Abstract
Background
Surgical site infection (SSI) is an important complication after spine surgery. The management of SSI is characterized by significant variability, and there is little guidance regarding an evidence-based approach. The objective of this study was to identify risk factors associated with treatment failure of SSI after spine surgery.
Patients and methods
A total of 225 consecutive patients with SSI after spine surgery between July 2005 and July 2010 were studied retrospectively. Patients were treated with aggressive surgical debridement and prolonged antibiotic therapy. Outcome and risk factors were analyzed in 197 patients having 1 year of follow-up. Treatment success was defined as resolution within 90 days.
Results
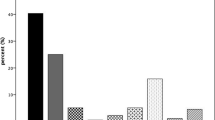
A total of 126 (76 %) cases were treated with retention of implants. Forty-three (22 %) cases had treatment failure with five (2.5 %) cases resulting in death. Lower rates of treatment success were observed with late infection (38 %), fusion with fixation to the ilium (67 %), Propionibacterium acnes (43 %), poly microbial infection (68 %), >6 operated spinal levels (67 %), and instrumented cases (73 %). Higher rates of early resolution were observed with superficial infection (93 %), methicillin-sensitive Staphylococcus aureus (95 %), and <3 operated spinal levels (88 %). Multivariate logistic regression revealed late infection was the most significant independent risk factor associated with treatment failure. Superficial infection and methicillin-sensitive Staphylococcus aureus were predictors of early resolution.
Conclusion
Postoperative spine infections were treated with aggressive surgical debridement and antibiotic therapy. High rates of treatment failure occurred in cases with late infection, long instrumented fusions, polymicrobial infections, and Propionibacterium acnes. Removal of implants and direct or staged re-implantation may be a useful strategy in cases with high risk of treatment failure.
Similar content being viewed by others
References
Mok JM, Guillaume TJ, Talu U, Berven SH, Deviren V, Kroeber M, Bradford DS, Hu SS. Clinical outcome of deep wound infection after instrumented posterior spinal fusion: a matched cohort analysis. Spine. 2009;34:578–83.
Goode AP, Cook C, Gill JB, Tackett S, Brown C, Richardson W. The risk of risk-adjustment measures for perioperative spine infection after spinal surgery. Spine. 2011;36:752–8.
Smith JS, Shaffrey CI, Sansur CA, Berven SH, Fu KM, Broadstone PA, Choma TJ, Goytan MJ, Noordeen HH, Knapp DR Jr, Hart RA, Donaldson WF 3rd, Polly DW Jr, Perra JH, Boachie-Adjei O, Scoliosis Research Society Morbidity and Mortality Committee. Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine. 2011;36:556–63.
Pull ter Gunne AF, Mohamed AS, Skolasky RL, van Laarhoven CJ, Cohen DB. The presentation, incidence, etiology, and treatment of surgical site infections after spinal surgery. Spine. 2010;35:1323–8.
Weinstein MA, McCabe JP, Cammisa FP Jr. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord. 2000;13:422–6.
Collins I, Wilson-MacDonald J, Chami G, Burgoyne W, Vineyakam P, Berendt T, Fairbank J. The diagnosis and management of infection following instrumented spinal fusion. Eu Spine J. 2008;17:445–50.
Sponseller PD, Shah SA, Abel MF, Newton PO, Letko L, Marks M. Infection rate after spine surgery in cerebral palsy is high and impairs results: multicenter analysis of risk factors and treatment. Clin Orthop Relat Res. 2010;468:711–6.
Koutsoumbelis S, Hughes AP, Girardi FP, Cammisa FP Jr, Finerty EA, Nguyen JT, Gausden E, Sama AA. Risk factors for postoperative infection following posterior lumbar instrumented arthrodesis. J Bone Joint Surg Am. 2011;93:1627–33.
Fang A, Hu SS, Endres N, Bradford DS. Risk factors for infection after spinal surgery. Spine. 2005;30:1460–5.
Olsen MA, Nepple JJ, Riew KD, Lenke LG, Bridwell KH, Mayfield J, Fraser VJ. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am. 2008;90:62–9.
Pull ter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine. 2009;34:1422–8.
Glassman SD, Dimar JR, Puno RM, Johnson JR. Salvage of instrumental lumbar fusions complicated by surgical wound infection. Spine. 1996;21:2163–9.
Levi AD, Dickman CA, Sonntag VK. Management of postoperative infections after spinal instrumentation. J Neurosurg. 1997;86:975–80.
Rihn JA, Lee JY, Ward WT. Infection after the surgical treatment of adolescent idiopathic scoliosis: evaluation of the diagnosis, treatment, and impact on clinical outcomes. Spine. 2008;33:289–94.
Ho C, Skaggs DL, Weiss JM, Tolo VT. Management of infection after instrumented posterior spine fusion in pediatric scoliosis. Spine. 2007;32:2739–44.
Mehbod AA, Ogilvie JW, Pinto MR, Schwender JD, Transfeldt EE, Wood KB, Le Huec JC, Dressel T. Postoperative deep wound infections in adults after spinal fusion: management with vacuum-assisted wound closure. J Spinal Disord Tech. 2005;18:14–7.
Canavese F, Gupta S, Krajbich JI, Emara KM. Vacuum-assisted closure for deep infection after spinal instrumentation for scoliosis. J Bone Joint Surg Br. 2008;90:377–81.
Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, Dudeck MA, Pollock DA, Horan TC. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37:783–805.
Kowalski TJ, Berbari EF, Huddleston PM, Steckelberg JM, Mandrekar JN, Osmon DR. The management and outcome of spinal implant infections: contemporary retrospective cohort study. Clin Infect Dis. 2007;44:913–20.
Kim JI, Suh KT, Kim SJ, Lee JS. Implant removal for the management of infection after instrumented spinal fusion. J Spinal Disord Tech. 2010;23:258–65.
Muschik M, Luck W, Schlenzka D. Implant removal for late-developing infection after instrumented posterior spinal fusion for scoliosis: reinstrumentation reduces loss of correction. A retrospective analysis of 45 cases. Eu Spine J. 2004;13:645–51.
Richards BS. Delayed infections following posterior spinal instrumentation for the treatment of idiopathic scoliosis. J Bone Joint Surg Am. 1995;77:524–9.
Haidar R, Najjar M, Der Boghossian A, Tabbarah Z. Propionibacterium acnes causing delayed postoperative spine infection: review. Scand J Infect Dis. 2010;42:405–11.
Hahn F, Zbinden R, Min K. Late implant infections caused by Propionibacterium acnes in scoliosis surgery. Eu Spine J. 2005;14:783–8.
Sampedro MF, Huddleston PM, Piper KE, Karau MJ, Dekutoski MB, Yaszemski MJ, Currier BL, Mandrekar JN, Osmon DR, McDowell A, Patrick S, Steckelberg JM, Patel R. A biofilm approach to detect bacteria on removed spinal implants. Spine. 2010;35:1218–24.
Gristina AG, Costerton JW. Bacterial adherence to biomaterials and tissue. The significance of its role in clinical sepsis. J Bone Joint Surg Am. 1985;67:264–73.
Hedequist D, Haugen A, Hresko T, Emans J. Failure of attempted implant retention in spinal deformity delayed surgical site infections. Spine. 2009;34:60–4.
Schoenfeld AJ, Ochoa LM, Bader JO, Belmont PJ Jr. Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am. 2011;93:1577–82.
Sansur CA, Smith JS, Coe JD, Glassman SD, Berven SH, Polly DW Jr, Perra JH, Boachie-Adjei O, Shaffrey CI. Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine. 2011;36:E593–7.
Acknowledgments
We are grateful to Dr. Steven Takemoto, Dr. Amir Abdul-jabbar, Dr. Serena S. Hu, Dr. Shane Burch, Praveen V. Mummaneni, MD, and Dr. Dean Chou for preparation of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was approved by the UCSF Committee on Human Research.
About this article
Cite this article
Maruo, K., Berven, S.H. Outcome and treatment of postoperative spine surgical site infections: predictors of treatment success and failure. J Orthop Sci 19, 398–404 (2014). https://doi.org/10.1007/s00776-014-0545-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-014-0545-z