuen.2011.09.009
Pauli-Pott U, Schloss S, Ruhl I, Skoluda N, Nater UM, Becker K (2017) Hair cortisol concentration in preschoolers with attention-deficit/hyperactivity symptoms-roles of gender and family adversity. Psychoneuroendocrinology 86:25–33. https://doi.org/10.1016/j.psyneuen.2017.09.002
Mann C, Schloss S, Cosan A, Becker K, Skoluda N, Nater UM, Pauli-Pott U (2021) Hair cortisol concentration and neurocognitive functions in preschool children at risk of developing attention deficit hyperactivity disorder. Psychoneuroendocrinology. https://doi.org/10.1016/j.psyneuen.2021.105322. (ARTN 105322)
Pauli-Pott U, Schloss S, Skoluda N, Nater UM, Becker K (2019) Low hair cortisol concentration predicts the development of attention deficit hyperactivity disorder. Psychoneuroendocrinology. https://doi.org/10.1016/j.psyneuen.2019.104442. (ARTN 104442)
Isik U, Bilgic A, Toker A, Kilinc I (2018) Serum levels of cortisol, dehydroepiandrosterone, and oxytocin in children with attention-deficit/hyperactivity disorder combined presentation with and without comorbid conduct disorder. Psychiat Res 261:212–219. https://doi.org/10.1016/j.psychres.2017.12.076
Angeli E, Korpa T, Johnson EO, Apostolakou F, Papassotiriou I, Chrousos GP, Pervanidou P (2018) Salivary cortisol and alpha-amylase diurnal profiles and stress reactivity in children with attention deficit hyperactivity disorder. Psychoneuroendocrinology 90:174–181. https://doi.org/10.1016/j.psyneuen.2018.02.026
Larsson H, Sariaslan A, Langstrom N, D’Onofrio B, Lichtenstein P (2014) Family income in early childhood and subsequent attention deficit/hyperactivity disorder: a quasi-experimental study. J Child Psychol Psychiatry 55(5):428–435. https://doi.org/10.1111/jcpp.12140
Biederman J, Faraone SV, Monuteaux MC (2002) Differential effect of environmental adversity by gender: rutter’s index of adversity in a group of boys and girls with and without ADHD. Am J Psychiatry 159(9):1556–1562. https://doi.org/10.1176/appi.ajp.159.9.1556
Tucker JRD, Hobson CW (2021) A systematic review of longitudinal studies investigating the association between early life maternal depression and offspring ADHD. J Atten Dis. https://doi.org/10.1177/10870547211063642. (Artn 10870547211063642)
Ursache A, Noble KG (2016) Neurocognitive development in socioeconomic context: multiple mechanisms and implications for measuring socioeconomic status. Psychophysiology 53(1):71–82. https://doi.org/10.1111/psyp.12547
Wang LJ, Huang YS, Hsiao CC, Chen CK (2017) The trend in morning levels of salivary cortisol in children with ADHD during 6 months of methylphenidate treatment. J Atten Disord 21(3):254–261. https://doi.org/10.1177/1087054712466139
Angold A, Prendergast M, Cox A, Harrington R, Simonoff E, Rutter M (1995) The child and adolescent psychiatric-assessment (Capa). Psychol Med 25(4):739–753. https://doi.org/10.1017/S003329170003498x
Stalder T, Steudte S, Miller R, Skoluda N, Dettenborn L, Kirschbaum C (2012) Intraindividual stability of hair cortisol concentrations. Psychoneuroendocrinology 37(5):602–610. https://doi.org/10.1016/j.psyneuen.2011.08.007
Wuttke-Linnemann A, Henrici C, Skoluda N, Nater UM, Endres K, Fellgiebel A (2022) Psychobiological monitoring of a home-based dyadic intervention for people living with dementia and their caregivers: added value to evaluate treatment success and understand underlying mechanisms. J Alzheimer’s Dis (Preprint). https://doi.org/10.3233/JAD-210618
Goreis A, Nater UM, Skoluda N, Mewes R (2022) Psychobiological effects of chronic ethnic discrimination in Turkish immigrants: stress responses to standardized face-to-face discrimination in the laboratory. Psychoneuroendocrinology. https://doi.org/10.1016/j.psyneuen.2022.105785. (ARTN 105785)
Gray NA, Dhana A, Van Der Vyver L, Van Wyk J, Khumalo NP, Stein DJ (2018) Determinants of hair cortisol concentration in children: a systematic review. Psychoneuroendocrinology 87:204–214. https://doi.org/10.1016/j.psyneuen.2017.10.022
Boucsein W, Fowles DC, Grimnes S, Ben-Shakhar G, Roth WT, Dawson ME, Filion DL, Hoc SPRA (2012) Publication recommendations for electrodermal measurements. Psychophysiology 49(8):1017–1034. https://doi.org/10.1111/j.1469-8986.2012.01384.x
Asendorpf JB (1990) Development of inhibition during childhood: Evidence for situational specificity and a two-factor model. Dev Psychol 26:721–730
Döpfner M, Görtz-Dorten A (2017) DISYPS-III. Diagnostik-System für psychische Störungen nach ICD-10 und DSM-5 für Kinder und Jugendliche—III. Hogrefe, Bern
Laucht M, Skowronck MH, Becker K, Schmidt MH, Esser G, Schulze TG, Rietschel M (2007) Interacting effects of dopamine transporter gene and psychosocial adversity on attention-deficit/hyperactivity Disorder symptoms among 15-year-olds from a high-risk community sample. Arch Gen Psychiatry 64:585–590
Hautzinger M, Bailer M, Hofmeister D, Keller F (2012) Allgemeine Depressionsskala (Aufl. 2). Hogrefe, Göttingen
Raffington L, Prindle J, Keresztes A, Binder J, Heim C, Shing YL (2018) Blunted cortisol stress reactivity in low-income children relates to lower memory function. Psychoneuroendocrinology 90:110–121. https://doi.org/10.1016/j.psyneuen.2018.02.002
Lukito S, Norman L, Carlisi C, Radua J, Hart H, Simonoff E, Rubia K (2020) Comparative meta-analyses of brain structural and functional abnormalities during cognitive control in attention-deficit/hyperactivity disorder and autism spectrum disorder. Psychol Med 50(6):894–919. https://doi.org/10.1017/S0033291720000574. (Pii S0033291720000574)
Lupien SJ, Juster RP, Raymond C, Marin MF (2018) The effects of chronic stress on the human brain: from neurotoxicity, to vulnerability, to opportunity. Front Neuroendocrinol 49:91–105. https://doi.org/10.1016/j.yfrne.2018.02.001
McEwen BS, Gianaros PJ (2010) Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann Ny Acad Sci 1186:190–222. https://doi.org/10.1111/j.1749-6632.2009.05331.x
Schloss S, Derz F, Schurek P, Cosan AS, Becker K, Pauli-Pott U (2021) Reward-related dysfunctions in children developing attention deficit hyperactivity disorder-roles of oppositional and callous-unemotional symptoms. Front Psychiatry. https://doi.org/10.3389/fpsyt.2021.738368. (ARTN 738368)
Martel MM (2013) Sexual selection and sex differences in the prevalence of childhood externalizing and adolescent internalizing disorders. Psychol Bull 139(6):1221–1259. https://doi.org/10.1037/a0032247
Narmandakh A, Roest AM, de Jonge P, Oldehinkel AJ (2021) Psychosocial and biological risk factors of anxiety disorders in adolescents: a TRAILS report. Eur Child Adolesc Psychiatry 30(12):1969–1982. https://doi.org/10.1007/s00787-020-01669-3
Staufenbiel SM, Penninx BWJH, Spijker AT, Elzinga BM, van Rossum EFC (2013) Hair cortisol, stress exposure, and mental health in humans: a systematic review. Psychoneuroendocrinology 38(8):1220–1235. https://doi.org/10.1016/j.psyneuen.2012.11.015
Blair RJ, Leibenluft E, Pine DS (2014) Conduct disorder and callous-unemotional traits in youth. N Engl J Med 371(23):2207–2216. https://doi.org/10.1056/NEJMra1315612
Schlensog-Schuster F, Keil J, Von Klitzing K, Gniewosz G, Schulz CC, Schlesier-Michel A, Mayer S, Stadelmann S, Dohnert M, Klein AM, Sierau S, Manly JT, Sheridan MA, White LO (2022) From maltreatment to psychiatric disorders in childhood and adolescence: the relevance of emotional maltreatment. Child Maltreat. https://doi.org/10.1177/10775595221134248
Iob E, Baldwin JR, Plomin R, Steptoe A (2021) Adverse childhood experiences, daytime salivary cortisol, and depressive symptoms in early adulthood: a longitudinal genetically informed twin study. Transl Psychiatry. https://doi.org/10.1038/s41398-021-01538-w. (ARTN 420)
Cantave CY, Brendgen M, Lupien S, Dionne G, Vitaro F, Boivin M, Ouellet-Morin I (2022) Association between the timing of family socioeconomic deprivation and adolescence hair cortisol among adolescent twins: a study of the genetic and environmental processes involved. Psychoneuroendocrinology. https://doi.org/10.1016/j.psyneuen.2022.105889. (ARTN 105889)
Bryson HE, Mensah F, Goldfeld S, Price AMH, Giallo R (2021) Hair cortisol in mother-child dyads: examining the roles of maternal parenting and stress in the context of early childhood adversity. Eur Child Adolesc Psychiatry 30(4):563–577. https://doi.org/10.1007/s00787-020-01537-0
Ouyang L, Fang X, Mercy J, Perou R, Grosse SD (2008) Attention-deficit/hyperactivity disorder symptoms and child maltreatment: a population-based study. J Pediatr 153(6):851–856. https://doi.org/10.1016/j.jpeds.2008.06.002
Acknowledgements
The research for this article was funded by a Grant from the German Research Foundation (DFG, Be2573/3-1,3-2) to Prof. Dr. Katja Becker and Prof. Dr. Ursula Pauli-Pott and the University of Marburg (Forschungsförderfond MR/17) to Susan Schloß, Ursula Pauli-Pott, and Katja Becker.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission made substantial contributions.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Medical Faculty, University of Marburg.
Informed consent
Parents and children gave their written informed consent to participate in the study.
Consent for publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pauli-Pott, U., Skoluda, N., Nater, U.M. et al. Long-term cortisol secretion in attention deficit hyperactivity disorder: roles of sex, comorbidity, and symptom presentation. Eur Child Adolesc Psychiatry 33, 569–579 (2024). https://doi.org/10.1007/s00787-023-02180-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-023-02180-1