Abstract
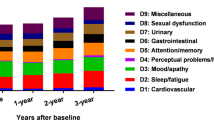
Data on frequency, severity and correlations of NMS with motor complications are only available for a limited number of NMS. The NMS Scale (NMSS) is a validated tool to assess a broad range of NMS, which has not been used in NMS fluctuations. We assessed fluctuations of a broad range of non-motor symptom (NMS) for a 1-month time period in fluctuating Parkinson’s disease (PD) in a multicenter cross-sectional study using the NMSS assessing NMS in motor On (NMSSOn) and Off state (NMSSOff) combined with clinical NMS and motor function scoring in 100 fluctuating PD patients. ΔNMSSOn/Off was defined as the differences of NMSS scores between On and Off. Complete NMSS datasets were available from 73 patients (53 % men; age: 68.2 ± 9.7 years) with mean total NMSS score in On state of 41.5 ± 37.6 and in Off state of 75.6 ± 42.3 (P < 0.001). Scores were higher in Off compared to On state for all domains except for domain “perceptual problems/hallucinations” (P = 0.608). Clinimetric properties of the NMSS were similar to those reported previously for NMS assessments independent of motor oscillations. NMSSOn, NMSSOff and ΔNMSSOn/Off showed weak to moderate correlations with demographics, indicators of motor symptom severity as well as with other measures of NMS, depression and quality of life. Correlations of NMSS items/domains with independent measures of related constructs were weak to moderate. In conclusion, when assessed with the NMSS, a broad range of NMS fluctuate with motor oscillations, but these fluctuations do neither correlate with motor function nor with measures of disease progression.

Similar content being viewed by others
References
Bayulkem K, Lopez G (2011) Clinical approach to nonmotor sensory fluctuations in Parkinson’s disease. J Neurol Sci 310(1–2):82–85
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Calandrella D, Antonini A (2012) Pulsatile or continuous dopaminomimetic strategies in Parkinson’s disease. Parkinsonism Relat Disord 18(Suppl 1):S120–S122
Chaudhuri KR, Martinez-Martin P, Schapira AH, Stocchi F, Sethi K, Odin P, Brown RG, Koller W, Barone P, MacPhee G, Kelly L, Rabey M, MacMahon D, Thomas S, Ondo W, Rye D, Forbes A, Tluk S, Dhawan V, Bowron A, Williams AJ, Olanow CW (2006) International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Mov Disord 21(7):916–923
Chaudhuri KR, Martinez-Martin P, Brown RG, Sethi K, Stocchi F, Odin P, Ondo W, Abe K, Macphee G, Macmahon D, Barone P, Rabey M, Forbes A, Breen K, Tluk S, Naidu Y, Olanow W, Williams AJ, Thomas S, Rye D, Tsuboi Y, Hand A, Schapira AH (2007) The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov Disord 22(13):1901–1911
Chaudhuri KR, Rizos A, Sethi KD (2013a) Motor and nonmotor complications in Parkinson’s disease: an argument for continuous drug delivery? J Neural Transm 120(9):1305–1320
Chaudhuri KR, Rojo JM, Schapira AH, Brooks DJ, Stocchi F, Odin P, Antonini A, Brown RJ, Martinez-Martin P (2013b) A proposal for a comprehensive grading of Parkinson’s disease severity combining motor and non-motor assessments: meeting an unmet need. PLoS One 8(2):e57221
Cockrell JR, Folstein MF (1988) Mini-mental state examination (MMSE). Psychopharmacol Bull 24(4):689–692
D’Amato RJ, Zweig RM, Whitehouse PJ, Wenk GL, Singer HS, Mayeux R, Price DL, Snyder SH (1987) Aminergic systems in Alzheimer’s disease and Parkinson’s disease. Ann Neurol 22(2):229–236
Dickson DW, Braak H, Duda JE, Duyckaerts C, Gasser T, Halliday GM, Hardy J, Leverenz JB, Del Tredici K, Wszolek ZK, Litvan I (2009) Neuropathological assessment of Parkinson’s disease: refining the diagnostic criteria. Lancet Neurol 8(12):1150–1157
Fahn S, Elton RL, Committee UD (1987) The unified Parkinson’s disease rating scale. In: Fahn S, Marsden CD, Calne DB (eds) Recent developments in Parkinson’s disease., vol 2. Macmillan Healthcare Information, Florham Park, pp 153–163, 293–304
Ferketich SL, Figueredo AJ, Knapp TR (1991) The multitrait-multimethod approach to construct validity. Res Nurs Health 14(4):315–320
Gallagher DA, Schrag A (2012) Psychosis, apathy, depression and anxiety in Parkinson’s disease. Neurobiol Disease 46(3):581–589
Gallagher DA, Lees AJ, Schrag A (2010) What are the most important nonmotor symptoms in patients with Parkinson’s disease and are we missing them? Mov Disord 25(15):2493–2500
Hillen ME, Sage JI (1996) Nonmotor fluctuations in patients with Parkinson’s disease. Neurology 47(5):1180–1183
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17(5):427–442
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55(3):181–184
Kulisevsky J, Pascual-Sedano B, Barbanoj M, Gironell A, Pagonabarraga J, Garcia-Sanchez C (2007) Acute effects of immediate and controlled-release levodopa on mood in Parkinson’s disease: a double-blind study. Mov Disord 22(1):62–67
Kuopio AM, Marttila RJ, Helenius H, Toivonen M, Rinne UK (2000) The quality of life in Parkinson’s disease. Mov Disord 15(2):216–223
Martinez-Martin P, Rodriguez-Blazquez C, Abe K, Bhattacharyya KB, Bloem BR, Carod-Artal FJ, Prakash R, Esselink RA, Falup-Pecurariu C, Gallardo M, Mir P, Naidu Y, Nicoletti A, Sethi K, Tsuboi Y, van Hilten JJ, Visser M, Zappia M, Chaudhuri KR (2009) International study on the psychometric attributes of the non-motor symptoms scale in Parkinson disease. Neurology 73(19):1584–1591
Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM, Chaudhuri KR (2011) The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov Disord 26(3):399–406
McHorney CA, Tarlov AR (1995) Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res 4(4):293–307
Muller CM, de Vos RA, Maurage CA, Thal DR, Tolnay M, Braak H (2005) Staging of sporadic Parkinson disease-related alpha-synuclein pathology: inter- and intra-rater reliability. J Neuropathol Exp Neurol 64(7):623–628
Nebe A, Ebersbach G (2009) Pain intensity on and off levodopa in patients with Parkinson’s disease. Mov Disord 24(8):1233–1237
Peto V, Jenkinson C, Fitzpatrick R, Greenhall R (1995) The development and validation of a short measure of functioning and well being for individuals with Parkinson’s disease. Qual Life Res 4(3):241–248
Saper CB, Sorrentino DM, German DC, de Lacalle S (1991) Medullary catecholaminergic neurons in the normal human brain and in Parkinson’s disease. Ann Neurol 29(6):577–584
Schrag A, Jahanshahi M, Quinn N (2000) What contributes to quality of life in patients with Parkinson’s disease? J Neurol Neurosurg Psychiatry 69(3):308–312
Seki M, Takahashi K, Uematsu D, Mihara B, Morita Y, Isozumi K, Ohta K, Muramatsu K, Shirai T, Nogawa S, Gotoh J, Yamaguchi K, Tomita Y, Yasutomi D, Nihei Y, Iwasawa S, Suzuki N (2013) Clinical features and varieties of non-motor fluctuations in Parkinson’s disease: a Japanese multicenter study. Parkinsonism Relat Disord 19(1):104–108
Siemers ER, Shekhar A, Quaid K, Dickson H (1993) Anxiety and motor performance in Parkinson’s disease. Mov Disord 8(4):501–506
Stacy MA, Murphy JM, Greeley DR, Stewart RM, Murck H, Meng X (2008) The sensitivity and specificity of the 9-item wearing-off questionnaire. Parkinsonism Relat Disord 14(3):205–212
Storch A, Odin P, Trender-Gerhard I, Fuchs G, Reifschneider G, Chaudhuri KR, Jost WH, Ebersbach G (2010) Non-motor Symptoms Questionnaire and Scale for Parkinson’s disease. Cross-cultural adaptation into the German language. Der Nervenarzt 81(8):980–985
Storch A, Schneider CB, Wolz M, Sturwald Y, Nebe A, Odin P, Mahler A, Fuchs G, Jost WH, Chaudhuri KR, Koch R, Reichmann H, Ebersbach G (2013) Nonmotor fluctuations in Parkinson disease: severity and correlation with motor complications. Neurology 80(9):800–809
Witjas T, Kaphan E, Azulay JP, Blin O, Ceccaldi M, Pouget J, Poncet M, Cherif AA (2002) Nonmotor fluctuations in Parkinson’s disease: frequent and disabling. Neurology 59(3):408–413
Wolz M, Hauschild J, Fauser M, Klingelhofer L, Reichmann H, Storch A (2012) Immediate effects of deep brain stimulation of the subthalamic nucleus on nonmotor symptoms in Parkinson’s disease. Parkinsonism Relat Disord 18:994–997
Acknowledgments
We acknowledge all collaborators of the NoMoFlu-PD study group and the international Parkinson’s disease non motor group who have contributed to the concept of this work. The NoMoFlu-PD Study Group consists of the following structure: NoMoFlu PD steering committee K. Ray Chaudhuri, National Parkinson Foundation Centre of Excellence, Kings College Hospital and Kings College London and Biomedical Research Centre, Kings College London, UK; Georg Ebersbach, Movement Disorders Clinic, Beelitz-Heilstätten, Germany; Gerd Fuchs, Parkinson Clinic Wolfach, Wolfach, Germany; Wolfgang H. Jost, Department of Neurology, Deutsche Klinik für Diagnostik, Wiesbaden, Germany; Per Odin, Department of Neurology, Klinikum Bremerhaven, Bermerhaven, Germany; Alexander Storch, Division of Neurodegenerative Diseases, Department of Neurology, Technische Universität Dresden, and German Centre for Neurodegenerative Diseases (DZNE) Dresden, Dresden, Germany. Participating centers and investigators Division of Neurodegenerative Diseases, Department of Neurology, Technische Universität Dresden, and German Centre for Neurodegenerative Diseases (DZNE) Dresden, Dresden, Germany (Drs. Storch, Schneider, Wolz, Klingelhöfer, Fauser, Reichmann, Melzer, Stürwald, Schmidt [study nurse], A. Wolz [study nurse], C. Bosredon [study nurse]); Movement Disorders Clinic, Beelitz-Heilstätten, Germany (Drs. Nebe, Ebersbach); Department of Neurology, Klinikum Bremerhaven, Bremerhaven, Germany (Gies, Drs. Odin, Mahler); Parkinson Clinic Wolfach, Wolfach, Germany (Dr. Fuchs); Department of Neurology, Deutsche Klinik für Diagnostik, Wiesbaden, Germany (Dr. Jost). Statistical analysis Dr. Koch (Department of Biometrics and Medical Informatics, Dresden University of Technology); Drs. Storch, Schneider (Division of Neurodegenerative Diseases, Department of Neurology, Technische Universität Dresden). Drs. Storch, Schneider and Koch had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
AS has received unrestricted research grants from Boehringer Ingelheim, TEVA and GKC, honoraria for presentations/lectures or advisory boards from Boehringer Ingelheim, AbbVie, TEVA, Archimedes, UCB Pharma, Orion, Novartis, Lundbeck, TEVA, MEDA, GSK, NeuroConsil, Desitin, and Mundipharma, and consultancy fees from Boehringer Ingelheim, Britannia, GKC Melbourne, Mundipharma. CBS, LK, PM-M and RK have nothing to disclose. PO has received honoraria for presentations/lectures or advisory boards from AbbVie, Britannia, UCB Pharma, Orion, TEVA, Biogen, and consultancy fees from AbbVie. GF and GE have received honoraria for presentations/lectures or advisory boards from Boehringer Ingelheim. WHJ has received honoraria for presentations/lectures or advisory boards from Boehringer Ingelheim, TEVA, Desitin, GSK. HR was acting on advisory boards and gave lectures and received research grants from Biogen, Bayer Health Care, Boehringer/Ingelheim, Cephalon, Desitin, GSK, Merck-Serono, Novartis, Orion, Pfizer, AbbVie, TEVA/Lundbeck, UCB Schwarz Pharma, and MEDA. KRC has received unrestricted research grants from Boehringer Ingelheim, UCB and AbbVie, honoraria for presentations/lectures or advisory boards from Boehringer Ingelheim, AbbVie, UCB Pharma, Britannia, Medtronic, GSK and Mundipharma, and consultancy fees from Boehringer Ingelheim, Britannia, AbbVie, GSK, Medtronic, UCB and Mundipharma.
Funding sources
This study was supported in part by an unrestricted research grant from Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany. The financial sponsors of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had the final responsibility for the decision to submit for publication.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Storch, A., Schneider, C.B., Klingelhöfer, L. et al. Quantitative assessment of non-motor fluctuations in Parkinson’s disease using the Non-Motor Symptoms Scale (NMSS). J Neural Transm 122, 1673–1684 (2015). https://doi.org/10.1007/s00702-015-1437-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-015-1437-x