Abstract
Objectives
The β1 integrin (CD29) is a putative marker for cancerous epithelial stem cells. Cancer stem cells are essential to drive tumor growth, recurrence, and metastasis. We investigated the role of β1-integrin expression in the development of malignant phenotypes of oral squamous cell carcinoma (OSCC).
Materials and methods
Immunostaining was used to analyze the expression levels of β1 integrins in different types of cell colonies and tumor spheres. The results of cell viability and migration assays with and without siRNA knockdown of β1-integrin expression were compared. Cells expressing β1 integrins were evaluated for their tumorigenicity in mice. The expression of β1 integrins in human specimens of oral cancers at different clinical stages was semiquantified based on immunohistochemical staining of the β1-integrin protein.
Results
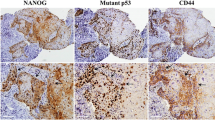
The expression level of β1 integrins in Meng-1 oral epidermoid carcinoma cells (OECM-1) cells was significantly higher in holoclonal colonies and tumor spheres compared to control cells. The knockdown of β1-integrin expression in OECM-1 cells reduced cell proliferation, migration, and tumor sphere formation. Beta-1 integrin (+) cells were more tumorigenic in the mouse xenograft model than β1 integrin (−) cells. In the human specimens, the expression level of the β1-integrin protein positively correlated with the clinical stage.
Conclusion
The expression of β1 integrin in OECM-1 cells is involved in the development of malignant phenotypes of OSCC.
Clinical relevance
Inhibitors for β1-integrin signaling may be suitable to become target-specific therapies for OSCC.






Similar content being viewed by others
References
Reichart PA (2001) Identification of risk groups for oral precancer and cancer and preventive measures. Clin Oral Invest 5:207–213
Oliveira DT, de Moraes RV, Fiamengui Filho JF, Fanton Neto J, Landman G, Kowalski LP (2006) Oral verrucous carcinoma: a retrospective study in São Paulo region, Brazil. Clin Oral Invest 10:205–209
Al-Rawi NH, Talabani NG (2008) Squamous cell carcinoma of the oral cavity: a case series analysis of clinical presentation and histological grading of 1,425 cases from Iraq. Clin Oral Investig 12:15–18
Ravindran G, Devaraj H (2012) Aberrant expression of β-catenin and its association with ∆Np63, Notch-1, and clinicopathological factors in oral squamous cell carcinoma. Clin Oral Investig 16:1275–1288
Myoung H, Kim MJ, Lee JH, OK YJ, Paeng JY, Yun PY (2006) Correlation of proliferative markers (Ki-67 and PCNA) with survival and lymph node metastasis in oral squamous cell carcinoma: a clinical and histopathological analysis of 113 patients. Int J Oral Maxillofac Surg 35:1005–1010
Hinerman RW, Mendenhall WM, Morris CG, Amdur RJ, Werning JW, Villaret DB (2004) Postoperative irradiation for squamous cell carcinoma of the oral cavity: 35-year experience. Head Neck 26:984–994
Felthaus O, Ettl T, Gosau M, Driemel O, Brockhoff G, Reck A, Zeitler K, Hautmann M, Reichert TE, Schmalz G, Morsczeck C (2011) Cancer stem cell-like cells from a single cell of oral squamous carcinoma cell lines. Biochem Biophys Res Commun 407:28–33
Costea DE, Tsinkalovsky O, Vintermyr OK, Johannessen AC, Mackenzie IC (2006) Cancer stem cells—new and potentially important targets for the therapy of oral squamous cell carcinoma. Oral Diseases 12:443–454
Zhang Z, Filho MS, Nör JE (2012) The biology of head and neck cancer stem cells. Oral Oncol 48:1–9
Krishnamurthy S, Nör JE (2012) Head and neck cancer stem cells. J Dent Res 91:334–340
Jones PH, Harper S, Watt FM (1995) Stem cell patterning and fate in human epidermis. Cell 80:83–93
Locke M, Heywood M, Fawell S, Mackenzie IC (2005) Retention of intrinsic stem cell hierarchies in carcinoma-derived cell lines. Cancer Res 65:8944–8950
Huang AH, Chen YK, Chan AW, Shieh TY, Lin LM (2009) Isolation and characterization of normal hamster buccal pouch stem/stromal cells—a potential oral cancer stem/stem-like cell model. Oral Oncol 45:e189–e195
Kim SA, Kwon SM, Kim JA, Kang KW, Yoon JH, Ahn SG (2011) 5′-Nitro-indirubinoxime, an indirubin derivative, suppresses metastatic ability of human head and neck cancer cells through the inhibition of integrin β1/FAK/Akt signaling. Cancer Lett 306:197–204
Barkan D, Chambers AF (2011) β1-integrin: a potential therapeutic target in the battle against cancer recurrence. Clin Cancer Res 17:7219–7223
Barrandon Y, Green H (1987) Three clonal types of keratinocytes with different capacities for multiplication. Proc Natl Acad Sci U S A 84:2302–2306
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A (eds) (2010) AJCC cancer staging manual, 7th edn. Springer, New York
Miyazaki T, Futaki S, Hasegawa K, Kawasaki M, Sanzen N, Hayashi M, Kawase E, Sekiguchi K, Nakatsuji N, Suemori H (2008) Recombinant human laminin isoforms can support the undifferentiated growth of human embryonic stem cells. Biochem Biophys Res Commun 375:27–32
Lee ST, Yun JI, Jo YS, Mochizuki M, van der Vlies AJ, Kontos S, Ihm JE, Lim JM, Hubbell JA (2010) Engineering integrin signaling for promoting embryonic stem cell self-renewal in a precisely defined niche. Biomaterials 31:1219–1226
Igarashi T, Shimmura S, Yoshida S, Tonogi M, Shinozaki N, Yamane GY (2008) Isolation of oral epithelial progenitors using collagen IV. Oral Dis 14:413–418
Hongo K, Tanaka J, Tsuno NH, Kawai K, Nishikawa T, Shuno Y, Sasaki K, Kaneko M, Hiyoshi M, Sunami E, Kitayama J, Takahashi K, Nagawa H (2012) CD133(−) cells, derived from a single human colon cancer cell line, are more resistant to 5-fluorouracil (FU) than CD133(+) cells, dependent on the β1-integrin signaling. J Surg Res 175:278–288
Zhang X, Liu Y, Gilcrease MZ, Yuan XH, Clayman GL, Adler-Storthz K, Chen Z (2002) A lymph node metastatic mouse model reveals alternations of metastasis-related gene expression in metastatic human oral carcinoma sublines selected from a poorly metastatic parental cell line. Cancer 95:1663–1672
Geng S, Guo Y, Wang Q, Li L, Wang J (2013) Cancer stem-like cells enriched with CD29 and CD44 markers exhibit molecular characteristics with epithelial-mesenchymal transition in squamous cell carcinoma. Arch Dermatol Res 305:35–47
Koukourakis MI, Giatromanolaki A, Tsakmaki V, Danielidis V, Sivridis E (2012) Cancer stem cell phenotype relates to radio-chemotherapy outcome in locally advanced squamous cell head–neck cancer. Br J Cancer 106:846–853
Thomas GJ, Jones J, Speight PM (1997) Integrins and oral cancer. Oral Oncol 33:381–388
Maragou P, Bazopoulou-Kyrkanidou E, Panotopoulou E, Kakarantza-Angelopoulou E, Sklavounou-Andrikopoulou A, Kotaridis S (1999) Alteration of integrin expression in oral squamous cell carcinomas. Oral Dis 5:20–26
Tennenbaum T, Yuspa SH, Grover A, Castronovo V, Sobel ME, Yamada Y, De Luca LM (1992) Extracellular matrix receptors and mouse skin carcinogenesis: altered expression linked to appearance of early markers of tumor progression. Cancer Res 52:2966–2976
Tumbarello DA, Temple J, Brenton JD (2012) β3 integrin modulates transforming growth factor beta induced (TGFBI) function and paclitaxel response in ovarian cancer cells. Mol Cancer 11:36
Parise LV, Lee JW, Juliano RL (2000) New aspects of integrin signaling in cancer. Semin Cancer Biol 10:407–414
Juliano RL (1993) The role of beta 1 integrins in tumors. Semin Cancer Biol 4:277–283
Hynes RO (2002) Integrins: bidirectional, allosteric signaling machines. Cell 110:673–687
Aguirre Ghiso JA, Kovalski K, Ossowski L (1999) Tumor dormancy induced by downregulation of urokinase receptor in human carcinoma involves integrin and MAPK signaling. J Cell Biol 147:89–104
Hodkinson PS, Elliott T, Wong WS, Rintoul RC, Mackinnon AC, Haslett C, Sethi T (2006) ECM overrides DNA damage-induced cell cycle arrest and apoptosis in small-cell lung cancer cells through beta1 integrin-dependent activation of PI3-kinase. Cell Death Differ 13:1776–1788
Park CC, Zhang HJ, Yao ES, Park CJ, Bissell MJ (2008) Beta 1 integrin inhibition dramatically enhances radiotherapy efficacy in human breast cancer xenografts. Cancer Res 68:4398–4405
Sayed SI, Dwivedi RC, Katna R, Garg A, Pathak KA, Nutting CM, Rhys-Evans P, Harrington KJ, Kazi R (2011) Implications of understanding cancer stem cell (CSC) biology in head and neck squamous cell cancer. Oral Oncol 47:237–243
Senger DR, Perruzzi CA, Streit M, Koteliansky VE, de Fougerolles AR, Detmar M (2002) The alpha(1)beta(1) and alpha(2)beta(1) integrins provide critical support for vascular endothelial growth factor signaling, endothelial cell migration, and tumor angiogenesis. Am J Pathol 160:195–204
Brown MC, Staniszewska I, Del Valle L, Tuszynski GP, Marcinkiewicz C (2008) Angiostatic activity of obtustatin as alpha1beta1 integrin inhibitor in experimental melanoma growth. Int J Cancer 123:2195–2203
Acknowledgments
This study was supported by grants from the National Science Council, Taiwan (NSC 99-2314-B-006-035-MY3) and National Cheng Kung University Hospital, Taiwan (NCKUH-10004002).
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, HC., Wu, CL., Chen, YL. et al. High-level β1-integrin expression in a subpopulation of highly tumorigenic oral cancer cells. Clin Oral Invest 18, 1277–1284 (2014). https://doi.org/10.1007/s00784-013-1088-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-013-1088-y