Abstract
Objective
Due to inconsistent findings in limited previous cohort studies, the aim of this study was to estimate the obesity effect on periodontitis progression in Thai adults.
Materials and methods
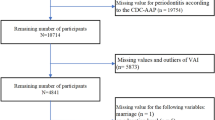
This 10-year retrospective cohort study comprised 2216 employees of the Electric Generation Authority of Thailand (EGAT). Their demographic, medical, and periodontal status was collected. Subjects with periodontitis progression were defined as having ≥ 2 teeth with progression. Additional proximal clinical attachment loss ≥ 3 mm or tooth loss with severe periodontitis at baseline were used to identify disease progression at the tooth level. Central obesity was classified using the waist-hip ratio. Multi-level Poisson regression was used to determine the effect of obesity on periodontitis progression by adjusting for age, sex, education, income, smoking, alcohol drinking, exercise, diabetes mellitus, and hypertension.
Results
The cumulative incidence of periodontitis progression during the 10-year period was 59.6 cases per 100 persons (95% CI: 57.5, 61.6). The univariate analysis indicated that obese subjects had 15% higher risk of progression than that of healthy subjects. However, when confounders were analyzed simultaneously, the effect of obesity was not significant with a risk ratio of 0.98 (95% CI: 0.88, 1.08).
Conclusions
Despite the higher incidence of disease progression in the obese, obesity is not an independent risk factor for periodontitis progression.
Clinical relevance
Obesity and periodontitis progression share many common risk factors. Using the obesity as a preliminary screening for periodontitis progression may be an alternative prevention protocol.
Similar content being viewed by others
References
Haslam DW, James WP (2005) Obesity Lancet 366:1197–1209. https://doi.org/10.1016/s0140-6736(05)67483-1
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A et al (2017) Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 377:13–27. https://doi.org/10.1056/NEJMoa1614362
Kotsis V, Jordan J, Micic D, Finer N, Leitner DR, Toplak H et al (2018) Obesity and cardiovascular risk: a call for action from the European society of hypertension working group of obesity, diabetes and the high-risk patient and European association for the study of obesity: part A: mechanisms of obesity induced hypertension, diabetes and dyslipidemia and practice guidelines for treatment. J Hypertens 36:1427–1440. https://doi.org/10.1097/hjh.0000000000001730
Khader Y, Batieha A, Jaddou H, El-Khateeb M, Ajlouni K (2019) The performance of anthropometric measures to predict diabetes mellitus and hypertension among adults in Jordan. BMC Public Health 19:1416. https://doi.org/10.1186/s12889-019-7801-2
Hopkins BD, Goncalves MD, Cantley LC (2016) Obesity and cancer mechanisms: cancer metabolism. J Clin Oncol 34:4277–4283. https://doi.org/10.1200/jco.2016.67.9712
Kornman KS (2008) Mapping the pathogenesis of periodontitis: a new look. J Periodontol 79:1560–1568. https://doi.org/10.1902/jop.2008.080213
Fain JN, Madan AK, Hiler ML, Cheema P, Bahouth SW (2004) Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans. Endocrinology 145:2273–2282. https://doi.org/10.1210/en.2003-1336
Hajishengallis G, Lamont RJ (2012) Beyond the red complex and into more complexity: the polymicrobial synergy and dysbiosis (PSD) model of periodontal disease etiology. Mol Oral Microbiol 27:409–419. https://doi.org/10.1111/j.2041-1014.2012.00663.x
Martinez-Herrera M, Silvestre-Rangil J, Silvestre FJ (2017) Association between obesity and periodontal disease. A systematic review of epidemiological studies and controlled clinical trials. Med Oral Patol Oral Cir Bucal 22:e708–e715. https://doi.org/10.4317/medoral.21786
Genco RJ, Grossi SG, Ho A, Nishimura F, Murayama Y (2005) A proposed model linking inflammation to obesity, diabetes, and periodontal infections. J Periodontol 76:2075–2084
Jimenez M, Hu FB, Marino M, Li Y, Joshipura KJ (2012) Prospective associations between measures of adiposity and periodontal disease. Obesity 20:1718–1725. https://doi.org/10.1038/oby.2011.291
Gorman A, Kaye EK, Apovian C, Fung TT, Nunn M, Garcia RI (2012) Overweight and obesity predict time to periodontal disease progression in men. J Clin Periodontol 39:107–114. https://doi.org/10.1111/j.1600-051X.2011.01824.x
Saxlin T, Ylostalo P, Suominen-Taipale L, Aromaa A, Knuuttila M (2010) Overweight and obesity weakly predict the development of periodontal infection. J Clin Periodontol 37:1059–1067. https://doi.org/10.1111/j.1600-051X.2010.01633.x
Vathesatogkit P, Woodward M, Tanomsup S, Ratanachaiwong W, Vanavanan S, Yamwong S et al (2012) Cohort profile: the electricity generating authority of Thailand study. Int J Epidemiol 41:359–365. https://doi.org/10.1093/ije/dyq218
Lertpimonchai A, Rattanasiri S, Tamsailom S, Champaiboon C, Ingsathit A, Kitiyakara C et al (2019) Periodontitis as the risk factor of chronic kidney disease: mediation analysis. J Clin Periodontol 46:631–639. https://doi.org/10.1111/jcpe.13114
Tonetti MS, Claffey N (2005) Advances in the progression of periodontitis and proposal of definitions of a periodontitis case and disease progression for use in risk factor research. Group C consensus report of the 5th European Workshop in Periodontology. J Clin Periodontol 32(Suppl 6):210–3. https://doi.org/10.1111/j.1600-051X.2005.00822.x
Chalmers J, MacMahon S, Mancia G, Whitworth J, Beilin L, Hansson L et al (1999) 1999 World Health Organization-International Society of Hypertension Guidelines for the management of hypertension. Guidelines sub-committee of the World Health Organization. Clin Exp Hypertens 21:1009–1060. https://doi.org/10.3109/10641969909061028
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Clin Periodontol 45(Suppl 20):S149-s161. https://doi.org/10.1111/jcpe.12945
Ortigara GB, Mário Ferreira TG, Tatsch KF, Romito GA, Ardenghi TM, Sfreddo CS et al (2021) The 2018 EFP/AAP periodontitis case classification demonstrates high agreement with the 2012 CDC/AAP criteria. J Clin Periodontol. https://doi.org/10.1111/jcpe.13462
Germen M, Baser U, Lacin CC, Fıratlı E, İşsever H, Yalcin F (2021) Periodontitis prevalence, severity, and risk factors: a comparison of the AAP/CDC case definition and the EFP/AAP classification. Int J Environ Res Public Health 18(7):3459. https://doi.org/10.3390/ijerph18073459
Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ (2012) Update of the case definitions for population-based surveillance of periodontitis. J Periodontol 83:1449–1454. https://doi.org/10.1902/jop.2012.110664
Ogawa H, Yoshihara A, Hirotomi T, Ando Y, Miyazaki H (2002) Risk factors for periodontal disease progression among elderly people. J Clin Periodontol 29:592–597. https://doi.org/10.1034/j.1600-051X.2002.290702.x
Lindhe J, Nyman S (1984) Long-term maintenance of patients treated for advanced periodontal disease. J Clin Periodontol 11:504–514. https://doi.org/10.1111/j.1600-051x.1984.tb00902.x
Brambilla P, Bedogni G, Moreno LA, Goran MI, Gutin B, Fox KR et al (2006) Crossvalidation of anthropometry against magnetic resonance imaging for the assessment of visceral and subcutaneous adipose tissue in children. Int J Obes 30:23–30. https://doi.org/10.1038/sj.ijo.0803163
Chen CC, Wang WS, Chang HY, Liu JS, Chen YJ (2009) Heterogeneity of body mass index, waist circumference, and waist-to-hip ratio in predicting obesity-related metabolic disorders for Taiwanese aged 35–64 y. Clin Nutr 28:543–548. https://doi.org/10.1016/j.clnu.2009.04.017
Chen YM, Ho SC, Lam SS, Chan SS (2006) Validity of body mass index and waist circumference in the classification of obesity as compared to percent body fat in Chinese middle-aged women. Int J Obes 30:918–925. https://doi.org/10.1038/sj.ijo.0803220
Cheng CH, Ho CC, Yang CF, Huang YC, Lai CH, Liaw YP (2010) Waist-to-hip ratio is a better anthropometric index than body mass index for predicting the risk of type 2 diabetes in Taiwanese population. Nutr Res 30:585–593. https://doi.org/10.1016/j.nutres.2010.08.007
Huxley R, Mendis S, Zheleznyakov E, Reddy S, Chan J (2010) Body mass index, waist circumference and waist:hip ratio as predictors of cardiovascular risk–a review of the literature. Eur J Clin Nutr 64:16–22. https://doi.org/10.1038/ejcn.2009.68
Neovius M, Linné Y, Rossner S (2005) BMI, waist-circumference and waist-hip-ratio as diagnostic tests for fatness in adolescents. Int J Obes 29:163–169. https://doi.org/10.1038/sj.ijo.0802867
Oka R, Miura K, Sakurai M, Nakamura K, Yagi K, Miyamoto S et al (2009) Comparison of waist circumference with body mass index for predicting abdominal adipose tissue. Diabetes Res Clin Pract 83:100–105. https://doi.org/10.1016/j.diabres.2008.10.001
Parikh RM, Joshi SR, Menon PS, Shah NS (2007) Index of central obesity - a novel parameter. Med Hypotheses 68:1272–1275. https://doi.org/10.1016/j.mehy.2006.10.038
Yamborisut U, Kijboonchoo K, Wimonpeerapattana W, Srichan W, Thasanasuwan W (2008) Study on different sites of waist circumference and its relationship to weight-for-height index in Thai adolescents. J Med Assoc Thai 91:1276–1284
Yang F, Lv JH, Lei SF, Chen XD, Liu MY, Jian WX et al (2006) Receiver-operating characteristic analyses of body mass index, waist circumference and waist-to-hip ratio for obesity: screening in young adults in central south of China. Clin Nutr 25:1030–1039. https://doi.org/10.1016/j.clnu.2006.04.009
Rothman KJ (2008) BMI-related errors in the measurement of obesity. Int J Obes 32(Suppl 3):S56–S59. https://doi.org/10.1038/ijo.2008.87
World Health Organization (2011) Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8–11 December 2008. WHO Document Production Services, Geneva, Switzerland
Yang H, Xin Z, Feng JP, Yang JK (2017) Waist-to-height ratio is better than body mass index and waist circumference as a screening criterion for metabolic syndrome in Han Chinese adults. Medicine 96:e8192. https://doi.org/10.1097/md.0000000000008192
Lee HJ, Hwang SY, Hong HC, Ryu JY, Seo JA, Kim SG et al (2015) Waist-to-hip ratio is better at predicting subclinical atherosclerosis than body mass index and waist circumference in postmenopausal women. Maturitas 80:323–328. https://doi.org/10.1016/j.maturitas.2014.12.015
Lertpimonchai A, Rattanasiri S, Arj-Ong Vallibhakara S, Attia J, Thakkinstian A (2017) The association between oral hygiene and periodontitis: a systematic review and meta-analysis. Int Dent J 67:332–343. https://doi.org/10.1111/idj.12317
Acknowledgements
We thank Assoc.Prof. Suphot Tamsailom and Assist.Prof. Kanoknadda Tavedhikul for their advice in study design and data interpretation, Dr. Kevin Tompkins for language editing, and Assoc.Prof. Kitti Torrungruang for periodontal data management in EGAT2/2. We also thank Nisakron Thongmung for organizing the survey and managing the medical data.
Funding
This research was financially supported by Chulalongkorn University.
Author information
Authors and Affiliations
Contributions
Apinun Charupinijkul, Sirikarn Arunyanak and Attawood Lertpimonchai made substantial contributions to the conception and design of the study. Prin Vathesatogkit, Sirikarn Arunyanak, Attawood Lertpimonchai, and Lalitsara Thienpramuk performed the field survey and data collection. Apinun Charupinijkul, Sirikarn Arunyanak, Sasivimol Rattanasiri, and Attawood Lertpimonchai performed data analysis and data interpretation. Apinun Charupinijkul, Sirikarn Arunyanak, and Attawood Lertpimonchai drafted the article and critical revision critically. All authors have given final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by The Ethics Committee of the Faculty of Dentistry, Chulalongkorn University (HREC-DCU 2020–019).
Informed consent
Informed consent was obtained from every subject in the study.
Conflict of interest
The authors declares no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Charupinijkul, A., Arunyanak, S., Rattanasiri, S. et al. The effect of obesity on periodontitis progression: the 10-year retrospective cohort study. Clin Oral Invest 26, 535–542 (2022). https://doi.org/10.1007/s00784-021-04031-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04031-2