Abstract
Background
Peri-implant diseases have been recognized as being among the ever-increasing complications related to dental implants. The aim of this study was to evaluate the adjunctive use of enamel matrix derivative (EMD) to mechanical debridement (MD) in patients with these conditions in terms of clinical parameters and cytokine levels of peri-implant crevicular fluid (PICF).
Methods
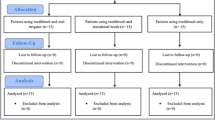
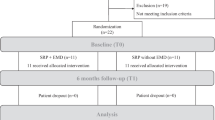
In the present double-blind clinical trial, 46 patients with peri-implant mucositis (PM) were randomly divided into control and test groups. Two different therapeutic protocols, consisting of non-surgical MD alone (control group) and MD with the application of EMD (test group), were considered for the two groups. Clinical parameters [bleeding on probing (BOP) and probing depth (PD)] and sampling from PICF were carried out before treatment and 3 months postoperatively. The levels of IL-6 and IL-17 cytokines in PICF were evaluated by enzyme-linked immunosorbent (ELISA).
Results
Three-month post-interventional assay revealed significant improvements in BOP and PD in the test group in comparison to the control group (P < 0.0001). Relative to control, IL-6 and IL-17 levels were reduced significantly (p < 0.05) in the test group compared to the control group.
Conclusion
Application of EMD can be considered an adjunct to MD in the non-surgical treatment of PM. However, complete recovery was not observed using either treatment approach showing that management of implant-associated disease is still a significant clinical problem.

Similar content being viewed by others
Notes
Top Dent Lifco Dental AB, Enko¨ping, Sweden
Piezon ® 250, EMS Electro Medical Systems SA, Nyon, Switzerland
Air-Flow Master ®, Perio Powder ®; EMS Electro Medical Systems SA, Nyon, Switzerland
Laboratorios KIN, S.A., ,Barcelona, Spain
Emdogain ® Straumann, Basel, Switzerland
Laboratorios KIN, S.A., ,Barcelona, Spain
12 UNC color coded probe, Hu-Friedy Mfg. Co., LLC.Chicago, IL
Insight Dental Films, Eastman Kodak Company, Rochester, NY, USA
Periopaper ® Oraflow, Plainview, NY, USA
Eppendorf ® AG, Hamburg, Germany
PBS, Invitrogen, USA
Sigma-Aldrich, Saint Louis, MO, USA
MABTECH AB, R&D Systems, Büro Deutschland, Germany
References
Aljateeli M, Fu JH, Wang HL (2012) Managing peri-implant bone loss: current understanding. Clin Implant Dent Relat Res 14(Suppl 1):e109–e118
Algraffee H, Borumandi F, Cascarini L (2012) Peri-implantitis. Br J Oral Maxillofac Surg 50(8):689–694
Lindhe J, Meyle J (2008) Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol 35(8 Suppl):282–285
Atieh MA et al (2013) The frequency of peri-implant diseases: a systematic review and meta-analysis. J Periodontol 84(11):1586–1598
Zitzmann NU, Berglundh T (2008) Definition and prevalence of peri-implant diseases. J Clin Periodontol 35(8 Suppl):286–291
Hultin M et al (2002) Microbiological findings and host response in patients with peri-implantitis. Clin Oral Implants Res 13(4):349–358
Van Dyke TE (2012) The impact of genotypes and immune reactivity on peri-implant inflammation: identification and therapeutic use of anti-inflammatory drugs and immunomodulators. Eur J Oral Implantol 5(Suppl):S51–S60
Irshad M et al (2013) Cytokine and matrix metalloproteinase expression in fibroblasts from peri-implantitis lesions in response to viable Porphyromonas gingivalis. J Periodontal Res 48(5):647–656
Javed F et al (2011) Proinflammatory cytokines in the crevicular fluid of patients with peri-implantitis. Cytokine 53(1):8–12
Severino VO, Napimoga MH, de Lima Pereira SA (2011) Expression of IL-6, IL-10, IL-17 and IL-8 in the peri-implant crevicular fluid of patients with peri-implantitis. Arch Oral Biol 56(8):823–828
Heitz-Mayfield LJ (2008) Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol 35(8 Suppl):292–304
Renvert S, Persson GR (2009) Periodontitis as a potential risk factor for peri-implantitis. J Clin Periodontol 36(Suppl 10):9–14
Strietzel FP et al (2007) Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. J Clin Periodontol 34(6):523–544
Kozlovsky A et al (2007) Impact of implant overloading on the peri-implant bone in inflamed and non-inflamed peri-implant mucosa. Clin Oral Implants Res 18(5):601–610
Nogueira-Filho G, Iacopino AM, Tenenbaum HC (2011) Prognosis in implant dentistry: a system for classifying the degree of peri-implant mucosal inflammation. J Can Dent Assoc 77:3
Lang NP et al (2004) Consensus statements and recommended clinical procedures regarding implant survival and complications. Int J Oral Maxillofac Implants 19(Suppl):150–154
Zeza B, Pilloni A (2012) Peri-implant mucositis treatments in humans: a systematic review. Ann Stomatol (Roma) 3(3–4):83–89
Renvert S, Roos-Jansaker AM, Claffey N (2008) Non-surgical treatment of peri-implant mucositis and peri-implantitis: a literature review. J Clin Periodontol 35(8 Suppl):305–315
Renvert S et al (2009) Mechanical non-surgical treatment of peri-implantitis: a double-blind randomized longitudinal clinical study. I: clinical results. J Clin Periodontol 36(7):604–609
Renvert S et al (2008) Mechanical and repeated antimicrobial therapy using a local drug delivery system in the treatment of peri-implantitis: a randomized clinical trial. J Periodontol 79(5):836–844
Schar D et al (2013) Anti-infective therapy of peri-implantitis with adjunctive local drug delivery or photodynamic therapy: six-month outcomes of a prospective randomized clinical trial. Clin Oral Implants Res 24(1):104–110
Thierbach R, Eger T (2013) Clinical outcome of a nonsurgical and surgical treatment protocol in different types of peri-implantitis: a case series. Quintessence Int 44(2):137–148
Esposito M, Grusovin MG, Worthington HV (2012) Treatment of peri-implantitis: what interventions are effective? A Cochrane systematic review. Eur J Oral Implantol 5(Suppl):S21–S41
Esposito M et al (2008) The efficacy of interventions to treat peri-implantitis: a Cochrane systematic review of randomised controlled clinical trials. Eur J Oral Implantol 1(2):111–125
Deppe H et al (2013) Nonsurgical antimicrobial photodynamic therapy in moderate vs severe peri-implant defects: a clinical pilot study. Quintessence Int 44(8):609–618
van Winkelhoff AJ (2012) Antibiotics in the treatment of peri-implantitis. Eur J Oral Implantol 5(Suppl):S43–S50
Schwarz F et al (2005) Clinical evaluation of an Er:YAG laser for nonsurgical treatment of peri-implantitis: a pilot study. Clin Oral Implants Res 16(1):44–52
Kotsakis, G. A., et al. (2014) A systematic review and meta-analysis of the effect of various laser wavelengths in the treatment of peri-implantitis. J Periodontol
Salvi GE et al (2007) Adjunctive local antibiotic therapy in the treatment of peri-implantitis II: clinical and radiographic outcomes. Clin Oral Implants Res 18(3):281–285
Renvert S, Roos-Jansåker AM, Claffey N (2008) Non-surgical treatment of peri-implant mucositis and peri-implantitis: a literature review. J Clin Periodontol 35(s8):305–315
Petković A et al (2010) Proinflammatory cytokines (IL-1β and TNF-α) and chemokines (IL-8 and MIP-1α) as markers of peri-implant tissue condition. Int J Oral Maxillofac Surg 39(5):478–485
Heitz-Mayfield LJ (2008) Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol 35(s8):292–304
Esposito M et al (2009) Enamel matrix derivative (Emdogain) for periodontal tissue regeneration in intrabony defects. A Cochrane systematic review. Eur J Oral Implantol 2(4):247–266
Koop R, Merheb J, Quirynen M (2012) Periodontal regeneration with enamel matrix derivative in reconstructive periodontal therapy: a systematic review. J Periodontol 83(6):707–720
Li W, Xiao L, Hu J (2012) The use of enamel matrix derivative alone versus in combination with bone grafts to treat patients with periodontal intrabony defects: a meta-analysis. J Am Dent Assoc 143(9):e46–e56
Hammarström L, Heijl L, Gestrelius S (1997) Periodontal regeneration in a buccal dehiscence model in monkeys after application of enamel matrix proteins. J Clin Periodontol 24(9 Pt 2):669–677
Koop R, Merheb J, Quirynen M (2012) Periodontal regeneration with enamel matrix derivative in reconstructive periodontal therapy: a systematic review. J Periodontol 83(6):707–720
Sculean A et al (2003) Histologic evaluation of human intrabony defects following non-surgical periodontal therapy with and without application of an enamel matrix protein derivative. J Periodontol 74(2):153–160
Chano L et al (2003) Emdogain® regulation of cellular differentiation in wounded rat periodontium. J Periodontal Res 38(2):164–174
Spahr A et al (2002) Effect of the enamel matrix derivative Emdogain on the growth of periodontal pathogens in vitro. J Clin Periodontol 29(1):62–72
Walter C et al (2006) Moderate effect of enamel matrix derivative (Emdogain gel) on Porphyromonas gingivalis growth in vitro. Arch Oral Biol 51(3):171–176
Wada Y, Mizuno M, Tamura M (2009) Enamel matrix derivative neutralized the effect of lipopolysaccharide on osteoprotegerin and receptor activator of nuclear factor kappa B ligand expression of osteoblasts. Arch Oral Biol 54(4):306–312
Bosshardt DD (2008) Biological mediators and periodontal regeneration: a review of enamel matrix proteins at the cellular and molecular levels. J Clin Periodontol 35(s8):87–105
Jiang J et al (2001) Effects of enamel matrix derivative on gene expression of primary osteoblasts. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 91(1):95–100
Qu Z et al (2010) Effect of Emdogain on proliferation and migration of different periodontal tissue-associated cells. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109(6):924–931
Weishaupt P et al (2008) Stimulation of osteoblasts with Emdogain increases the expression of specific mineralization markers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106(2):304–308
Kemoun P et al (2011) The role of cell surface markers and enamel matrix derivatives on human periodontal ligament mesenchymal progenitor responses in vitro. Biomaterials 32(30):7375–7388
Lyngstadaas SP et al (2009) Enamel matrix proteins; old molecules for new applications. Orthod Craniofac Res 12(3):243–253
Wennstrom JL, Lindhe J (2002) Some effects of enamel matrix proteins on wound healing in the dento-gingival region. J Clin Periodontol 29(1):9–14
Khedmat S et al (2010) Effects of enamel matrix derivative on the viability, cytokine secretion, and phagocytic activity of human monocytes. J Endod 36(6):1000–1003
Sculean A et al (2004) Treatment of peri-implantitis with EDTA decontamination and application of an enamel matrix protein derivate—a report of 3 cases. PERIO (Periodontal Practice Today) 1:237–245
Froum SJ, Froum SH, Rosen PS (2012) Successful management of peri-implantitis with a regenerative approach: a consecutive series of 51 treated implants with 3-to 7.5-year follow-up. International Journal of Periodontics and Restorative Dentistry 32(1):11
Sanz M, Chapple IL (2012) Clinical research on peri-implant diseases: consensus report of Working Group 4. J Clin Periodontol 39(Suppl 12):202–206
Etter TH et al (2002) Healing after standardized clinical probing of the perlimplant soft tissue seal. Clin Oral Implants Res 13(6):571–580
Sahm N et al (2011) Non-surgical treatment of peri-implantitis using an air-abrasive device or mechanical debridement and local application of chlorhexidine: a prospective, randomized, controlled clinical study. J Clin Periodontol 38(9):872–878
Mellado-Valero A et al (2013) Decontamination of dental implant surface in peri-implantitis treatment: a literature review. Med Oral Patol Oral Cir Bucal 18(6):e869–e876
1996) Meffert, R., Periodontitis vs. peri-implantitis: the same disease? The same treatment? Critical Reviews in Oral Biology & Medicine 7(3):278–291
Froum SJ et al (2001) A comparative study utilizing open flap debridement with and without enamel matrix derivative in the treatment of periodontal intrabony defects: a 12-month re-entry study. J Periodontol 72(1):25–34
Gutierrez MA, Mellonig JT, Cochran DL (2003) Evaluation of enamel matrix derivative as an adjunct to non-surgical periodontal therapy. J Clin Periodontol 30(8):739–745
Mombelli A et al (2005) Enamel matrix proteins and systemic antibiotics as adjuncts to non-surgical periodontal treatment: clinical effects. J Clin Periodontol 32(3):225–230
Brito C et al (2014) Is keratinized mucosa indispensable to maintain peri-implant health? A systematic review of the literature. J Biomed Mater Res B Appl Biomater 102(3):643–650
Casado PL et al (2013) Peri-implant disease and chronic periodontitis: is interleukin-6 gene promoter polymorphism the common risk factor in a Brazilian population? Int J Oral Maxillofac Implants 28(1):35–43
Kadkhodazadeh M et al (2013) IL-17 gene polymorphism is associated with chronic periodontitis and peri-implantitis in Iranian patients: a cross-sectional study. Immunol Investig 42(2):156–163
Koh A et al (2007) Role of osteopontin in neutrophil function. Immunology 122(4):466–475
Froum SJ, Rosen PS (2012) A proposed classification for peri-implantitis. International Journal of Periodontics and Restorative Dentistry 32(5):533
Lindhe J, Meyle J (2008) Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol 35(s8):282–285
Rosen P et al (2013) Peri-implant mucositis and peri-implantitis: a current understanding of their diagnoses and clinical implications. J Periodontol 84(4):436–443
Lang NP, Berglundh T (2011) Periimplant diseases: where are we now?—Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol 38(s11):178–181
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Funding
The work was supported by the Dental and Periodontal Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
Ethical approval
The study was approved by the Research Ethics Committee of Tabriz University of Medical Sciences (No. 9278) and registered with the local World Health Organization Registry Network (IRCT2013060113543N1).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
(DOC 217 kb)
Rights and permissions
About this article
Cite this article
Kashefimehr, A., Pourabbas, R., Faramarzi, M. et al. Effects of enamel matrix derivative on non-surgical management of peri-implant mucositis: a double-blind randomized clinical trial. Clin Oral Invest 21, 2379–2388 (2017). https://doi.org/10.1007/s00784-016-2033-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-2033-7