Abstract
Objectives
Salivary glands are affected during radiotherapy in the head and neck region, leading to a reduction in salivary flow and changes its composition. Besides negatively affecting the oral soft tissues, this can also lead to dental impairment. Thus, we evaluated the effect of radiotherapy in the proteomic profile of the saliva in patients with head and neck cancer (HNC).
Materials and methods
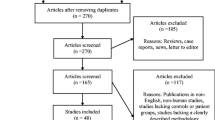
HNC patients had their saliva collected before (BRT), during (2–5 weeks; DRT), and after (3–4 months; ART) radiotherapy. Saliva was also collected from healthy volunteers (control; C). Samples were processed for proteomic analysis.
Results
In total, 1055 proteins were identified, among which 46 were common to all groups, while 86, 86, 286, and 395 were exclusively found in C, BRT, DRT, and ART, respectively. Remarkably, alpha-enolase was increased 35-fold DRT compared with BRT, while proline-rich proteins were decreased. ART there was a 16-fold increase in scaffold attachment factor-B1 and a 3-fold decrease in alpha-enolase and several cystatins. When compared with C, salivary proteins of BRT patients showed increases cystatin-C, lysozyme C, histatin-1, and proline-rich proteins
Conclusion/clinical revelance
Both HNC and radiotherapy remarkably change the salivary protein composition. Altogether, our results, for the first time, suggest investigating alpha-enolase levels in saliva DRT in future studies as a possible biomarker and strategy to predict the efficiency of the treatment. Moreover, our data provide important insights for designing dental products that are more effective for these patients and contribute to a better understanding of the progressive changes in salivary proteins induced by radiotherapy.

Graphical abstract



Similar content being viewed by others
References
Safdari Y, Khalili M, Farajnia S, Asgharzadeh M, Yazdani Y, Sadeghi M (2014) Recent advances in head and neck squamous cell carcinoma--a review. Clin Biochem 47(13-14):1195–1202. https://doi.org/10.1016/j.clinbiochem.2014.05.066
Leemans CR, Braakhuis BJ, Brakenhoff RH (2011) The molecular biology of head and neck cancer. Nat Rev Cancer 11(1):9–22. https://doi.org/10.1038/nrc2982
Cruz FO, Ferreira EB, Vasques CI, Mata LR, Reis PE (2016) Validation of an educative manual for patients with head and neck cancer submitted to radiation therapy. Rev Lat Am Enfermagem:24. https://doi.org/10.1590/1518-8345.0949.2706
Soulieres D, Faivre S, Mesia R, Remenar E, Li SH, Karpenko A, Dechaphunkul A, Ochsenreither S, Kiss LA, Lin JC, Nagarkar R, Tamas L, Kim SB, Erfan J, Alyasova A, Kasper S, Barone C, Turri S, Chakravartty A, Chol M, Aimone P, Hirawat S, Licitra L (2017) Buparlisib and paclitaxel in patients with platinum-pretreated recurrent or metastatic squamous cell carcinoma of the head and neck (BERIL-1): a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Oncol 18:323–335. https://doi.org/10.1016/S1470-2045(17)30064-5
Zago SD (2006) The radiotherapy effect on the quality of life of patients with head and neck cancer. Revista Brasileira de Cancerologia 52(4):323–329
Mira JG, Fullerton GD, Wescott WB (1982) Correlation between initial salivary flow rate and radiation dose in the production of xerostomia. Acta Radiol Oncol 21(3):151–154
Makkonen T (1988) Studies on oral complications of head and neck cancer radiotherapy. Proc Finn Dent Soc 84(Suppl 4-5):1–111
Chencharick JD, Mossman KL (1983) Nutritional consequences of the radiotherapy of head and neck cancer. Cancer. 51(5):811–815. https://doi.org/10.1002/1097-0142(19830301)51:5<811::aid-cncr2820510511>3.0.co;2-m
Specht L (2002) Oral complications in the head and neck radiation patient. Introduction and scope of the problem. Support Care Cancer 10(1):36–39
Murad AM KA (1996) Oncologia: bases clínicas do tratamento. Rio de Janeiro: Guanabara Koogan;. 1.ed
Jham BC, da Silva Freire AR (2006) Oral complications of radiotherapy in the head and neck. Braz J Otorhinolaryngol 72(5):704–708. https://doi.org/10.1016/s1808-8694(15)31029-6
Shyh-An Yeh MD (2010) Radiotherapy for head and neck cancer. Semin Plast Surg 24(2):127–136
Ventura T, Cassiano LPS, Souza ESCM, Taira EA, Leite AL, Rios D, Buzalaf MAR (2017) The proteomic profile of the acquired enamel pellicle according to its location in the dental arches. Arch Oral Biol 79:20–29. https://doi.org/10.1016/j.archoralbio.2017.03.001
Winck FV, Prado Ribeiro AC, Ramos Domingues R, Ling LY, Riano-Pachon DM, Rivera C, Brandao TB, Gouvea AF, Santos-Silva AR, Coletta RD, Paes Leme AF (2015) Insights into immune responses in oral cancer through proteomic analysis of saliva and salivary extracellular vesicles. Sci Rep 5:16305. https://doi.org/10.1038/srep16305
Ventura T, Ribeiro NR, Dionizio AS, Sabino IT, Buzalaf MAR (2018) Standardization of a protocol for shotgun proteomic analysis of saliva. J Appl Oral Sci 26:e20170561. https://doi.org/10.1590/1678-7757-2017-0561
Delmonico L, Bravo M, Silvestre RT, Ornellas MH, De Azevedo CM, Alves G (2016) Proteomic profile of saliva and plasma from women with impalpable breast lesions. Oncol Lett 12(3):2145–2152. https://doi.org/10.3892/ol.2016.4828
Jasim H, Olausson P, Hedenberg-Magnusson B, Ernberg M, Ghafouri B (2016) The proteomic profile of whole and glandular saliva in healthy pain-free subjects. Sci Rep 6:39073. https://doi.org/10.1038/srep39073
Penteado CAS, Batista TBD, Chaiben CL, Bonacin BG, Ventura TMO, Dionizio A, Couto Souza PH, Buzalaf MAR, Azevedo-Alanis LR (2020) Salivary protein candidates for biomarkers of oral disorders in alcohol and tobacco dependents. Oral Dis 26:1200–1208. https://doi.org/10.1111/odi.13337
Dawes C (1972) Circadian rhythms in human salivary flow rate and composition. J Physiol 220(3):529–545
Taira EA, Ventura TMS, Cassiano LPS, Silva CMS, Martini T, Leite AL, Rios D, Magalhaes AC, Buzalaf MAR (2018) Changes in the proteomic profile of acquired enamel pellicles as a function of their time of formation and hydrochloric acid exposure. Caries Res 52(5):367–377. https://doi.org/10.1159/000486969
Van De Wiele C, Signore A, Scopinaro F, Waterhouse R, Dierckx RA, Imitt (2001) Imaging tumour hypoxia: where are we? Nucl Med Commun 22(9):945–947
Buzalaf MA, Hannas AR, Kato MT (2012) Saliva and dental erosion. J Appl Oral Sci 20(5):493–502. https://doi.org/10.1590/s1678-77572012000500001
Shannon IL, Starcke EN, Wescott WB (1977) Effect of radiotherapy on whole saliva flow. J Dent Res 56(6):693–693. https://doi.org/10.1177/00220345770560062201
Dirix P, Nuyts S, Van den Bogaert W (2006) Radiation-induced xerostomia in patients with head and neck cancer: a literature review. Cancer. 107(11):2525–2534. https://doi.org/10.1002/cncr.22302
Vissink A, Mitchell JB, Baum BJ, Limesand KH, Jensen SB, Fox PC, Elting LS, Langendijk JA, Coppes RP, Reyland ME (2010) Clinical management of salivary gland hypofunction and xerostomia in head-and-neck cancer patients: successes and barriers. Int J Radiat Oncol Biol Phys 78(4):983–991. https://doi.org/10.1016/j.ijrobp.2010.06.052
Cowman RA, Baron SS, Glassman AH, Davis ME, Strosberg AM (1983) Changes in protein-composition of saliva from radiation-induced xerostomia patients and its effect on growth of oral Streptococci. Journal of Dental Research 62(3):336–340. https://doi.org/10.1177/00220345830620030601
Funegard U, Franzen L, Ericson T, Henriksson R (1994) Parotid-saliva composition during and after irradiation of head and neck-cancer. Oral Oncol 30b(4):230–233. https://doi.org/10.1016/0964-1955(94)90002-7
Makkonen TA, Tenovuo J, Vilja P, Heimdahl A (1986) Changes in the protein-composition of whole saliva during radiotherapy in patients with oral or pharyngeal cancer. Oral Surg Oral Med O 62(3):270–275. https://doi.org/10.1016/0030-4220(86)90007-1
Anderson MW, Izutsu KT, Rice JC (1981) Parotid-gland patho-physiology after mixed gamma and neutron-irradiation of cancer-patients. Oral Surg Oral Med O 52(5):495–500. https://doi.org/10.1016/0030-4220(81)90361-3
Vissink A, Jansma J, Spijkervet FKL, Burlage FR, Coppes RP (2003) Oral sequelae of head and neck radiotherapy. Crit Rev Oral Biol M 14(3):199–212. https://doi.org/10.1177/154411130301400305
Gallo C, Ciavarella D, Santarelli A, Ranieri E, Colella G, Lo Muzio L, Lo Russo L (2016) Potential salivary proteomic markers of oral squamous cell carcinoma. Cancer Genomics Proteomics 13(1):55–61
Yang J, Lee SJ, Kwon Y, Ma L, Kim J (2020) Tumor suppressive function of Matrin 3 in the basal-like breast cancer. Biol Res 53(1):42. https://doi.org/10.1186/s40659-020-00310-6
Hannig M, Dounis E, Henning T, Apitz N, Stosser L (2006) Does irradiation affect the protein composition of saliva? Clin Oral Investig 10(1):61–65. https://doi.org/10.1007/s00784-005-0026-z
Stenudd C, Nordlund A, Ryberg M, Johansson I, Kallestal C, Stromberg N (2001) The association of bacterial adhesion with dental caries. J Dent Res 80(11):2005–2010. https://doi.org/10.1177/00220345010800111101
Richards TM, Hurley T, Grove L, Harrington KJ, Carpenter GH, Proctor GB, Nutting CM (2017) The effect of parotid gland-sparing intensity-modulated radiotherapy on salivary composition, flow rate and xerostomia measures. Oral Dis 23(7):990–1000. https://doi.org/10.1111/odi.12686
Nishimura Y, Homma-Takeda S, Kim HS, Kakuta I (2014) Radioprotection of mice by lactoferrin against irradiation with sublethal X-rays. J Radiat Res 55(2):277–282. https://doi.org/10.1093/jrr/rrt117
Sakai M, Matsushita T, Hoshino R, Ono H, Ikai K, Sakai T (2017) Identification of the protective mechanisms of Lactoferrin in the irradiated salivary gland. Sci Rep 7(1):9753. https://doi.org/10.1038/s41598-017-10351-9
Bobek LA, Levine MJ (1992) Cystatins - inhibitors of cysteine proteinases. Crit Rev Oral Biol M 3(4):307–332. https://doi.org/10.1177/10454411920030040101
Petushkova AI, Savvateeva LV, Korolev DO, Zamyatnin AA (2019) Cysteine cathepsins: potential applications in diagnostics and therapy of malignant tumors. Biochemistry-Moscow+. 84(7):746–761. https://doi.org/10.1134/S000629791907006x
Xiao PP, Hu YH, Sun L (2010) Scophthalmus maximus cystatin B enhances head kidney macrophage-mediated bacterial killing. Dev Comp Immunol 34(12):1237–1241. https://doi.org/10.1016/j.dci.2010.07.008
Delecrode TR, Siqueira WL, Zaidan FC, Bellini MR, Moffa EB, Mussi MC, Xiao Y, Buzalaf MA (2015) Identification of acid-resistant proteins in acquired enamel pellicle. J Dent 43(12):1470–1475. https://doi.org/10.1016/j.jdent.2015.10.009
Missale C, Nash SR, Robinson SW, Jaber M, Caron MG (1998) Dopamine receptors: from structure to function. Physiol Rev 78(1):189–225
Sachlos E, Risueno RM, Laronde S, Shapovalova Z, Lee JH, Russell J, Malig M, McNicol JD, Fiebig-Comyn A, Graham M, Levadoux-Martin M, Lee JB, Giacomelli AO, Hassell JA, Fischer-Russell D, Trus MR, Foley R, Leber B, Xenocostas A, Brown ED, Collins TJ, Bhatia M (2012) Identification of drugs including a dopamine receptor antagonist that selectively target cancer stem cells. Cell. 149(6):1284–1297. https://doi.org/10.1016/j.cell.2012.03.049
Kim JW, Dang CV (2005) Multifaceted roles of glycolytic enzymes. Trends Biochem Sci 30(3):142–150. https://doi.org/10.1016/j.tibs.2005.01.005
Jung DW, Kim WH, Williams DR (2014) Chemical genetics and its application to moonlighting in glycolytic enzymes. Biochem Soc T 42:1756–1761. https://doi.org/10.1042/Bst20140201
Miles LA, Dahlberg CM, Plescia J, Felez J, Kato K, Plow EF (1991) Role of cell-surface lysines in plasminogen binding to cells - identification of alpha-enolase as a candidate plasminogen receptor. Biochemistry-Us 30(6):1682–1691. https://doi.org/10.1021/bi00220a034
Dano K, Behrendt N, Hoyer-Hansen G, Johnsen M, Lund LR, Ploug M, Romer J (2005) Plasminogen activation and cancer. Thromb Haemost 93(4):676–681. https://doi.org/10.1160/Th05-01-0054
Acknowledgements
The authors are grateful especialy the trial participants and their families, and the staff of the Clinical Research Center of the FOB/USP. The authors are gratefull to Mrs. Larissa Tercilia Grizzo for technical support with proteomic analysis.
Funding
The authors thank FAPESP for financial support and for the concession of a scholarship to the first (Proc. FAPESP 2017/05031-2) and second (Proc. FAPESP 2018/17860-6) authors. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brazil (CAPES) - Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The collection of the samples started after approval by the local Institutional Ethics Committee (No. 61484116.0.0000.5417), Bauru School of Dentistry, University of São Paulo, and signature of informed consent. The study was performed in accordance with the Declaration of Helsinki.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 260 kb)
Rights and permissions
About this article
Cite this article
Ventura, T.M.O., Ribeiro, N.R., Taira, E.A. et al. Radiotherapy changes the salivary proteome in head and neck cancer patients: evaluation before, during, and after treatment. Clin Oral Invest 26, 225–258 (2022). https://doi.org/10.1007/s00784-021-03995-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03995-5