Abstract
Objectives
The aim of this in vitro study was to evaluate the sealing ability of combined application of iRoot BP Plus Root Repair Material (BP-RRM) and iRoot SP Injectable Root Canal Sealer (SP-RCS) for root-end filling.
Material and methods
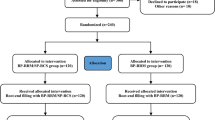
A total of 120 extracted human teeth were used in this study and were randomly divided into four groups. The BP-RRM+SP-RCS group included teeth retro-filled with combined use of BP-RRM and SP-RCS (n=45), and the BP-RRM group included teeth retro-filled by BP-RRM alone (n=45). Teeth without root-end preparation and filling were equally divided into positive control (n=15) and negative control (n=15). The apical sealing ability was evaluated by micro-CT analysis, dye penetrant examination, bacterial leakage test, and glucose leakage test.
Results
Micro-CT analysis showed that the total void fraction of BP-RRM+SP-RCS group was significantly lower than that of BP-RRM group, particularly at the coronal 1/3 segment of the retro-filled roots. Consistently, the maximum linear depth of dye leakage in BP-RRM+SP-RCS group was less than that of BP-RRM group. Bacterial leakage test showed that the microbial leakage in BP-RRM+SP-RCS group was significantly less than that in BP-RRM group. However, no significant difference in glucose leakage between BP-RRM+SP-RCS group and BP-RRM group was observed.
Conclusion
Combined use of BP-RRM and SP-RCS for root-end filling promotes apical sealing in vitro.
Clinical relevance
Combined use of BP-RRM and SP-RCS for root-end filling exhibited better apical sealing as compared to BP-RRM alone in vitro, and this may help reducing technical sensitivity and promoting clinical efficiency during endodontic microsurgery.




Similar content being viewed by others
References
Gomes B, Herrera DR (2018) Etiologic role of root canal infection in apical periodontitis and its relationship with clinical symptomatology. Braz Oral Res 32:e69. https://doi.org/10.1590/1807-3107bor-2018.vol32.0069
Karamifar K, Tondari A, Saghiri MA (2020) Endodontic periapical lesion: an overview on the etiology, diagnosis and current treatment modalities. Eur Endod J 5:54–67. https://doi.org/10.14744/eej.2020.42714
Siqueira JF Jr, Rôças IN, Ricucci D, Hülsmann M (2014) Causes and management of post-treatment apical periodontitis. Br Dent J 216:305–312. https://doi.org/10.1038/sj.bdj.2014.200
Floratos S, Kim S (2017) Modern endodontic microsurgery concepts: a clinical update. Dent Clin North Am 61:81–91. https://doi.org/10.1016/j.cden.2016.08.007
Song M, Nam T, Shin SJ, Kim E (2014) Comparison of clinical outcomes of endodontic microsurgery: 1 year versus long-term follow-up. J Endod 40:490–494. https://doi.org/10.1016/j.joen.2013.10.034
Setzer FC, Shah SB, Kohli MR, Karabucak B, Kim S (2010) Outcome of endodontic surgery: a meta-analysis of the literature--part 1: comparison of traditional root-end surgery and endodontic microsurgery. J Endod 36:1757–1765. https://doi.org/10.1016/j.joen.2010.08.007
von Arx T, Jensen SS, Hänni S, Friedman S (2012) Five-year longitudinal assessment of the prognosis of apical microsurgery. J Endod 38:570–579. https://doi.org/10.1016/j.joen.2012.02.002
Abusrewil SM, McLean W, Scott JA (2018) The use of bioceramics as root-end filling materials in periradicular surgery: a literature review. Saudi Dent J 30:273–282. https://doi.org/10.1016/j.sdentj.2018.07.004
Dawood AE, Parashos P, Wong RHK, Reynolds EC, Manton DJ (2017) Calcium silicate-based cements: composition, properties, and clinical applications. J Investig Clin Dent 8. https://doi.org/10.1111/jicd.12195
Zhou W, Zheng Q, Tan X, Song D, Zhang L, Huang D (2017) Comparison of mineral trioxide aggregate and iRoot BP Plus root repair material as root-end filling materials in endodontic microsurgery: a prospective randomized controlled study. J Endod 43:1–6. https://doi.org/10.1016/j.joen.2016.10.010
Jung J, Kim S, Kim E, Shin SJ (2020) Volume of voids in retrograde filling: comparison between calcium silicate cement alone and combined with a calcium silicate-based sealer. J Endod 46:97–102. https://doi.org/10.1016/j.joen.2019.10.015
Öğütlü F, Karaca İ (2018) Clinical and radiographic outcomes of apical surgery: a clinical study. J Maxillofac Oral Surg 17:75–83. https://doi.org/10.1007/s12663-017-1008-9
von Arx T, Jensen SS, Janner SFM, Hänni S, Bornstein MM (2019) A 10-year follow-up study of 119 teeth treated with apical surgery and root-end filling with mineral trioxide aggregate. J Endod 45:394–401. https://doi.org/10.1016/j.joen.2018.12.015
Song M, Kim SG, Lee SJ, Kim B, Kim E (2013) Prognostic factors of clinical outcomes in endodontic microsurgery: a prospective study. J Endod 39:1491–1497. https://doi.org/10.1016/j.joen.2013.08.026
von Arx T, Peñarrocha M, Jensen S (2010) Prognostic factors in apical surgery with root-end filling: a meta-analysis. J Endod 36:957–973. https://doi.org/10.1016/j.joen.2010.02.026
Chybowski EA, Glickman GN, Patel Y, Fleury A, Solomon E, He J (2018) Clinical outcome of non-surgical root canal treatment using a single-cone technique with endosequence bioceramic sealer: a retrospective analysis. J Endod 44:941–945. https://doi.org/10.1016/j.joen.2018.02.019
Roizenblit RN, Soares FO, Lopes RT, Dos Santos BC, Gusman H (2020) Root canal filling quality of mandibular molars with EndoSequence BC and AH Plus sealers: A micro-CT study. Aust Endod J 46:82–87. https://doi.org/10.1111/aej.12373
Jafari F, Jafari S (2017) Composition and physicochemical properties of calcium silicate based sealers: A review article. J Clin Exp Dent 9:e1249–e1255. https://doi.org/10.4317/jced.54103
Donnermeyer D, Bürklein S, Dammaschke T, Schäfer E (2019) Endodontic sealers based on calcium silicates: a systematic review. Odontology 107:421–436. https://doi.org/10.1007/s10266-018-0400-3
Donnermeyer D, Schemkämper P, Bürklein S, Schäfer E (2022) Short and long-term solubility, alkalizing effect, and thermal persistence of premixed calcium silicate-based sealers: AH plus bioceramic sealer vs. total fill BC sealer. Materials (Basel) 15. https://doi.org/10.3390/ma15207320
Silva E, Cardoso ML, Rodrigues JP, De-Deus G, Fidalgo T (2021) Solubility of bioceramic- and epoxy resin-based root canal sealers: a systematic review and meta-analysis. Aust Endod J 47:690–702. https://doi.org/10.1111/aej.12487
Rencher B, Chang AM, Fong H, Johnson JD, Paranjpe A (2021) Comparison of the sealing ability of various bioceramic materials for endodontic surgery. Restor Dent Endod 46:e35. https://doi.org/10.5395/rde.2021.46.e35
Shinbori N, Grama AM, Patel Y, Woodmansey K, He J (2015) Clinical outcome of endodontic microsurgery that uses EndoSequence BC root repair material as the root-end filling material. J Endod 41:607–612. https://doi.org/10.1016/j.joen.2014.12.028
Chan S, Glickman GN, Woodmansey KF, He J (2020) Retrospective analysis of root-end microsurgery outcomes in a postgraduate program in endodontics using calcium silicate-based cements as root-end filling materials. J Endod 46:345–351. https://doi.org/10.1016/j.joen.2019.11.010
Liao WC, Lee YL, Tsai YL et al (2019) Outcome assessment of apical surgery: a study of 234 teeth. J Formos Med Assoc 118:1055–1061. https://doi.org/10.1016/j.jfma.2018.10.019
Sarnadas M, Marques JA, Baptista IP, Santos JM (2021) Impact of periodontal attachment loss on the outcome of endodontic microsurgery: a systematic review and meta-analysis. Medicina (Kaunas) 57. https://doi.org/10.3390/medicina57090922
Yoo YJ, Kim DW, Perinpanayagam H et al (2020) Prognostic factors of long-term outcomes in endodontic microsurgery: a retrospective cohort study over five years. J Clin Med 9. https://doi.org/10.3390/jcm9072210
Chen YY, Pradan SP, Yang JB (2021) A retrospective study of endodontic microsurgery about 302 patients. Hua Xi Kou Qiang Yi Xue Za Zhi 39:458–463. https://doi.org/10.7518/hxkq.2021.04.013
Kim D, Lee H, Chung M, Kim S, Song M, Kim E (2020) Effects of fast- and slow-setting calcium silicate-based root-end filling materials on the outcome of endodontic microsurgery: a retrospective study up to 6 years. Clin Oral Investig 24:247–255. https://doi.org/10.1007/s00784-019-02937-6
Safi C, Kohli MR, Kratchman SI, Setzer FC, Karabucak B (2019) Outcome of endodontic microsurgery using mineral trioxide aggregate or root repair material as root-end filling material: a randomized controlled trial with cone-beam computed tomographic evaluation. J Endod 45:831–839. https://doi.org/10.1016/j.joen.2019.03.014
Džanković A, Hadžiabdić N, Korać S, Tahmiščija I, Konjhodžić A, Hasić-Branković L (2020) Sealing ability of mineral trioxide aggregate, biodentine and glass ionomer as root-end materials: a question of choice. Acta Med Acad 49:232–239. https://doi.org/10.5644/ama2006-124.312
Eskandarinezhad M, Shahveghar-Asl N, Sharghi R et al (2017) Sealing efficacy of mineral trioxide aggregate with and without nanosilver for root end filling: an in vitro bacterial leakage study. J Clin Exp Dent 9:e27–e33. https://doi.org/10.4317/jced.53070
Xu Q, Fan MW, Fan B, Cheung GS, Hu HL (2005) A new quantitative method using glucose for analysis of endodontic leakage. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99:107–111. https://doi.org/10.1016/j.tripleo.2004.06.006
Barthel CR, Moshonov J, Shuping G, Orstavik D (1999) Bacterial leakage versus dye leakage in obturated root canals. Int Endod J 32:370–375. https://doi.org/10.1046/j.1365-2591.1999.00235.x
De-Deus G, Petruccelli V, Gurgel-Filho E, Coutinho-Filho T (2006) MTA versus Portland cement as repair material for furcal perforations: a laboratory study using a polymicrobial leakage model. Int Endod J 39:293–298. https://doi.org/10.1111/j.1365-2591.2006.01096.x
Torabinejad M, Rastegar AF, Kettering JD, Pitt Ford TR (1995) Bacterial leakage of mineral trioxide aggregate as a root-end filling material. J Endod 21:109–112. https://doi.org/10.1016/s0099-2399(06)80433-4
Taschieri S, Bettach R, Lolato A, Moneghini L, Fabbro MD (2011) Endodontic surgery failure: SEM analysis of root-end filling. J Oral Sci 53:393–396. https://doi.org/10.2334/josnusd.53.393
Kohli MR, Berenji H, Setzer FC, Lee SM, Karabucak B (2018) Outcome of endodontic surgery: a meta-analysis of the literature-part 3: comparison of endodontic microsurgical techniques with 2 different root-end filling materials. J Endod 44:923–931. https://doi.org/10.1016/j.joen.2018.02.021
Setzer F, Harley M, Cheung J, Karabucak B (2021) Possible causes for failure of endodontic surgery - a retrospective series of 20 resurgery cases. Eur Endod J 6:235–241. https://doi.org/10.14744/eej.2021.14238
Kruse C, Spin-Neto R, Christiansen R, Wenzel A, Kirkevang LL (2016) Periapical bone healing after apicectomy with and without retrograde root filling with mineral trioxide aggregate: a 6-year follow-up of a randomized controlled trial. J Endod 42:533–537. https://doi.org/10.1016/j.joen.2016.01.011
Pinto D, Marques A, Pereira JF, Palma PJ, Santos JM (2020) Long-term prognosis of endodontic microsurgery-a systematic review and meta-analysis. Medicina (Kaunas) 56. https://doi.org/10.3390/medicina56090447
von Arx T, Janner SFM, Haenni S, Bornstein MM (2020) Bioceramic root repair material (BCRRM) for root-end obturation in apical surgery. An analysis of 174 teeth after 1 year. Swiss Dent J 130:390–396
Song W, Li S, Tang Q, Chen L, Yuan Z (2021) In vitro biocompatibility and bioactivity of calcium silicate-based bioceramics in endodontics (Review). Int J Mol Med 48. https://doi.org/10.3892/ijmm.2021.4961
Kim SY, Kim HC, Shin SJ, Kim E (2018) Comparison of gap volume after retrofilling using 4 different filling materials: evaluation by micro-computed tomography. J Endod 44:635–638. https://doi.org/10.1016/j.joen.2017.11.009
Jardine AP, Rosa KFV, Matoso FB, Quintana RM, Grazziotin-Soares R, Kopper PMP (2021) Marginal gaps and internal voids after root-end filling using three calcium silicate-based materials: A Micro-CT analysis. Braz Dent J 32:1–7. https://doi.org/10.1590/0103-6440202104096
Celikten B, Jacobs R, de Faria VK et al (2019) Comparative evaluation of cone beam CT and micro-CT on blooming artifacts in human teeth filled with bioceramic sealers. Clin Oral Investig 23:3267–3273. https://doi.org/10.1007/s00784-018-2748-8
Veríssimo DM, do Vale MS (2006) Methodologies for assessment of apical and coronal leakage of endodontic filling materials: a critical review. J Oral Sci 48: 93-98. https://doi.org/10.2334/josnusd.48.93
Camps J, Pashley D (2003) Reliability of the dye penetration studies. J Endod 29:592–594. https://doi.org/10.1097/00004770-200309000-00012
Barbosa-Ribeiro M, Arruda-Vasconcelos R, Mendes Louzada L et al (2020) Microbiological investigation in teeth with persistent/secondary endodontic infection in different stages of root canal retreatment. Eur Endod J 5:219–225. https://doi.org/10.14744/eej.2020.73626
Barbosa-Ribeiro M, Arruda-Vasconcelos R, Louzada LM, Dos Santos DG, Andreote FD, Gomes B (2021) Microbiological analysis of endodontically treated teeth with apical periodontitis before and after endodontic retreatment. Clin Oral Investig 25:2017–2027. https://doi.org/10.1007/s00784-020-03510-2
de Almeida J, Pimenta AL, Felippe WT (2015) A laboratory assessment of bacterial leakage in MTA apical plugs exposed to phosphate-buffered saline. Acta Odontol Latinoam 28:144–148. https://doi.org/10.1590/s1852-48342015000200008
Medeiros PL, Bernardineli N, Cavenago BC et al (2016) Sealing ability of MTA, CPM, and MBPc as root-end filling materials: a bacterial leakage study. J Appl Oral Sci 24:148–152. https://doi.org/10.1590/1678-775720130103
Gandhi B, Halebathi-Gowdra R (2017) Comparative evaluation of the apical sealing ability of a ceramic based sealer and MTA as root-end filling materials - an in-vitro study. J Clin Exp Dent 9:e901–e905. https://doi.org/10.4317/jced.53903
Shahriari S, Faramarzi F, Alikhani MY, Farhadian M, Hendi SS (2016) Apical sealing ability of mineral trioxide aggregate, intermediate restorative material and calcium enriched mixture cement: a bacterial leakage study. Iran Endod J 11:336–340. https://doi.org/10.22037/iej.2016.16
Savadkouhi ST, Bakhtiar H, Ardestani SE (2016) In vitro and ex vivo microbial leakage assessment in endodontics: a literature review. J Int Soc Prev Community Dent 6:509–516. https://doi.org/10.4103/2231-0762.195516
Hegde V, Arora S (2015) Sealing ability of three hydrophilic single-cone obturation systems: an in vitro glucose leakage study. Contemp Clin Dent 6:S86–S89. https://doi.org/10.4103/0976-237x.152953
Sudan PS, Samson EP, Kukreja MK, Khan M, Misurya R, Ismail PMS (2018) A comparative evaluation of apical leakage using three root canal sealants: an in vitro study. J Contemp Dent Pract 19:955–958
Qu ZZ, Li XG, Wang Q (2016) Study of dental apex sealing effects after post space. Shanghai Kou Qiang Yi Xue 25:560–565
Jafari F, Jafari S (2017) Importance and methodologies of endodontic microleakage studies: a systematic review. J Clin Exp Dent 9:e812–e819. https://doi.org/10.4317/jced.53604
Shemesh H, Souza EM, Wu MK, Wesselink PR (2008) Glucose reactivity with filling materials as a limitation for using the glucose leakage model. Int Endod J 41:869–872. https://doi.org/10.1111/j.1365-2591.2008.01440.x
Jafari F, Rahimi S, Shahi S, Jafari S (2017) Endodontic microleakage studies: correlation among different methods, clinical relevance, and potential laboratory errors. Minerva Stomatol 66:169–177. https://doi.org/10.23736/s0026-4970.17.04013-4
Arx TV, Bosshardt D, Bingisser AC, Bornstein MM (2018) Endoscopic evaluation of cut root faces and histologic analysis of removed apices following root resection: a clinical study. Eur Endod J 3:18–23. https://doi.org/10.5152/eej.2017.17046
Yoon J, Cho BH, Bae J, Choi Y (2018) Anatomical analysis of the resected roots of mandibular first molars after failed non-surgical retreatment. Restor Dent Endod 43:e16. https://doi.org/10.5395/rde.2018.43.e16
Funding
This work was supported by a grant from the Science & Technology Department of Sichuan Province (2021YFQ0064).
Author information
Authors and Affiliations
Contributions
X.X. conceived the ideas; X.D. performed all the experimental procedures and analyzed the data; X.D., Q.X., and X.X. managed the writing of the manuscript. All the authors reviewed the manuscript critically.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of the West China Hospital of Stomatology, Chengdu, China (WCHSIRB-D-2022-202).
Informed consent
Informed consent was obtained from the patients who had teeth extracted for orthodontic reasons.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, X., Xie, Q. & Xu, X. In vitro evaluation of the sealing ability of combined use of iRoot BP Plus and iRoot SP for root-end filling. Clin Oral Invest 27, 2969–2977 (2023). https://doi.org/10.1007/s00784-023-04896-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04896-5