Abstract
Objectives
This systematic review analyzed the relationship between periapical and periodontal pathologies in the posterior maxilla and the appearance of the Schneiderian membrane in cone-beam computed tomography (CBCT) compared with sound dentitions.
Methods
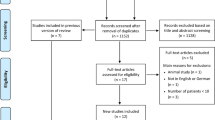
Five electronic databases (Cochrane Library, Embase, OpenGrey, PubMed, Web of Science), complemented by hand searching, were screened up to May 9, 2016. Human clinical studies that used CBCT and contained information on the periapical/periodontal status in the posterior maxilla and Schneiderian membrane appearance were included. A weighted vote counting (WVC) method was applied to summarize results across studies.
Results
Out of 413 records, 20 studies were included. In the WVC, the studies that observed a positive association between periapical lesions and the appearance of the Schneiderian membrane outweighed those that found no such association (WVC 51 % and WVC 33 %, respectively), with some studies yielding indeterminate results (WVC 16 %). Regarding the relation between periodontal pathologies and the appearance of the Schneiderian membrane, WVC produced a tie between studies demonstrating a positive association (WVC 46 %) and those showing no association (WVC 44 %); one study (WVC 10 %) reported indeterminate results.
Conclusions
On CBCT scans, periapical lesions in the posterior maxilla are likely to be associated with Schneiderian membrane thickening. In contrast, current evidence regarding the relation between periodontal diseases and the appearance of the Schneiderian membrane in CBCT is inconclusive.
Clinical relevance
Incidental maxillary sinus findings on CBCT scans warrant thorough differential diagnosis. Frequently, they may be related to dental pathologies.



Similar content being viewed by others
References
Ariji Y, Obayashi N, Goto M, et al. (2006) Roots of the maxillary first and second molars in horizontal relation to alveolar cortical plates and maxillary sinus: computed tomography assessment for infection spread. Clin Oral Investig 10(1):35–41
Kang SH, Kim BS, Kim Y (2015) Proximity of posterior teeth to the maxillary sinus and buccal bone thickness: a biometric assessment using cone-beam computed tomography. J Endod 41(11):1839–1846
von Arx T, Fodich I, Bornstein MM (2014) Proximity of premolar roots to maxillary sinus: a radiographic survey using cone-beam computed tomography. J Endod 40(10):1541–1548
Tian X-M, Qian L, Xin X-Z, et al. (2015) An analysis of the proximity of maxillary posterior teeth to the maxillary sinus using cone-beam computed tomography. J Endod 42(3):371–377
Lemagner F, Maret D, Peters OA, et al. (2015) Prevalence of apical bone defects and evaluation of associated factors detected with cone-beam computed tomographic images. J Endod 41(7):1043–1047
Walter C, Weiger R, Zitzmann NU (2011) Periodontal surgery in furcation-involved maxillary molars revisited—an introduction of guidelines for comprehensive treatment. Clin Oral Invest 15(1):9–20
Obayashi N, Ariji Y, Goto M, et al. (2004) Spread of odontogenic infection originating in the maxillary teeth: computerized tomographic assessment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 98(2):223–231
Selden HS (1999) Endo-antral syndrome and various endodontic complications. J Endod 25(5):389–393
Brook I (2006) Sinusitis of odontogenic origin. Otolaryngol Head Neck Surg 135(3):349–355
Hoskison E, Daniel M, Rowson JE, et al. (2012) Evidence of an increase in the incidence of odontogenic sinusitis over the last decade in the UK. J Laryngol Otol 126(1):43–46
Brook I (1992) Aerobic and anaerobic bacteriology of intracranial abscesses. Pediatr Neurol 8(3):210–214
Brook I, Friedman EM (1982) Intracranial complications of sinusitis in children. A sequela of periapical abscess. Ann Otol Rhinol Laryngol 91(1 Pt 1):41–43
Bomeli SR, Branstetter BF, Ferguson BJ (2009) Frequency of a dental source for acute maxillary sinusitis. Laryngoscope 119(3):580–584
Vallo J, Suominen-Taipale L, Huumonen S, et al. (2010) Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Health Examination Survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109(3):e80–e87
Lofthag-Hansen S, Huumonen S, Grondahl K, et al. (2007) Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103(1):114–119
Kanagasingam S, Mannocci F, Lim CX, et al. (2016) Diagnostic accuracy of periapical radiography and cone beam computed tomography in detecting apical periodontitis using histopathological findings as a reference standard. Int Endod J. doi:10.1111/iej.12650
Shahbazian M, Vandewoude C, Wyatt J, et al. (2014) Comparative assessment of panoramic radiography and CBCT imaging for radiodiagnostics in the posterior maxilla. Clin Oral Invest 18(1):293–300
Fokkens WJ, Lund VJ, Mullol J, et al. (2012) European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl 20(23):1–298
Al Abduwani J, Zilin Skiene L, Colley S, et al. (2016) Cone beam CT paranasal sinuses versus standard multidetector and low dose multidetector CT studies. Am J Otolaryngol 37(1):59–64
Patel S, Durack C, Abella F, et al. (2014) European Society of Endodontology position statement: the use of CBCT in endodontics. Int Endod J 47(6):502–504
Walter C, Schmidt JC, Dula K, et al. (2016) Cone beam computed tomography (CBCT) for diagnosis and treatment planning in periodontology: a systematic review. Quintessence Int 47(1):25–37
Dula K, Benic GI, Bornstein MM, et al. (2015) SADMFR guidelines for the use of cone-beam computed tomography/digital volume tomography. Swiss Dent J 125(9):945–953
Carter L, Farman AG, Geist J, et al. (2008) American Academy of Oral and Maxillofacial Radiology executive opinion statement on performing and interpreting diagnostic cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106(4):561–562
Jones NS (2002) CT of the paranasal sinuses: a review of the correlation with clinical, surgical and histopathological findings. Clin Otolaryngol Allied Sci 27(1):11–17
Ritter L, Lutz J, Neugebauer J, et al. (2011) Prevalence of pathologic findings in the maxillary sinus in cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111(5):634–640
Bornstein MM, Wasmer J, Sendi P, et al. (2012) Characteristics and dimensions of the Schneiderian membrane and apical bone in maxillary molars referred for apical surgery: a comparative radiographic analysis using limited cone beam computed tomography. J Endod 38(1):51–57
Nunes CA, Guedes OA, Alencar AH, et al. (2015) Evaluation of periapical lesions and their association with maxillary sinus abnormalities on cone-beam computed tomographic images. J Endod 42(1):42–46
Janner SF, Caversaccio MD, Dubach P, et al. (2011) Characteristics and dimensions of the Schneiderian membrane: a radiographic analysis using cone beam computed tomography in patients referred for dental implant surgery in the posterior maxilla. Clin Oral Implants Res 22(12):1446–1453
Phothikhun S, Suphanantachat S, Chuenchompoonut V, et al. (2012) Cone-beam computed tomographic evidence of the association between periodontal bone loss and mucosal thickening of the maxillary sinus. J Periodontol 83(5):557–564
Ren S, Zhao H, Liu J, et al. (2015) Significance of maxillary sinus mucosal thickening in patients with periodontal disease. Int Dent J 65(6):303–310
Shanbhag S, Karnik P, Shirke P, et al. (2013) Association between periapical lesions and maxillary sinus mucosal thickening: a retrospective cone-beam computed tomographic study. J Endod 39(7):853–857
Maia LC, Antonio AG (2012) Systematic reviews in dental research. A guideline. J Clin Pediatr Dent 37(2):117–124
Moher D, Liberati A, Tetzlaff J, et al. (2009a) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012
Moher D, Liberati A, Tetzlaff J, et al. (2009b) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med 6(6):e1000097
Schmidt JC, Sahrmann P, Weiger R, et al. (2013) Biologic width dimensions—a systematic review. J Clin Periodontol 40(5):493–504
Graziani F, Figuero E, Herrera D (2012) Systematic review of quality of reporting, outcome measurements and methods to study efficacy of preventive and therapeutic approaches to peri-implant diseases. J Clin Periodontol 39(Suppl 12):224–244
Higgins JP, Green S (eds) (2011) Cochrane handbook for systematic reviews of interventions. Cochrane Collaboration, Version 5.1.0 (updated March 2011)
Acharya A, Hao J, Mattheos N, et al. (2014) Residual ridge dimensions at edentulous maxillary first molar sites and periodontal bone loss among two ethnic cohorts seeking tooth replacement. Clin Oral Implants Res 25(12):1386–1394
Block MS, Dastoury K (2014) Prevalence of sinus membrane thickening and association with unhealthy teeth: a retrospective review of 831 consecutive patients with 1,662 cone-beam scans. J Oral Maxillofac Surg 72(12):2454–2460
Brüllmann DD, Schmidtmann I, Hornstein S, et al. (2012) Correlation of cone beam computed tomography (CBCT) findings in the maxillary sinus with dental diagnoses: a retrospective cross-sectional study. Clin Oral Invest 16(4):1023–1029
Dagassan-Berndt DC, Zitzmann NU, Lambrecht JT, et al. (2013) Is the Schneiderian membrane thickness affected by periodontal disease? A cone beam computed tomography-based extended case series. J Int Acad Periodontol 15(3):75–82
Eggers G (2011) Cone beam computer tomography for paranasal sinus imaging. Int J Comput Assisted Radiol Surg 6:205–206
Goller-Bulut D, Sekerci A-E, Kose E, et al. (2015) Cone beam computed tomographic analysis of maxillary premolars and molars to detect the relationship between periapical and marginal bone loss and mucosal thickness of maxillary sinus. Med Oral Patol Oral Cir Bucal 20(5):9
Kasikcioglu A, Gulsahi A (2015) Relationship between maxillary sinus pathologies and maxillary posterior tooth periapical pathologies. Oral Radiol:1–7
Lu Y, Liu Z, Zhang L, et al. (2012) Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. J Endod 38(8):1069–1074
Nurbakhsh B, Friedman S, Kulkarni GV, et al. (2011) Resolution of maxillary sinus mucositis after endodontic treatment of maxillary teeth with apical periodontitis: a cone-beam computed tomography pilot study. J Endod 37(11):1504–1511
Rege IC, Sousa TO, Leles CR, et al. (2012) Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health 12:30
Schneider AC, Brägger U, Sendi P, et al. (2013) Characteristics and dimensions of the sinus membrane in patients referred for single-implant treatment in the posterior maxilla: a cone beam computed tomographic analysis. Int J Oral Maxillofac Implants 28(2):587–596
Sheikhi M, Pozve NJ, Khorrami L (2014) Using cone beam computed tomography to detect the relationship between the periodontal bone loss and mucosal thickening of the maxillary sinus. Dent Res J (Isfahan) 11(4):495–501
Yildirim E, Ciftci ME, Kamak G et al (2016) Evaluation of the relationship between maxillary sinus floor position and maxillary sinusitis using cone beam computed tomography. Oral Radiol 1–7
Yoo J-Y, Pi S-H, Kim Y-S, et al. (2011) Healing pattern of the mucous membrane after tooth extraction in the maxillary sinus. J Periodontal Implant Sci 41(1):23–29
Schmidt JC, Walter C, Amato M, et al. (2014) Treatment of periodontal-endodontic lesions—a systematic review. J Clin Periodontol 41(8):779–790
Miracle AC, Mukherji SK (2009) Conebeam CT of the head and neck, part 1: physical principles. AJNR Am J Neuroradiol 30(6):1088–1095
Leiva-Salinas C, Flors L, Gras P, et al. (2014) Dental flat panel conebeam CT in the evaluation of patients with inflammatory sinonasal disease: diagnostic efficacy and radiation dose savings. AJNR Am J Neuroradiol 35(11):2052–2057
Tos M, Mogensen C (1979) Mucus production in the nasal sinuses. Acta Otolaryngol Suppl 360:131–134
Pommer B, Unger E, Suto D, et al. (2009) Mechanical properties of the Schneiderian membrane in vitro. Clin Oral Implants Res 20(6):633–637
Aimetti M, Massei G, Morra M, et al. (2008) Correlation between gingival phenotype and Schneiderian membrane thickness. Int J Oral Maxillofac Implants 23(6):1128–1132
Ørstavik D, Kerekes K, Eriksen HM (1986) The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol 2(1):20–34
Estrela C, Bueno MR, Azevedo BC, et al. (2008) A new periapical index based on cone beam computed tomography. J Endod 34(11):1325–1331
Walter C, Rodriguez FR, Taner B, et al. (2012a) Association of tobacco use and periapical pathosis—a systematic review. Int Endod J 45(12):1065–1073
Pope O, Sathorn C, Parashos P (2014) A comparative investigation of cone-beam computed tomography and periapical radiography in the diagnosis of a healthy periapex. J Endod 40(3):360–365
Roque-Torres GD, Ramirez-Sotelo LR, Vaz SL, et al. (2016) Association between maxillary sinus pathologies and healthy teeth. Braz J Otorhinolaryngol 82(1):33–38
Houser SM, Keen KJ (2008) The role of allergy and smoking in chronic rhinosinusitis and polyposis. Laryngoscope 118(9):1521–1527
Tarp B, Fiirgaard B, Christensen T, et al. (2000) The prevalence and significance of incidental paranasal sinus abnormalities on MRI. Rhinology 38(1):33–38
Anavi Y, Allon DM, Avishai G, et al. (2008) Complications of maxillary sinus augmentations in a selective series of patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106(1):34–38
Garlini G, Redemagni M, Donini M, et al. (2010) Maxillary sinus elevation with an alloplastic material and implants: 11 years of clinical and radiologic follow-up. J Oral Maxillofac Surg 68(5):1152–1157
Manor Y, Mardinger O, Bietlitum I, et al. (2010) Late signs and symptoms of maxillary sinusitis after sinus augmentation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110(1):e1–e4
Bolger WE, Butzin CA, Parsons DS (1991) Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 101(1 Pt 1):56–64
Manning SC, Biavati MJ, Phillips DL (1996) Correlation of clinical sinusitis signs and symptoms to imaging findings in pediatric patients. Int J Pediatr Otorhinolaryngol 37(1):65–74
Matsuno O, Ono E, Takenaka R, et al. (2008) Asthma and sinusitis: association and implication. Int Arch Allergy Immunol 147(1):52–58
International Commission on Radiological Protection (1977) Recommendations of the International Commission on Radiological Protection (ICRP #26). The International Commission on Radiological Protection, Oxford ICRP Publication 26
Walter C, Weiger R, Dietrich T, et al. (2012b) Does three-dimensional imaging offer a financial benefit for treating maxillary molars with furcation involvement? A pilot clinical case series. Clin Oral Implants Res 23(3):351–358
Hodez C, Griffaton-Taillandier C, Bensimon I (2011) Cone-beam imaging: applications in ENT. Eur Ann Otorhinolaryngol Head Neck Dis 128(2):65–78
Carmeli G, Artzi Z, Kozlovsky A, et al. (2011) Antral computerized tomography pre-operative evaluation: relationship between mucosal thickening and maxillary sinus function. Clin Oral Implants Res 22(1):78–82
Longhini AB, Branstetter BF, Ferguson BJ (2010) Unrecognized odontogenic maxillary sinusitis: a cause of endoscopic sinus surgery failure. Am J Rhinol Allergy 24(4):296–300
Troeltzsch M, Pache C, Troeltzsch M, et al. (2015) Etiology and clinical characteristics of symptomatic unilateral maxillary sinusitis: a review of 174 cases. J Craniomaxillofac Surg 43(8):1522–1529
Bornstein MM, von Arx T, Altermatt HJ (2008) Loss of pulp sensitivity and pain as the first symptoms of a Ewing’s sarcoma in the right maxillary sinus and alveolar process: report of a case. J Endod 34(12):1549–1553
Bell GW, Joshi BB, Macleod RI (2011) Maxillary sinus disease: diagnosis and treatment. Br Dent J 210(3):113–118
Marending M, Peters OA, Zehnder M (2005) Factors affecting the outcome of orthograde root canal therapy in a general dentistry hospital practice. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99(1):119–124
Longo DL, Drazen JM (2016) Data sharing. N Engl J Med 374(3):276–277
Acknowledgments
Original investigators, irrespective of their inclusion in this systematic review, whose research productivity in this field established the basis of this review are gratefully acknowledged [80].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The work was funded by the Department of Periodontology, Endodontology and Cariology, University Centre for Dental Medicine, University of Basel, Hebelstrasse 3, CH-4056, Basel, Switzerland.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Florin Eggmann and Thomas Connert contributed equally to this work.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Eggmann, F., Connert, T., Bühler, J. et al. Do periapical and periodontal pathologies affect Schneiderian membrane appearance? Systematic review of studies using cone-beam computed tomography. Clin Oral Invest 21, 1611–1630 (2017). https://doi.org/10.1007/s00784-016-1944-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1944-7