Abstract
Objectives
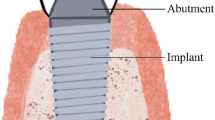
To evaluate the effect of various titanium abutment modifications on the behaviour of peri-implant soft tissue healing, inflammation and maintenance.
Material and methods
An electronic database research until 30 April 2019 was performed. A meta-analysis (MA) for each outcome parameter was performed by using the random-effects models with the DerSimonian-Laird estimator.
Results
Ten studies were included in the present review. Four studies with a long follow-up (5–6 years) reported the outcomes in a heterogeneous way and were suitable for MA. Six studies (4 RCT, 2 CCT) including 118 patients and 182 implants dealing with a modified healing abutment surface and short follow-up were selected for MA. The MA for PI and BoP as outcome showed no significant differences between surfaces (PI: P = 0.091; BoP: P = 0.099). The MA for PD as outcome showed no significant differences between surfaces (P = 0.488). No statistical significance was found by evaluating each mixed-effects model for potential moderators (type of study, study design, number of implants, follow-up length). The other four studies with a longer follow-up (5–6 years) reported contradictory results depending on the surface treatment investigated.
Conclusions
Within their limits, the present findings suggest that peri-implant soft tissue may not be affected by the surface treatment of titanium abutments on the short term. Contrasting results are reported in longer follow-up periods depending on the technique used to modify the abutment.
Clinical relevance
Clinicians should carefully evaluate the use of a modified titanium surface in their practice. Even if no differences in terms of inflammation are present at short term, these findings need to be validated in long-term studies.




Similar content being viewed by others
References
Özcan M, Hämmerle C (2012) Titanium as a reconstruction and implant material in dentistry: advantages and pitfalls. Materials (Basel) 5:1528–1545. https://doi.org/10.3390/ma5091528
Albrektsson T, Wennerberg A (2004) Oral implant surfaces: part 1—review focusing on topographic and chemical properties of different surfaces and in vivo responses to them. Int J Prosthodont 17:536–543
Menini M, Dellepiane E, Chvartszaid D, Baldi D, Schiavetti I, Pera P (2015) Influence of Different Surface Characteristics on Peri-implant Tissue Behavior: A Six-Year Prospective Report. Int J Prosthodont 28:389–395
Palmquist A, Lindberg F, Emanuelsson L, Branemark R, Engqvist H, Thomsen P (2009) Morphological studies on machined implants of commercially pure titanium and titanium alloy (Ti6Al4V) in the rabbit. J Biomed Mater Res B Appl Biomater 91B:309–319
Conserva E, Menini M, Ravera G, Pera P (2013) The role of surface implant treatments on the biological behavior of SaOS-2 osteoblast-like cells. An in vitro comparative study. Clin Oral Implants Res 24:880–889
Sanz-Martín I, Sanz-Sánchez I, Carrillo de Albornoz A, Figuero E, Sanz M (2018) Effects of modified abutment characteristics on peri-implant soft tissue health: A systematic review and meta-analysis. Clin Oral Implants Res 29:118–129
Salvi GE, Bosshardt DD, Lang NP, Abrahamsson I, Berglundh T, Lindhe J, Donos N (2015) Temporal sequence of hard and soft tissue healing around titanium dental implants. Perio 2000(68):135–152
Schierano G, Ramieri G, Cortese M, Aimetti M, Preti G (2002) Organization of the connective tissue barrier around long-term loaded implant abutments in man. Clin Oral Implants Res 13:460–464
Nevins M, Camelo M, Nevins ML, Schupbach P, Kim DM (2012) Reattachment of connective tissue fibers to a laser-microgrooved abutment surface. Int J Periodontics Restorative Dent 32:e131–e134
Shapoff CA, Babushkin JA, Wohl DJ (2016) Clinical use of laser-microtextured abutments: A case series. Int J Periodontics Restorative Dent 39:655–662
Mariotti A, Hefti AF (2015) Defining periodontal health. BMC Oral Health 15:S6
Wennerberg A, Sennerby L, Kultje C, Lekholm U (2003) Some soft tissue characteristics at implant abutment with different surface topography. A study in humans. J Clin Periodontol 30:88–94
Mangano C, Mangano FG, Shibli JA, Roth LA, D ’ Addazio G, Piattelli A, Iezzi G (2018) Immunohistochemical evaluation of Peri-implant soft tissues around machined and direct metal laser sintered (DMLS) healing abutments in humans. Int J Environ Res Public Health 30:15(8)
Quirynen M, van der Mei HC, Bollen CM, Schotte A, Marechal M, Doornbusch GI, Naert I, Busscher HJ, van Steenberghe D (1993) An in vivo study of the influence of the surface roughness of implants on the microbiology of supra- and subgingival plaque. J Dent Res 72:1304–1309
Pesce P, Canullo L, Grusovin MG, de Bruyn H, Cosyn J, Pera P (2015) Systematic review of some prosthetic risk factors for periimplantitis. J Prosthet Dent 114:346–350
Pesce P, Menini M, Tealdo T, Bevilacqua M, Pera F, Pera P (2014) Peri-implantitis: a systematic review of recently published papers. Int J Prosthodont 27:15–25
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Akobeng AK (2005) Understanding randomised controlled trials. Arch Dis Child 90:840–844. https://doi.org/10.1136/adc.2004.058222
Higgins JP, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011. The Cochrane Collaboration, Chichester
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Sterne JAC, Egger M (2001) Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 54:1046–1055
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. J Stat Softw 36:1–48. https://doi.org/10.18637/jss.v036.i03
Hall J, Neilands J, Davies JR, Ekestubbe A, Friberg B (2019) A randomized, controlled, clinical study on a new titanium oxide abutment surface for improved healing and soft tissue health. Clin Implant Dent Relat Res 21:55–68. https://doi.org/10.1111/cid.12749
Garcia B, Camacho F, Pearrocha D, Tallarico M, Perez S, Canullo L (2017) Influence of plasma cleaning procedure on the interaction between soft tissue and abutments: a randomized controlled histologic study. Clin Oral Implants Res 28:1269–1277. https://doi.org/10.1111/clr.12953
Schwarz F, Becker J, Civale S, Hazar D, Iglhaut T, Iglhaut G (2018) Onset, progression and resolution of experimental peri-implant mucositis at different abutment surfaces: A randomized controlled two-Centre study. J Clin Periodontol 45:471–483
Menini M, Dellepiane E, Baldi D, Longobardi MG, Pera P, Izzotti A (2017) Microarray expression in peri-implant tissue next to different titanium implant surfaces predicts clinical outcomes: a split- mouth study. Clin Oral Implants Res 28:e121–e134
Degidi M, Artese L, Piattelli A, Scarano A, Shibli JA, Piccirilli M, Perrotti V, Iezzi G (2012) Histological and immunohistochemical evaluation of the peri-implant soft tissues around machined and acid-etched titanium healing abutments: a prospective randomised study. Clin Oral Investig 16(3):857–866
Baldi D, Menini M, Pera F, Ravera G, Pera P (2009) Plaque accumulation on exposed titanium surfaces and peri-implant tissue behavior. A preliminary 1-year clinical study. Int J Prosthodont 22:447–455
Raes M, D'hondt R, Teughels W, Coucke W, Quirynen M (2018) A 5-year randomized clinical trial comparing minimally with moderately rough implants in patients with severe periodontitis. J Clin Periodontol 45:711–720
Göthberg C, Gröndahl K, Omar O, Thomsen P, Slotte C (2018) Bone and soft tissue outcomes, risk factors, and complications of implant-supported prostheses: 5-years RCT with different abutment types and loading protocols. Clin Implant Dent Relat Res 20:313–321
Canullo L, Tallarico M, Peñarrocha-Oltra D, Monje A, Wang HL, Peñarrocha-Diago M (2016) Implant abutment cleaning by plasma of argon: 5-year follow-up of a randomized controlled trial. J Periodontol 87:434–442
Canullo L, Tallarico M, Penarrocha M, Corrente G, Fiorellini J, Penarrocha D (2017) Plasma of argon cleaning treatment on implant abutments in Periodontally healthy patients: six years Postloading results of a randomized controlled trial. Int J Periodontics Restorative Dent 37:683–690
Teughels W, Van Assche N, Sliepen I, Quirynen M (2006) Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implants Res 17:68–81
Ioannidis JPA, Trikalinos TA (2007) The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ 176:1091–1096
Funding
This study was self-supported.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. All procedures performed in the included studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 278 kb).
Rights and permissions
About this article
Cite this article
Canullo, L., Menini, M., Santori, G. et al. Titanium abutment surface modifications and peri-implant tissue behavior: a systematic review and meta-analysis. Clin Oral Invest 24, 1113–1124 (2020). https://doi.org/10.1007/s00784-020-03210-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03210-x