Abstract
Objective
In this research, we assessed the usefulness of network meta-analysis (NMA), in creating a hierarchy to define the most effective oral care intervention for the prevention and management of ventilation-associated pneumonia (VAP).
Materials and methods
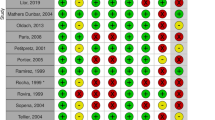
We applied NMA to a previously published robust pairwise meta-analysis. Statistical analyses were based on comparing rates of total VAP events between intervention groups and placebo-usual care groups. We synthesized a netgraph, reported the ranking order of the interventions, and summarized output by a forest plot with a reference treatment placebo/usual care.
Results
The results of this NMA are from the low and high risk of bias studies, and hence, we strongly recommend not to use findings of this NMA for clinical treatment needs, but based on results of the NMA, we highly recommend for future clinical trials. With our inclusion and exclusion criteria for the NMA, we extracted 25 studies (4473 subjects). The NMA included 16 treatments, 29 pairwise comparisons, and 15 designs. Based on results of NMA frequentist-ranking P scores, tooth brushing (P fixed-0.94, P random-0.89), tooth brushing with povidone-iodine (P fixed-0.90, P random-0.88), and furacillin (P fixed-0.88, P random-0.84) were the best three interventions for preventing VAP.
Conclusions
Any conclusion drawn from this NMA should be taken with caution and recommend future clinical trials with the results.
Clinical relevance
NMA appeared to be an effective platform from which multiple interventions reported in disparate clinical trials could be compared to derive a hierarchical assessment of efficacy in VAP intervention.



Similar content being viewed by others
Abbreviations
- VAP:
-
Ventilation-associated pneumonia
- OCI:
-
Oral care interventions
- NMA:
-
Network meta-analysis
- PMA:
-
Pairwise meta-analysis
- RCT:
-
Randomized controlled trials
- CHX:
-
Chlorhexidine
- Tb:
-
Tooth brushing
- TE:
-
Treatment effects
- SeTE:
-
Standard error of the treatment effects
- PI:
-
Povidone iodine
References
Magill SS, O’Leary E, Janelle SJ, Thompson DL, Dumyati G, Nadle J, Wilson LE, Kainer MA, Lynfield R, Greissman S, Ray SM, Beldavs Z, Gross C, Bamberg W, Sievers M, Concannon C, Buhr N, Warnke L, Maloney M, Ocampo V, Brooks J, Oyewumi T, Sharmin S, Richards K, Rainbow J, Samper M, Hancock EB, Leaptrot D, Scalise E, Badrun F, Phelps R, Edwards JR (2018) Changes in prevalence of health care-associated infections in U.S. hospitals. N Engl J Med 379(18):1732–1744
Ewan VC, Sails AD, Walls AW, Rushton S, Newton JL (2015) Dental and microbiological risk factors for hospital-acquired pneumonia in non-ventilated older patients. PLoS One 10(4):e0123622
Villar CC, Pannuti CM, Nery DM, Morillo CM, Carmona MJ, Romito GA (2016) Effectiveness of intraoral chlorhexidine protocols in the prevention of ventilator-associated pneumonia: meta-analysis and systematic review. Respir Care 61(9):1245–1259
Labeau SO, Van de Vyver K, Brusselaers N, Vogelaers D, Blot SI (2011) Prevention of ventilator-associated pneumonia with oral antiseptics: a systematic review and meta-analysis. Lancet Infect Dis 11(11):845–854
Hua F, Xie H, Worthington HV, Furness S, Zhang Q, Li C (2016) Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst Rev 10(10):CD008367
Mills EJ, Thorlund K, Ioannidis JP (2013) Demystifying trial networks and network meta-analysis. BMJ 346:f2914
Achana FA, Cooper NJ, Dias S, Lu G, Rice SJ, Kendrick D, Sutton AJ (2013) Extending methods for investigating the relationship between treatment effect and baseline risk from pairwise meta-analysis to network meta-analysis. Stat Med 32(5):752–771. https://doi.org/10.1002/sim.5539
Ioannidis JP (2009) Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta analyses. CMAJ 181(8):488–493
Cipriani A, Higgins JP, Geddes JR, Salanti G (2013) Conceptual and technical challenges in network meta-analysis. Ann Intern Med 159(2):130–137
Ades AE, Caldwell DM, Reken S, Welton NJ, Sutton AJ, Dias S (2013) Evidence synthesis for decision making: a reviewer’s checklist. Med Decis Mak 33(5):679–691
Rücker G, Schwarzer G (2017) Resolve conflicting rankings of outcomes in network meta-analysis: partial ordering of treatments. Res Synth Methods 8(4):526–536
Salanti G, Ades AE, Ioannidis JP (2011) Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 64(2):163–171
Urquhart O, Tampi MP, Pilcher L, Slayton RL, Araujo MWB, Fontana M, Guzmán-Armstrong S, Nascimento MM, Nový BB, Tinanoff N, Weyant RJ, Wolff MS, Young DA, Zero DT, Brignardello-Petersen R, Banfield L, Parikh A, Joshi G, Carrasco-Labra A (2019) Nonrestorative treatments for caries: systematic review and network meta-analysis. J Dent Res 98(1):14–26. https://doi.org/10.1177/0022034518800014
Moher DLA, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Mbuagbaw L, Rochwerg B, Jaeschke R, Heels-Andsell D, Alhazzani W, Thabane L, Guyatt GH (2017) Approaches to interpreting and choosing the best treatments in network meta-analyses. Syst Rev 6(1):79
Rücker G, Schwarzer G (2015) Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol 15:58
Klompas M, Speck K, Howell MD, Greene LR, Berenholtz SM (2014) Reappraisal of routine oral care with chlorhexidine gluconate for patients receiving mechanical ventilation: systematic review and meta-analysis. JAMA Intern Med 174(5):751–761
Norman G, Dumville JC, Moore ZE, Tanner J, Christie J, Goto S (2016) Antibiotics and antiseptics for pressure ulcers. Cochrane Database Syst Rev 4(4):CD011586
de Lacerda Vidal CF, Vidal AK, Monteiro JG Jr et al (2017) Impact of oral hygiene involving toothbrushing versus chlorhexidine in the prevention of ventilator-associated pneumonia: a randomized study. BMC Infect Dis 17(1):112. https://doi.org/10.1186/s12879-017-2188-0
González-Rubio Aguilar P, Ávalos Arenas V, Vega Gudiño NA, Moreno Herrera SD, Villa Guillén M, Moyao-García D, Fragoso Ríos R, Cuairán Ruidíaz V, Castro Díaz A, de la Rosa Zamboni D (2019) The impact of tooth brushing versus tooth brushing and chlorhexidine application to avoid postoperative pneumonia in children. Am J Infect Control 47(11):1340–1345. https://doi.org/10.1016/j.ajic.2019.05.018
Kaneoka A, Pisegna JM, Miloro KV, Lo M, Saito H, Riquelme LF, LaValley MP, Langmore SE (2015) Prevention of healthcare-associated pneumonia with oral care in individuals without mechanical ventilation: a systematic review and meta-analysis of randomized controlled trials. Infect Control Hosp Epidemiol 36(8):899–906. https://doi.org/10.1017/ice.2015.77
Satheeshkumar PS, Papatheodorou S, Sonis S (2020) Enhanced oral hygiene interventions as a risk mitigation strategy for the prevention of non-ventilator-associated pneumonia: a systematic review and meta-analysis. Br Dent J 228(8):615–622. https://doi.org/10.1038/s41415-020-1452-7
Salanti G, Nikolakopoulou A, Sutton AJ, Reichenbach S, Trelle S, Naci H, Egger M (2018) Planning a future randomized clinical trial based on a network of relevant past trials. Trials 19(1):365. https://doi.org/10.1186/s13063-018-2740-2
Goudie AC, Sutton AJ, Jones DR (2010) Donald A (2016) Empirical assessment suggests that existing evidence could be used more fully in designing randomized controlled trials. J Clin Epidemiol 63:983–991
Cooper NJ, Jones DR, Sutton AJ (2005) The use of systematic reviews when designing studies. Clin Trials Lond Engl 2:260–264
Clark T, Berger U, Mansmann U (2013) Sample size determinations in original research protocols for randomised clinical trials submitted to UK research ethics committees: review. BMJ 346:f1135
Jones AP, Conroy E, Williamson PR, Clarke M, Gamble C (2013) The use of systematic reviews in the planning, design and conduct of randomised trials: a retrospective cohort of NIHR HTA funded trials. BMC Med Res Methodol 13:50
Longworth L, Youn J, Bojke L, Palmer S, Griffin S, Spackman E, Claxton K (2013) When does NICE recommend the use of health technologies within a programme of evidence development? A systematic review of NICE guidance. PharmacoEconomics 31:137–149
Eichler H-G, Thomson A, Eichler I, Schneeweiss S (2015) Assessing the relative efficacy of new drugs: an emerging opportunity. Nat Rev Drug Discov 14:443–444
Naci H, O’Connor AB (2013) Assessing comparative effectiveness of new drugs before approval using prospective network meta-analyses. J Clin Epidemiol 66:812–816
Krahn U, Binder H, König J (2013) A graphical tool for locating inconsistency in network meta-analyses. BMC Med Res Methodol 13:35
Author information
Authors and Affiliations
Contributions
Satheeshkumar P Sankaran: Study design, statistical analysis, data interpretation, manuscript drafting, revision, and critical evaluation
Sonis S: Study design, data interpretation, manuscript revision and critical evaluation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
NA
Consent for publication
NA
Availability of data and materials
NA
Funding
No funding received for this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sankaran, S.P., Sonis, S. Network meta-analysis from a pairwise meta-analysis design: to assess the comparative effectiveness of oral care interventions in preventing ventilator-associated pneumonia in critically ill patients. Clin Oral Invest 25, 2439–2447 (2021). https://doi.org/10.1007/s00784-021-03802-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03802-1