Abstract
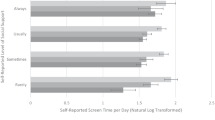
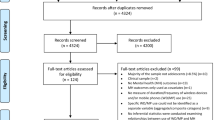
A strong association between sleep problems and suicidal thoughts and behaviors (STBs) has been demonstrated in high-income countries. The sleep-STB relationship, however, is minimally understood among youth in low and middle-incomes countries. There also is a limited understanding of how individual- (i.e., age, sex) and country-level (i.e., economic inequality, economic quality) factors may moderate the magnitude of the sleep-STB association among youth. Data were analyzed from the cross-national Global School-based Health Survey 2003–2017, which assessed a range of health behaviors among school-enrolled adolescents aged 11–18 years from 88 low-, lower-middle, upper-middle, and high-income countries. Multilevel models were used to examine the influence of individual- and country-level factors on the association between past-year worry-related sleep problems and past-year suicide ideation, suicide plans, and suicide attempts. Worry-related sleep problems were significantly associated with suicide ideation, plans, and attempts. Adolescent sex, country economic quality (income group designation), and country economic inequality moderated the sleep-STB association, but age did not. The sleep-STB relationship was stronger for males and across macroeconomic indices, the relationship was generally strongest among upper-middle income countries (economic quality) and countries with a big income gap (economic inequality). When examining how individual-level factors differentially affected the sleep-STB relationship within economic quality (income group designation), the effects were driven by older adolescents in high-income countries for suicide ideation and suicide plans. Study findings suggest an important role for global macroeconomic factors, for males, and older adolescents in high-income countries in the sleep-STB relationship. Future directions include expanding worldwide coverage of countries, assessing a wider range of sleep problems, and longitudinal work to understand potential mechanisms in the sleep-STB relationship.



Similar content being viewed by others
Availability of data and material
The GSHS datasets publicly available via the World Health Organization.
Code availability
Analyses were performed in SAS 9.4.
Notes
Consistent with prior GSHS work (e.g., Dema et al. [36], Uddin et al. [3]), all currently available GSHS datasets were used to maximize the coverage of LMICs. This approach was selected so as not to decrease the representation of countries, particularly those in the African Region (e.g., Tunisia, Uganda), where data would otherwise be unavailable.
The GSHS provided a range of age responses, depending on the survey year. For example, more recent surveys provided the following age options: 11 years old or younger, 12 years old, 13 years old, 14 years old, 15 years old, 16 years old, 17 years old, 18 years old or older while older surveys provided the following age options: 11 years old or younger, 12 years old, 13 years old, 14 years old, 15 years old, 16 years old or older. It is highly unlikely that children younger than age 11 or older than age 18 were included in the study, however, these are the age options that GSHS provided respondents. Due to these differing age response options across the 2003–2017 GSHS, ages 15 to 18 years old or older were collapsed into one bin (i.e., 15 years old or older) to aid in cross-national comparison. The GSHS collapsed 11 years or younger into one bin by default.
Due to the small size of some WHO regions (e.g., European Region has two countries), we elected not to examine our results by region. Instead, we chose to examine cross-national indices of economic quality and inequality as opposed to WHO region. The sleep-STB relationship is reported by country in Figs. 1–3.
Relative equality and adequate equality countries did not significantly differ on SI (χ2 = 3.75, p = 0.053, φ = 0.046), SP (χ2 = .16, p = 0.692, φ = 0.046) or worry-related sleep problems (t = −0.20, p = 0.842). These countries did differ on SA (χ2 = 31.93, p < 0.0001), but the effect size was small (φ = 0.014) and weighted percentages were similar (16.1% in countries with relative equality vs. 10.4% in countries with adequate equality). Despite this difference, we retained the combined relative/adequate equality group as we did not want to extrapolate study results from a group with only three countries (relative equality).
Abbreviations
- CBT-I:
-
Cognitive Behavioral Therapy for Insomnia
- GSHS:
-
Global School-based Student Health Survey
- HIC:
-
High-income countries
- LMIC:
-
Low- and middle-income countries
- LIC:
-
Low-income countries
- MIC:
-
Middle-income countries
- SI:
-
Suicide ideation
- SP:
-
Suicide plan
- SA:
-
Suicide attempt
- STBs:
-
Suicidal thoughts and behaviors
- UMIC:
-
Upper-middle income countries
- WHO:
-
World Health Organization
References
World Health Organization (2019) Suicide prevention. https://www.who.int/mental_health/suicide-prevention/en/
Tang JJ, Yu Y, Wilcox HC, Kang C, Wang K, Wang C, Wu Y, Chen R (2020) Global risks of suicidal behaviours and being bullied and their association in adolescents: school-based health survey in 83 countries. EClinicalMedicine 19:100253
Uddin R, Burton NW, Maple M, Khan SR, Khan A (2019) Suicidal ideation, suicide planning, and suicide attempts among adolescents in 59 low-income and middle-income countries: a population-based study. Lancet Child Adolesc Health 3(4):223–233
Biswas T, Scott JG, Munir K, Renzaho A, Rawal LB, Baxter J, Mamun A (2020) Global variation in the prevalence of suicidal ideation, anxiety and their correlates among adolescents: a population based study of 82 countries. EClinicalMedicine 24:100395
Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ (1997) Coming to terms with the terms of risk. Arch Gen Psychiatry 54(4):337–343
World Health Organization (2019) Suicide in the world: Global health estimates
Carskadon MA, Acebo C, Jenni OG (2004) Regulation of adolescent sleep. Ann N Y Acad Sci 1021:276–291
Winsler A, Deutsch A, Vorona RD, Payne PA, Szklo-Coxe M (2015) Sleepless in Fairfax: the difference one more hour of sleep can make for teen hopelessness, suicidal ideation, and substance use. J Youth Adolesc 44(2):362–378
Wong MM, Brower KJ, Nigg JT, Zucker RA (2010) Childhood sleep problems, response inhibition, and alcohol and drug outcomes in adolescence and young adulthood. Alcohol Clin Exp Res 34(6):1033–1044
McGlinchey EL, Harvey AG (2015) Risk behaviors and negative health outcomes for adolescents with late bedtimes. J Youth Adolesc 44(2):478–488
Kearns JC, Coppersmith DD, Santee AC, Insel C, Pigeon WR, Glenn CR (2020) Sleep problems and suicide risk in youth: a systematic review, developmental framework, and implications for hospital treatment. Gen Hosp Psychiatry 63:141–151
Crowley SJ, Wolfson AR, Tarokh L, Carskadon MA (2018) An update on adolescent sleep: new evidence informing the perfect storm model. J Adolesc 67:55–65
Tarokh L, Saletin JM, Carskadon MA (2016) Sleep in adolescence: physiology, cognition and mental health. Neurosci Biobehav Rev 70:182
Littlewood DL, Kyle SD, Carter L-A, Peters S, Pratt D, Gooding P (2019) Short sleep duration and poor sleep quality predict next-day suicidal ideation: an ecological momentary assessment study. Psychol Med 49(3):403–411
Pigeon WR, Pinquart M, Conner K (2012) Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry 73(9):e1160–e1167
Wong MM, Brower KJ (2012) The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J Psychiatr Res 46(7):953–959
Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, Joiner TE Jr (2012) Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord 136(3):743–750
Zuromski KL, Cero I, Witte TK (2017) Insomnia symptoms drive changes in suicide ideation: a latent difference score model of community adults over a brief interval. J Abnorm Psychol 126(6):739
Sudak H, Maxim K, Carpenter M (2008) Suicide and stigma: a review of the literature and personal reflections. Acad Psychiatry 32(2):136–142
Blake MJ, Sheeber LB, Youssef GJ, Raniti MB, Allen NB (2017) Systematic review and meta-analysis of adolescent cognitive–behavioral sleep interventions. Clin Child Fam Psychol Rev 20(3):227–249
Werner-Seidler A, Johnston L, Christensen H (2018) Digitally-delivered cognitive-behavioural therapy for youth insomnia: a systematic review. Internet Interv 11:71–78
Espie CA (2002) Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol 53(1):215–243
Espie CA, Broomfield NM, MacMahon KM, Macphee LM, Taylor LM (2006) The attention–intention–effort pathway in the development of psychophysiologic insomnia: a theoretical review. Sleep Med Rev 10(4):215–245
Harvey AG (2002) A cognitive model of insomnia. Behav Res Ther 40(8):869–893
Edinger JD, Carney CE (2014) Overcoming insomnia: A cognitive-behavioral therapy approach, therapist guide. Oxford University Press, Oxford
Dregan A, Lallukka T, Armstrong D (2013) Potential pathways from biopsychosocial risk factors to sleep loss due to worry: a population-based investigation. J Public Ment Health 12(1):43–50
Harvey AG (2000) Pre-sleep cognitive activity: a comparison of sleep-onset insomniacs and good sleepers. Br J Clin Psychol 39(3):275–286
Lund HG, Reider BD, Whiting AB, Prichard JR (2010) Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health 46(2):124–132
Watts FN, Coyle K, East MP (1994) The contribution of worry to insomnia. Br J Clin Psychol 33(2):211–220
Lallukka T, Dregan A, Armstrong D (2011) Comparison of a sleep item from the General Health Questionnaire-12 with the Jenkins Sleep Questionnaire as measures of sleep disturbance. J Epidemiol 21(6):474–480
Liu X (2004) Sleep and adolescent suicidal behavior. Sleep 27(7):1351–1358
Pengpid S, Peltzer K (2018) Vigorous physical activity, perceived stress, sleep and mental health among university students from 23 low-and middle-income countries. Int J Adolesc Med Health 32(2)
Stranges S, Tigbe W, Gómez-Olivé FX, Thorogood M, Kandala N-B (2012) Sleep problems: an emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 35(8):1173–1181
Kim HH-s, Chun J, (2020) Bullying victimization, school environment, and suicide ideation and plan: focusing on youth in low-and middle-income countries. J Adolesc Health 66(1):115–122
Page RM, West JH (2011) Suicide ideation and psychosocial distress in sub-Saharan African youth. Am J Health Behav 35(2):129–141
Dema T, Tripathy JP, Thinley S, Rani M, Dhendup T, Laxmeshwar C, Tenzin K, Gurung MS, Tshering T, Penjore T (2019) Suicidal ideation and attempt among school going adolescents in Bhutan–a secondary analysis of a global school-based student health survey in Bhutan 2016. BMC Public Health 19(1):1605
Almansour AM, Siziya S (2017) Suicidal ideation and associated factors among school going adolescents in Swaziland. Afr Health Sci 17(4):1172–1177
Smith L, Jackson SE, Vancampfort D, Jacob L, Firth J, Grabovac I, McDermott D, Yang L, López-Sánchez GF, Niederkrotenthaler T (2020) Sexual behavior and suicide attempts among adolescents aged 12–15 years from 38 countries: a global perspective. Psychiatry Res 287:112564
Koyanagi A, Stubbs B, Oh H, Veronese N, Smith L, Haro JM, Vancampfort D (2019) Food insecurity (hunger) and suicide attempts among 179,771 adolescents attending school from 9 high-income, 31 middle-income, and 4 low-income countries: a cross-sectional study. J Affect Disord 248:91–98
Adewuya AO, Oladipo EO (2019) Prevalence and associated factors for suicidal behaviours (ideation, planning, and attempt) among high school adolescents in Lagos, Nigeria. Eur Child Adolesc Psychiatry 29(11):1503–1512
Pandey AR, Bista B, Dhungana RR, Aryal KK, Chalise B, Dhimal M (2019) Factors associated with suicidal ideation and suicidal attempts among adolescent students in Nepal: findings from Global School-based Students Health Survey. PLoS ONE 14(4):e0210383
Brady D, Fullerton AS, Cross JM (2010) More than just nickels and dimes: A cross-national analysis of working poverty in affluent democracies. Soc Probl 57(4):559–585
Bachmann S (2018) Epidemiology of suicide and the psychiatric perspective. Int J Environ Res Public Health 15(7):1425
Kolves K, De Leo D (2014) Suicide rates in children aged 10–14 years worldwide: changes in the past two decades. Br J Psychiatry 205(4):283–285
Cha CB, Franz PJ, Guzmán ME, Glenn CR, Kleiman EM, Nock MK (2018) Annual research review: suicide among youth—epidemiology, (potential) etiology, and treatment. J Child Psychol Psychiatry 59(4):460–482
Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L (1999) Age-and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry 38(12):1497–1505
Bridge JA, Goldstein TR, Brent DA (2006) Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry 47(3–4):372–394
Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL (2001) Gender differences in suicide attempts from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry 40(4):427–434
Shah A (2012) Suicide rates: age-associated trends and their correlates. J Inj Violence Res 4(2):79
Glenn CR, Kleiman EM, Kellerman J, Pollak O, Cha CB, Esposito EC, Porter AC, Wyman PA, Boatman AE (2020) Annual research review: a meta-analytic review of worldwide suicide rates in adolescents. J Child Psychol Psychiatry 61(3):294–308
Haw C, Hawton K, Gunnell D, Platt S (2015) Economic recession and suicidal behaviour: possible mechanisms and ameliorating factors. Int J Soc Psychiatry 61(1):73–81
Bantjes J, Iemmi V, Coast E, Channer K, Leone T, McDaid D, Palfreyman A, Stephens B, Lund C (2016) Poverty and suicide research in low-and middle-income countries: systematic mapping of literature published in English and a proposed research agenda. Global Mental Health 3:e32
Iemmi V, Bantjes J, Coast E, Channer K, Leone T, McDaid D, Palfreyman A, Stephens B, Lund C (2016) Suicide and poverty in low-income and middle-income countries: a systematic review. Lancet Psychiatry 3(8):774–783
Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, De Girolamo G, De Graaf R, Demyttenaere K, Hu C, Iwata N (2011) Cross-national epidemiology of DSM-IV major depressive episode. BMC Med 9(1):1–16
Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S (2010) From depressive symptoms to depressive disorders: the relevance of thresholds. Br J Psychiatry 196(5):365–371
Stein DJ, Chiu WT, Hwang I, Kessler RC, Sampson N, Alonso J, Borges G, Bromet E, Bruffaerts R, De Girolamo G (2010) Cross-national analysis of the associations between traumatic events and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS ONE 5(5):e10574
Burns JK, Tomita A, Kapadia AS (2014) Income inequality and schizophrenia: increased schizophrenia incidence in countries with high levels of income inequality. Int J Soc Psychiatry 60(2):185–196
Yu S (2018) Uncovering the hidden impacts of inequality on mental health: a global study. Transl Psychiatry 8(1):1–10
Johnson SL, Wibbels E, Wilkinson R (2015) Economic inequality is related to cross-national prevalence of psychotic symptoms. Soc Psychiatry Psychiatr Epidemiol 50(12):1799–1807
Pickett KE, Wilkinson RG (2015) Income inequality and health: a causal review. Soc Sci Med 128:316–326
Chibanda D, Mesu P, Kajawu L, Cowan F, Araya R, Abas MA (2011) Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health 11(1):1–10
Youth Risk Behavior Survey Questionnaire (2019) www.cdc.gov/yrbs. Accessed 1 November 2020
Becker AE, Roberts AL, Perloe A, Bainivualiku A, Richards LK, Gilman SE, Striegel-Moore RH (2010) Youth health-risk behavior assessment in Fiji: the reliability of Global School-based Student Health Survey content adapted for ethnic Fijian girls. Ethn Health 15(2):181–197
Wang Q, Liu Y, Mati K (2020) Bully victimization is a correlate of sleep loss over worry (SLOW) among adolescents in four South-East Asian countries. Sleep Med 69:179–188
Harvey AG (2005) Unwanted intrusive thoughts in insomnia. In: Clark DA (ed) Intrusive thoughts in clinical disorders: theory, research, and treatment. Guilford Press, New York, pp 88–118
Harvey AG, Tang NK, Browning L (2005) Cognitive approaches to insomnia. Clin Psychol Rev 25(5):593–611
Miranda-Mendizabal A, Castellví P, Parés-Badell O, Alayo I, Almenara J, Alonso I, Blasco MJ, Cebria A, Gabilondo A, Gili M (2019) Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Int J Public Health 64(2):265–283
Group WB (2017) New country classifications by income level: 2017–2018. https://blogs.worldbank.org/opendata/new-country-classifications-income-level-2017-2018
World Bank Group (2020) Why use GNI per capita to classify economies into income groupings? https://datahelpdesk.worldbank.org/knowledgebase/articles/378831-why-use-gni-per-capita-to-classify-economies-into. Accessed 10 November 2020
Teng F, He J, Pan X, Zhang C (2011) Metric of carbon equity: Carbon Gini index based on historical cumulative emission per capita. Adv Clim Chang Res 2(3):134–140
SAS S, Guide SUs (2014) SAS Institute, Cary, NC
Salk RH, Hyde JS, Abramson LY (2017) Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull 143(8):783
Franko DL, Keel PK (2006) Suicidality in eating disorders: occurrence, correlates, and clinical implications. Clin Psychol Rev 26(6):769–782
Vijayakumar L (2015) Suicide in women. Indian J Psychiatry 57(Suppl 2):S233
Cluver L, Orkin M, Boyes ME, Sherr L (2015) Child and adolescent suicide attempts, suicidal behavior, and adverse childhood experiences in South Africa: a prospective study. J Adolesc Health 57(1):52–59
Anum A, Adjorlolo S, Kugbey N (2019) Depressive symptomatology in adolescents in Ghana: examination of psychometric properties of the Patient Health Questionnaire-9. J Affect Disord 256:213–218
Salamanca-Buentello F, Seeman MV, Daar AS, Upshur RE (2020) The ethical, social, and cultural dimensions of screening for mental health in children and adolescents of the developing world. PLoS ONE 15(8):e0237853
Katz C, Bolton SL, Katz LY, Isaak C, Tilston-Jones T, Sareen J, Team SCSP (2013) A systematic review of school-based suicide prevention programs. Depression Anxiety 30(10):1030–1045
Griffiths F, Lindenmeyer A, Powell J, Lowe P, Thorogood M (2006) Why are health care interventions delivered over the internet? A systematic review of the published literature. J Med Internet Res 8(2):e10
Bastien CH, Vallières A, Morin CM (2001) Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2(4):297–307
Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S (2011) The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 168(12):1266–1277
Reynolds WM (1988) SIQ, Suicidal ideation questionnaire: Professional manual. Psychol Assess Resour 10(3)
Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I (2011) Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT). Am J Psychiatry 168(5):495–501
King CD, Joyce VW, Nash CC, Buonopane RJ, Black JM, Zuromski KL, Millner AJ (2021) Fear of sleep and sleep quality mediate the relationship between trauma exposure and suicide attempt in adolescents. J Psychiatr Res 135:243–247
Associate Minister of Health (2006) New Zealand suicide prevention strategy 2006–2016. Associate Minister of Health, Wellington, New Zealand
Guzmán E, Cha C, Ribeiro J, Franklin J (2019) Suicide risk around the world: a meta-analysis of longitudinal studies. Soc Psychiatry Psychiatr Epidemiol 54(12):1459–1470
Acknowledgements
The authors would like to thank the World Health Organization and United States Centers for Disease Control for making the GSHS datasets publicly available for analysis.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Jaclyn C. Kearns and Catherine R. Glenn contributed to the manuscript conceptualization. Data preparation, data analysis, and draft of the results were performed by Julie A. Kittel. Paige Schlagbaum assisted with the literature review. Wilfred R. Pigeon provided expert commentary on the conceptualization and interpretation of data. The first draft of the manuscript was written by Jaclyn C. Kearns and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that they have no potential or competing conflicts of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kearns, J.C., Kittel, J.A., Schlagbaum, P. et al. Worry-related sleep problems and suicidal thoughts and behaviors among adolescents in 88 low-, middle-, and high-income countries: an examination of individual- and country-level factors. Eur Child Adolesc Psychiatry 31, 1995–2011 (2022). https://doi.org/10.1007/s00787-021-01838-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-021-01838-y