Abstract
Objectives
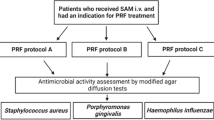
Platelet-rich fibrin (PRF) procuring protocols have been suggested, differing in speed and time duration. Since different derivation protocols may alter PRF characteristics, the present study was conducted to evaluate the variations in the fibrin network pattern, platelet count, and antimicrobial efficacy of PRF procured using variable centrifugation speeds and time durations in different age groups.
Materials and methods
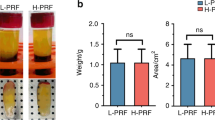
Sixty healthy subjects participated in the study and were equally divided into three age groups (20–34 years, 35–49 years, 50–65 years). From each age group, total of 6 PRF membranes were fabricated from 10 ml tubes. Three PRF membranes were obtained at 1400, 2800, and 3500 rpm for 8 min while other 3 membranes were obtained after 15 min of centrifugation respectively. The relative centrifugal force (RCF) values were within the spectrum of 228–1425 g. PRF membranes were then subjected to platelet count estimation, antimicrobial activity against oral bacteria, and changes in fibrin network pattern with respect to different age groups and different centrifugation protocols.
Results
Highest platelet concentration, antimicrobial activity, and dense fibrin network were obtained in 20–34 years age group. Intragroup analysis within each group revealed highest platelet count and antimicrobial activity in PRF membranes, obtained at 1400 rpm for 8 min. Denser fibrin network pattern was demonstrated by PRF membranes procured at 3500 rpm for 15 min.
Conclusions
PRF properties, i.e., platelet count, antimicrobial efficacy, and fibrin network, are influenced by technical aspects of PRF preparation (RCF value, centrifugation speed, and time) and patient age.
Clinical relevance
Based on the finding of present study, it can be implied that lower centrifugation speed and time can increase the platelet concentration and antimicrobial activity of the PRF membrane. Contrarily, lowering the speed and time leads to lesser density fibrin network pattern. Centrifugation protocols thus need to be adapted accordingly.






Similar content being viewed by others
References
Amable PR, Carias RB, Teixeira MV, da Cruz Pacheco Í, Corrêa do Amaral RJ, Granjeiro J, Borojevic R (2013) Platelet-rich plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Res Ther 4:67. https://doi.org/10.1186/scrt218
Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V, Fujioka-Kobayashi M, Bishara M, Zhang Y, Wang HL, Chandad F, Nacopoulos C, Simonpieri A, Aalam AA, Felice P, Sammartino G, Ghanaati S, Hernandez MA, Choukroun J (2017) Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Investig 21:1913–1927. https://doi.org/10.1007/s00784-017-2133-z
Cieslik-Bielecka A, Choukroun J, Odin G, Dohan Ehrenfest DM (2012) L-PRP/L-PRF in esthetic plastic surgery, regenerative medicine of the skin and chronic wounds. Curr Pharm Biotechnol 13:1266–1277. https://doi.org/10.2174/138920112800624463
Clark RA (2001) Fibrin and wound healing. Ann N Y Acad Sci 936:355–367. https://doi.org/10.1111/j.1749-6632.2001.tb03522.x
Gibble JW, Ness PM (1990) Fibrin glue: the perfect operative sealant? Transfusion 30:741–747. https://doi.org/10.1046/j.1537-2995.1990.30891020337.x
Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T (2014) Classification of platelet concentrates (platelet-rich plasma-PRP, platelet-rich fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J 4:3–9. https://doi.org/10.7892/boris.62982
Agrawal AA (2017) Evolution, current status and advances in application of platelet concentrate in periodontics and implantology. World J Clin Cases 5:159–171. https://doi.org/10.12998/wjcc.v5.i5.159
Marx RE (2004) Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg 62:489–496. https://doi.org/10.1016/j.joms.2003.12.003
Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR (1998) Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85:638–646. https://doi.org/10.1016/S1079-2104(98)90029-4
Cai YZ, Zhang C, Lin XJ (2015) Efficacy of platelet-rich plasma in arthroscopic repair of full-thickness rotator cuff tears: a meta-analysis. J Shoulder Elb Surg 24:1852–1859. https://doi.org/10.1016/j.jse.2015.07.035
Meheux CJ, McCulloch PC, Lintner DM, Varner KE, Harris JD (2016) Efficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: a systematic review. Arthroscopy 32:495–505. https://doi.org/10.1016/j.arthro.2015.08.005
Singh B, Goldberg LJ (2016) Autologous platelet-rich plasma for the treatment of pattern hair loss. Am J Clin Dermatol 17:359–367. https://doi.org/10.1007/s40257-016-0196-2
Anfossi G, Trovati M, Mularoni E, Massucco P, Calcamuggi G, Emanuelli G (1989) Influence of propranolol on platelet aggregation and thromboxane B2 production from platelet-rich plasma and whole blood. Prostaglandins Leukot Essent Fat Acids 36:1–7. https://doi.org/10.1016/0952-3278(89)90154-3
Fijnheer R, Pietersz RN, de Korte D, Gouwerok CW, Dekker WJ, Reesink HW, Roos D (1990) Platelet activation during preparation of platelet concentrates: a comparison of the platelet-rich plasma and the buffy coat methods. Transfusion 30:634–638. https://doi.org/10.1046/j.1537-2995.1990.30790385523.x
Choukroun J, Adda F, Schoeffler C, Vervelle A (2001) Opportunities in implant dentistry: PRF (in French). Implantodontie 42:e62
Pradeep AR, Rao NS, Agarwal E, Bajaj P, Kumari M, Naik SB (2012) Comparative evaluation of autologous platelet-rich fibrin and platelet- rich plasma in the treatment of 3-wall intrabony defects in chronic periodontitis: a randomized controlled clinical trial. J Periodontol 83:1499–1507. https://doi.org/10.1902/jop.2012.110705
Clark D, Rajendran Y, Paydar S, Ho S, Cox D, Ryder M, Dollard J, Kao RT (2018) Advanced platelet-rich fibrin and freeze-dried bone allograft for ridge preservation: a randomized controlled clinical trial. J Periodontol 89:379–387. https://doi.org/10.1002/JPER.17-0466
Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D (2009) Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: a 6-month study. J Periodontol 80:244–252. https://doi.org/10.1902/jop.2009.080253
Kökdere NN, Baykul T, Findik Y (2015) The use of platelet-rich fibrin (PRF) and PRF-mixed particulated autogenous bone graft in the treatment of bone defects: an experimental and histomorphometrical study. Dent Res J (Isfahan) 12:418–424. https://doi.org/10.4103/1735-3327.166188
Mazor Z, Horowitz RA, Corso MD et al (2009) Sinus floor augmentation with simultaneous implant placement using Choukroun’s platelet-rich fibrin as the sole grafting material: a radiologic and histologic study at 6 months. J Periodontol 80:2056–2064. https://doi.org/10.1902/jop.2009.090252
Fujioka-Kobayashi M, Miron RJ, Hernandez M, Kandalam U, Zhang Y, Choukroun J (2017) Optimized platelet-rich fibrin with the low-speed concept: growth factor release, biocompatibility, and cellular response. J Periodontol 88:112–121. https://doi.org/10.1902/jop.2016.160443
Kobayashi E, Flückiger L, Fujioka-Kobayashi M, Sawada K, Sculean A, Schaller B, Miron RJ (2016) Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin Oral Investig 20:2353–2360. https://doi.org/10.1007/s00784-016-1719-1
Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJJ, Mouhyi J, Dohan DM (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e56–e60. https://doi.org/10.1016/j.tripleo.2005.07.011
Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJJ, Mouhyi J, Dohan DM (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part V: histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:299–303. https://doi.org/10.1016/j.tripleo.2005.07.012
Dohan Ehrenfest DM, Del Corso M, Diss A, Mouhyi J, Charrier JB (2010) Three-dimensional architecture and cell composition of a Choukroun’s platelet-rich fibrin clot and membrane. J Periodontol 81:546–555. https://doi.org/10.1902/jop.2009.090531
Fabbro MD, Bortolin M, Taschieri S, Ceci C, Weinstein RL (2016) Antimicrobial properties of platelet-rich preparations. A systematic review of the current pre-clinical evidence. Platelets 27:276–285. https://doi.org/10.3109/09537104.2015.1116686
Eren G, Gürkan A, Atmaca H, Dönmez A, Atilla G (2016) Effect of centrifugation time on growth factor and MMP release of an experimental platelet-rich fibrin-type product. Platelets 27:427–432. https://doi.org/10.3109/09537104.2015.1131253
Miron RJ, Pinto NR, Quirynen M, Ghanaati S (2019) Standardization of relative centrifugal forces in studies related to platelet-rich fibrin. J Periodontol. https://doi.org/10.1002/JPER.18-0553
Webb DI, Parker L, Webb K (2004) Platelet count assessment from peripheral blood smear (PBS). Alaska Med 46:92–95
Malok M, Titchener EH, Bridgers C, Lee BY, Bamberg R (2007) Comparison of two platelet count estimation methodologies for peripheral blood smears. Clin Lab Sci 20:154–160
Tanner AC, Goodson JM (1986) Sampling of microorganisms associated with periodontal disease. Oral Microbiol Immunol 1:15–20. https://doi.org/10.1111/j.1399-302X.1986.tb00310.x
Karde PA, Sethi KS, Mahale SA, Khedkar SU, Patil AG, Joshi CP (2017) Comparative evaluation of platelet count and antimicrobial efficacy of injectable platelet-rich fibrin with other platelet concentrates: an in vitro study. J Indian Soc Periodontol 21:97–101. https://doi.org/10.4103/jisp.jisp_201_17
Athanassiadis B, Abbott PV, George N, Walsh LJ (2009) An in vitro study of the antimicrobial activity of some endodontic medicaments and their bases using an agar well diffusion assay. Aust Dent J 54:141–146. https://doi.org/10.1111/j.1834-7819.2009.01107.x
Dantas AA, Fontanari LA, Ishi Ede P et al (2012) Blood cells attachment after root conditioning and PRP application: an in vitro study. J Contemp Dent Pract 13:332–338
Yajamanya SR, Chatterjee A, Babu CN, Karunanithi D (2016) Fibrin network pattern changes of platelet-rich fibrin in young versus old age group of individuals: a cell block cytology study. J Indian Soc Periodontol 20:151–156. https://doi.org/10.4103/0972-124X.176390
Miron RJ, Fujioka-Kobayashi M, Bishara M, Zhang Y, Hernandez M, Choukroun J (2016) Platelet-rich fibrin and soft tissue wound healing: a systematic review. Tissue Eng B Rev 23:83–99. https://doi.org/10.1089/ten.TEB.2016.0233
Bajpai R, Rajak C, Poonia M (2015) Platelet estimation by peripheral smear: reliable, rapid, cost-effective method to assess degree of thrombocytopenia. Int J Med Sci Res Pract 2:90–93
Suchetha A, Lakshmi P, Bhat D, Mundinamane DB, Soorya KV, Bharwani GA (2015) Platelet concentration in platelet concentrates and periodontal regeneration-unscrambling the ambiguity. Contemp Clin Dent 6:510–516. https://doi.org/10.4103/0976-237X.169850
Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, Landes C, Sader R, Kirkpatrick CJ, Choukroun J (2014) Advanced platelet-rich fibrin: a new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implantol 40:679–689. https://doi.org/10.1563/aaid-joi-D-14-00138
Keith Wilson JW (2010) Principles and techniques of biochemistry and molecular biology. Cambridge University Press, Cambridge
Choukroun J, Ghanaati S (2018) Reduction of relative centrifugation force within injectable platelet-rich-fibrin (PRF) concentrates advances patients’ own inflammatory cells, platelets and growth factors: the first introduction to the low speed centrifugation concept. Eur J Trauma Emerg Surg 44:87–95. https://doi.org/10.1007/s00068-017-0767-9
Jenne CN, Urrutia R, Kubes P (2013) Platelets: bridging hemostasis, inflammation, and immunity. Int J Lab Hematol 35:254–261. https://doi.org/10.1111/ijlh.12084
Kour P, Pudakalkatti PS, Vas AM, Das S, Padmanabhan S (2018) Comparative evaluation of antimicrobial efficacy of platelet-rich plasma, platelet-rich fibrin, and injectable platelet-rich fibrin on the standard strains of Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans. Contemp Clin Dent 9:S325–S330. https://doi.org/10.4103/ccd.ccd_367_18
Badade PS, Mahale SA, Panjwani AA, Vaidya PD, Warang AD (2016) Antimicrobial effect of platelet-rich plasma and platelet-rich fibrin. Indian J Dent Res 27:300–304. https://doi.org/10.4103/0970-9290.186231
Moojen DJ, Everts PA, Schure RM et al (2008) Antimicrobial activity of platelet-leukocyte gel against Staphylococcus aureus. J Orthop Res 26:404–410. https://doi.org/10.1002/jor.20519
Castro AB, Herrero ER, Slomka V, Pinto N, Teughels W, Quirynen M (2019) Antimicrobial capacity of leucocyte-and platelet rich fibrin against periodontal pathogens. Sci Rep 9:8188. https://doi.org/10.1038/s41598-019-44755-6
D’asta F, Halstead F, Harrison P, Zecchi Orlandini S, Moiemen N, Lord J (2018) The contribution of leucocytes to the antimicrobial activity of platelet-rich plasma preparations: a systematic review. Platelets 29:9–20. https://doi.org/10.1080/09537104.2017.1317731
Yeaman MR (1997) The role of platelets in antimicrobial host defense. Clin Infect Dis 25:951–968. https://doi.org/10.1086/516120
Hoaglin DR, Lines GK (2013) Prevention of localized osteitis in mandibular third-molar sites using platelet-rich fibrin. Int J Dent 2013:875380–875384. https://doi.org/10.1155/2013/875380
Dohan Ehrenfest DM, Pinto NR, Pereda A, Jiménez P, Corso MD, Kang BS, Nally M, Lanata N, Wang HL, Quirynen M (2018) The impact of the centrifuge characteristics and centrifugation protocols on the cells, growth factors, and fibrin architecture of a leukocyte- and platelet-rich fibrin (L-PRF) clot and membrane. Platelets 29:171–184. https://doi.org/10.1080/09537104.2017.1293812
Miron RJ, Dham A, Dham U, Zhang Y, Pikos MA, Sculean A (2018) The effect of age, gender, and time between blood draw and start of centrifugation on the size outcomes of platelet-rich fibrin (PRF) membranes. Clin Oral Investig 23:2179–2185. https://doi.org/10.1007/s00784-018-2673-x
Miron RJ, Chai J, Zheng S, Feng M, Sculean A, Zhang Y (2019) A novel method for evaluating and quantifying cell types in platelet rich fibrin and an introduction to horizontal centrifugation. J Biomed Mater Res A. https://doi.org/10.1002/jbm.a.36734
Acknowledgments
The authors are thankful to Dr. Smita Khedkar (MD, Professor and Head, Department of Microbiology, Karmaveer Bhausaheb Hiray Dental College and Hospital, Nashik, Maharashtra, India) for her valuable guidance in microbial analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mamajiwala, A.S., Sethi, K.S., Raut, C.P. et al. Impact of different platelet-rich fibrin (PRF) procurement methods on the platelet count, antimicrobial efficacy, and fibrin network pattern in different age groups: an in vitro study. Clin Oral Invest 24, 1663–1675 (2020). https://doi.org/10.1007/s00784-019-03022-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03022-8