Abstract
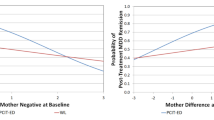
Whether effects of psychotherapies for depression are sustained after treatment is an important clinical issue. In older depressed children and adolescents such treatments have been shown to be sustained for several months. Rates of remission ranged from 62–69% at 3 months–1 year in one large scale study. To date there has been no data to inform whether the effects of earlier interventions for depression in the preschool period are sustained. To address this, we used data from a randomized controlled trial of a novel early intervention for depression called “Parent Child Interaction Therapy Emotion Development” (PCIT-ED) that has shown efficacy for depression, parenting stress and parenting practices. Participants and their caregivers were re-assessed 18 weeks after treatment completion. All study procedures were approved by the Washington University School of Medicine Internal Review Board prior to data collection. Study findings demonstrated a high rate of sustained gains in remission from depression, decreased parenting stress and parental depression 18 weeks after completion of a trial of PCIT-ED in a population of young children. Parental response to the child expression of emotion, a key treatment target drifted back towards baseline after 3 months. Relapse rates were 17% and predictors of relapse were the presence of an externalizing disorder, a higher number of co-morbid disorders and poorer guilt reparation and emotion regulation measured at treatment completion. This extends the body of literature demonstrating parent–child interaction therapy (PCIT) to have sustained effects on targeted disruptive symptom profiles to early childhood depression. This relatively low relapse rate after 18 weeks is comparable or better than many empirically proven treatments for depression in older children.

Similar content being viewed by others
References
Eckshtain D, Marchette LK, Schleider J, Evans S, Weisz JR (2019) Parental depressive symptoms as a predictor of outcome in the treatment of child internalizing and externalizing problems. J Abnorm Child Psychol 47(3):459–474
Weisz JR, McCarty CA, Valeri SM (2006) Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychol Bull 132(1):132–149. https://doi.org/10.1037/0033-2909.132.1.132
Forti-Buratti MA, Saikia R, Wilkinson EL, Ramchandani PG (2016) Psychological treatments for depression in pre-adolescent children (12 years and younger): systematic review and meta-analysis of randomised controlled trials. Eur Child Adolesc Psychiatry 25(10):1045–1054
Rith-Najarian LR, Mesri B, Park AL, Sun M, Chavira DA, Chorpita BF (2019) Durability of cognitive behavioral therapy effects for youth and adolescents with anxiety, depression, or traumatic stress: a meta-analysis on long-term follow-ups. Behav Ther 50(1):225–240
TfAwDS T (2009) The treatment for adolescents with depression study (TADS): outcomes over 1 year of naturalistic follow-up. Am J Psychiatry 166(10):1141–1149
Trowell J, Joffe I, Campbell J, Clemente C, Almqvist F, Soininen M, Koskenranta-Aalto U, Weintraub S, Kolaitis G, Tomaras V (2007) Childhood depression: a place for psychotherapy. Eur Child Adolesc Psychiatry 16(3):157–167
Birmaher B, Brent DA, Kolko D, Baugher M, Bridge J, Holder D, Iyengar S, Ulloa RE (2000) Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Arch Gen Psychiatry 57(1):29–36
Clarke G, Debar L, Lynch F, Powell J, Gale J, O'Connor E, Ludman E, Bush T, Lin EH, Von Korff M (2005) A randomized effectiveness trial of brief cognitive-behavioral therapy for depressed adolescents receiving antidepressant medication. J Am Acad Child Adolesc Psychiatry 44(9):888–898
Emslie GJ, Rush AJ, Weinberg WA, Kowatch RA, Carmody T, Mayes TL (1998) Fluoxetine in child and adolescent depression: acute and maintenance treatment. Depress Anxiety 7(1):32–39
Hardeveld F, Spijker J, De Graaf R, Nolen W, Beekman A (2010) Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand 122(3):184–191
Curry J, Silva S, Rohde P, Ginsburg G, Kratochvil C, Simons A, Kirchner J, May D, Kennard B, Mayes T (2011) Recovery and recurrence following treatment for adolescent major depression. Arch Gen Psychiatry 68(3):263–269
Matthews DD, Hammond WP, Nuru-Jeter A, Cole-Lewis Y, Melvin T (2013) Racial discrimination and depressive symptoms among African–American men: the mediating and moderating roles of masculine self-reliance and John Henryism. Psychol Men Masculinity 14(1):35
Eyberg S, Funderburk B (2011) Parent–child interaction therapy protocol. PCIT International Inc, Gainesville
Thomas R, Abell B, Webb HJ, Avdagic E, Zimmer-Gembeck MJ (2017) Parent–child interaction therapy: a meta-analysis. Pediatrics 140(3):e20170352
Brestan EV, Eyberg SM (1998) Effective psychosocial treatments of conduct-disordered children and adolescents: 29 years, 82 studies, and 5,272 kids. J Clin Child Psychol 27(2):180–189. https://doi.org/10.1207/s15374424jccp2702_5
Nixon RD, Sweeney L, Erickson DB, Touyz SW (2003) Parent-child interaction therapy: a comparison of standard and abbreviated treatments for oppositional defiant preschoolers. J Consult Clin Psychol 71(2):251
Hood KK, Eyberg SM (2003) Outcomes of parent-child interaction therapy: mothers' reports of maintenance three to six years after treatment. J Clin Child Adolesc Psychol 32(3):419–429. https://doi.org/10.1207/S15374424JCCP3203_10
Eyberg SM, Funderburk BW, Hembree-Kigin TL, McNeil CB, Querido JG, Hood KK (2001) Parent–child interaction therapy with behavior problem children: one and two year maintenance of treatment effects in the family. Child Family Behavior Therapy 23(4):1–20. https://doi.org/10.1300/J019v23n04_01
Boggs SR, Eyberg SM, Edwards DL, Rayfield A, Jacobs J, Bagner D, Hood KK (2005) Outcomes of parent-child interaction therapy: a comparison of treatment completers and study dropouts one to three years later. Child Fam Behav Ther 26(4):1–22
Abrahamse ME, Junger M, van Wouwe MA, Boer F, Lindauer RJ (2016) Treating child disruptive behavior in high-risk families: a comparative effectiveness trial from a community-based implementation. J Child Fam Stud 25(5):1605–1622
Choate ML, Pincus DB, Eyberg SM, Barlow DH (2005) Parent-child interaction therapy for treatment of separation anxiety disorder in young children: a pilot study. Cogn Behav Pract 12(1):126–135. https://doi.org/10.1016/S1077-7229(05)80047-1
Luby JL, Barch DM, Whalen D, Tillman R, Freedland KE (2018) A randomized controlled trial of parent-child psychotherapy targeting emotion development for early childhood depression. Am J Psychiatry 2018:18030321
Gaffrey MS, Luby JL (2012) Kiddie-Schedule for Affective Disorders and Schizophrenia—Early Childhood Version, 2012 Working Draft (KSADS-EC). Washington University School of Medicine, St. Louis
Achenbach TM (2001) Child behavior checklist for ages 6–18. University of Vermont, Burlington
Eyberg SM, Pincus D (1999) ECBI & SESBI-R : Eyberg child behavior inventory and sutter-Eyberg student behavior inventory-revised : professional manual. Psychological Assessment Resources, Odessa
Colvin A, Eyberg SM, Adams CD (1999) Restandardization of the Eyberg child behavior inventory
Luby JL, Heffelfinger A, Koenig-McNaught AL, Brown K, Spitznagel E (2004) The preschool feelings checklist: a brief and sensitive screening measure for depression in young children. J Am Acad Child Adolesc Psychiatry 43(6):708–717. https://doi.org/10.1097/01.chi.0000121066.29744.08
Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S (1983) A children’s global assessment scale (CGAS). Arch Gen Psychiatry 40(11):1228–1231
Busner J, Targum SD (2007) The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont) 4(7):28
Hodges K (1994) The preschool and early childhood functional assessment scale (PECFAS). Eastern Michigan University, Ypsilanti
Hodges K (2000) The child and adolescent functional assessment scale (CAFAS). Eastern Michigan University, Ypsilanti
Shields A, Cicchetti D (1997) Emotion regulation among school-age children: the development and validation of a new criterion Q-sort scale. Dev Psychol 33(6):906–916
Kochanska G (1992) My Child. University of Iowa, Iowa City
Bessmer JL, Brestan EV, Eyberg SM (2005) The dyadic parent-child interaction coding system II (DPICS II): reliability and validity with mother-child dyads. University of Florida
Fabes RA, Poulin RE, Eisenberg N, Madden-Derdich DA (2002) The Coping with Children's Negative Emotions Scale (CCNES): Psychometric properties and relations with children's emotional competence. Marriage Fam Rev
Robinson CC, Mandleco B, Olsen SF, Hart CH (2001) The Parenting Styles and Dimensions Questionnaire. In: Perlmutter BF, Touliatos J, Holden GW (eds) Handbook of family measurement techniques instruments & index, vol 3. SAGE, Thousand Oaks, pp 319–321
Beck AT, Steer RA, Brown GK (1996) Beck depression inventory-II. San Antonio 78(2):490–498
Abidin RR (1983) Parenting stress index : manual (PSI). Pediatric Psychology Press, Charlottesville
Luby JL, Barch DM, Whalen D, Tillman R, Freedland KE (2018) A randomized controlled trial of parent-child psychotherapy targeting emotion development for early childhood depression. Am J Psychiatry 175(11):1102–1110
Kennard BD, Emslie GJ, Mayes TL, Hughes JL (2006) Relapse and recurrence in pediatric depression. Child Adolescent Psychiatric Clin 15(4):1057–1079
Eyberg SM, Boggs S, Jaccard J (2014) Does maintenance treatment matter? J Abnorm Child Psychol 42(3):355–366
Luby JL, Si X, Belden AC, Tandon M, Spitznagel E (2009) Preschool depression: homotypic continuity and course over 24 months. Arch Gen Psychiatry 66(8):897–905. https://doi.org/10.1001/archgenpsychiatry.2009.97
Bufferd SJ, Dougherty LR, Carlson GA, Rose S, Klein DN (2012) Psychiatric disorders in preschoolers: continuity from ages 3 to 6. Am J Psychiatry 169(11):1157–1164. https://doi.org/10.1176/appi.ajp.2012.12020268
Wichstrøm L, Belsky J, Steinsbekk S (2017) Homotypic and heterotypic continuity of symptoms of psychiatric disorders from age 4 to 10 years: a dynamic panel model. J Child Psychol Psychiatry 58(11):1239–1247
Acknowledgements
We wish to thank our study population for their participation and the National Institutes of Mental Health for funding this study. This study was funded by NIMH R01 R01MH098454 to Drs. Luby and Barch.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Luby, J., Donohue, M.R., Gilbert, K. et al. Sustained remission of child depression despite drift in parent emotion management skills 18 weeks following Parent Child Interaction Therapy: emotion development. Eur Child Adolesc Psychiatry 30, 369–379 (2021). https://doi.org/10.1007/s00787-020-01522-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-020-01522-7