Abstract
Purpose
Postoperative morbidity in glioblastoma (GBM) patients can be due to the disease course but can also come from postoperative complications. Our objective was to study the association of dexamethasone use and perioperative hyperglycemia with postoperative complications in GBM patients.
Methods
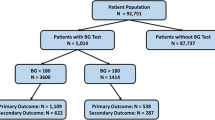
A single-center, retrospective cohort study was conducted in patients who underwent surgery for primary GBM from 2014–2018. Patients with perioperative fasting blood glucose (FBG) measurements and adequate follow-up to assess for complications were included.
Results
A total of 199 patients were included. More than half (53%) had poor perioperative glycemic control (FBG ≥ 7 mM for ≥ 20% perioperative days). Higher dexamethasone dose (≥ 8 mg) was associated with higher FBG on postoperative days 2–4 and 5 (p = 0.02,0.05,0.004,0.02, respectively). Poor glycemic control was associated with increased odds of 30-day any complication and 30-day infection on univariate analysis (UVA), and 30-day any complication and increased length of stay (LOS) on multivariate analysis (MVA). Higher average perioperative daily dexamethasone dose was associated with increased odds of 30-day any complication and 30-day infection on MVA. Elevated hemoglobin A1c (HgbA1c, ≥ 6.5%) was associated with increased odds of 30-day any complication, 30-day infection, and LOS on UVA. In a multivariate linear regression model, only the diagnosis of diabetes mellitus predicted perioperative hyperglycemia.
Conclusions
Perioperative hyperglycemia, higher average dexamethasone use and elevated preoperative HgbA1c are associated with increased risk of postoperative complications in GBM patients. Avoiding hyperglycemia and limiting dexamethasone use in postoperative period may decrease the risk of complications. Select HgbA1c screening may allow the identification of a group of patients at higher risk of complications.


Similar content being viewed by others
Data Availability
Data available on request from the authors, contingent on approval from local ethics board.
References
American Diabetes Association Professional Practice C (2022) 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care 45:S17-S38. https://doi.org/10.2337/dc22-S002
Bae SH, Park MJ, Lee MM, Kim TM, Lee SH, Cho SY, Kim YH, Kim YJ, Park CK, Kim CY (2014) Toxicity profile of temozolomide in the treatment of 300 malignant glioma patients in Korea. J Korean Med Sci 29:980–984. https://doi.org/10.3346/jkms.2014.29.7.980
Cannarsa GJ, Wessell AP, Chryssikos T, Stokum JA, Kim K, De Paula CH, Miller TR, Morris N, Badjatia N, Chaturvedi S, Gandhi D, Simard JM, Jindal G (2022) Initial Stress Hyperglycemia Is Associated With Malignant Cerebral Edema, Hemorrhage, and Poor Functional Outcome After Mechanical Thrombectomy. Neurosurgery 90:66–71. https://doi.org/10.1227/neu.0000000000001735
Decker M, Sacks P, Abbatematteo J, De Leo E, Brennan M, Rahman M (2019) The effects of hyperglycemia on outcomes in surgical high-grade glioma patients. Clin Neurol Neurosurg 179:9–13. https://doi.org/10.1016/j.clineuro.2019.02.011
Diabetes Canada Clinical Practice Guidelines Expert C, Punthakee Z, Goldenberg R, Katz P (2018) Definition, Classification and Diagnosis of Diabetes, Prediabetes and Metabolic Syndrome. Can J Diabetes 42 Suppl 1:S10-S15. https://doi.org/10.1016/j.jcjd.2017.10.003
Ferroni P, Roselli M, Riondino S, Cavaliere F, Guadagni F (2016) Insulin resistance as a predictor of venous thromboembolism in breast cancer. Endocr Relat Cancer 23:L25-28. https://doi.org/10.1530/ERC-16-0187
Fong AC, Cheung NW (2013) The high incidence of steroid-induced hyperglycaemia in hospital. Diabetes Res Clin Pract 99:277–280. https://doi.org/10.1016/j.diabres.2012.12.023
Grabowski MM, Recinos PF, Nowacki AS, Schroeder JL, Angelov L, Barnett GH, Vogelbaum MA (2014) Residual tumor volume versus extent of resection: predictors of survival after surgery for glioblastoma. J Neurosurg 121:1115–1123. https://doi.org/10.3171/2014.7.JNS132449
Guadagni F, Riondino S, Formica V, Del Monte G, Morelli AM, Lucchetti J, Spila A, D’Alessandro R, Della-Morte D, Ferroni P, Roselli M (2017) Clinical significance of glycemic parameters on venous thromboembolism risk prediction in gastrointestinal cancer. World J Gastroenterol 23:5187–5195. https://doi.org/10.3748/wjg.v23.i28.5187
Hagan K, Bhavsar S, Arunkumar R, Grasu R, Dang A, Carlson R, Cowles C, Arnold B, Potylchansky Y, Rahlfs TF, Lipski I, Walsh C, Jimenez F, Nguyen AT, Feng L, Cata JP (2017) Association Between Perioperative Hyperglycemia and Survival in Patients With Glioblastoma. J Neurosurg Anesthesiol 29:21–29. https://doi.org/10.1097/ANA.0000000000000339
Hanif F, Muzaffar K, Perveen K, Malhi SM, Simjee ShU (2017) Glioblastoma Multiforme: A Review of its Epidemiology and Pathogenesis through Clinical Presentation and Treatment. Asian Pac J Cancer Prev 18:3–9. https://doi.org/10.22034/APJCP.2017.18.1.3
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JE, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003. https://doi.org/10.1056/NEJMoa043331
Incekara F, Smits M, van der Voort SR, Dubbink HJ, Atmodimedjo PN, Kros JM, Vincent A, van den Bent M (2020) The Association Between the Extent of Glioblastoma Resection and Survival in Light of MGMT Promoter Methylation in 326 Patients With Newly Diagnosed IDH-Wildtype Glioblastoma. Front Oncol 10:1087. https://doi.org/10.3389/fonc.2020.01087
Jafar N, Edriss H, Nugent K (2016) The Effect of Short-Term Hyperglycemia on the Innate Immune System. Am J Med Sci 351:201–211. https://doi.org/10.1016/j.amjms.2015.11.011
Jiang SHK, Patel D, Waldeck AR, Botteman M, Aly A, Norden AD (2017) Direct medical costs of treatment in newly-diagnosed high-grade glioma among commercially insured US patients. J Med Econ 20:1237–1243. https://doi.org/10.1080/13696998.2017.1364258
Kostaras X, Cusano F, Kline GA, Roa W, Easaw J (2014) Use of dexamethasone in patients with high-grade glioma: a clinical practice guideline. Curr Oncol 21:e493-503. https://doi.org/10.3747/co.21.1769
Lieber BA, Han J, Appelboom G, Taylor BE, Han B, Agarwal N, Connolly ES Jr (2016) Association of Steroid Use with Deep Venous Thrombosis and Pulmonary Embolism in Neurosurgical Patients: A National Database Analysis. World Neurosurg 89:126–132. https://doi.org/10.1016/j.wneu.2016.01.033
Lim S, Yeh HH, Macki M, Mansour T, Schultz L, Telemi E, Haider S, Nerenz DR, Schwalb JM, Abdulhak M, Park P, Aleem I, Easton R, Khalil J, Perez-Cruet M, Chang V (2021) Preoperative HbA1c > 8% Is Associated With Poor Outcomes in Lumbar Spine Surgery: A Michigan Spine Surgery Improvement Collaborative Study. Neurosurgery 89:819–826. https://doi.org/10.1093/neuros/nyab294
Link TW, Woodworth GF, Chaichana KL, Grossman SA, Mayer RS, Brem H, Weingart JD, Quinones-Hinojosa A (2012) Hyperglycemia is independently associated with post-operative function loss in patients with primary eloquent glioblastoma. J Clin Neurosci 19:996–1000. https://doi.org/10.1016/j.jocn.2011.09.031
Liu H, Liu Z, Jiang B, Ding X, Huo L, Wan X, Liu J, Xia Z (2016) Prognostic Significance of Hyperglycemia in Patients with Brain Tumors: a Meta-Analysis. Mol Neurobiol 53:1654–1660. https://doi.org/10.1007/s12035-015-9115-4
McClelland S 3rd, Hall WA (2007) Postoperative central nervous system infection: incidence and associated factors in 2111 neurosurgical procedures. Clin Infect Dis 45:55–59. https://doi.org/10.1086/518580
Mistry AM, Jonathan SV, Monsour MA, Mobley BC, Clark SW, Moots PL (2021) Impact of postoperative dexamethasone on survival, steroid dependency, and infections in newly diagnosed glioblastoma patients. Neurooncol Pract 8:589–600. https://doi.org/10.1093/nop/npab039
Molinaro AM, Hervey-Jumper S, Morshed RA, Young J, Han SJ, Chunduru P, Zhang Y, Phillips JJ, Shai A, Lafontaine M, Crane J, Chandra A, Flanigan P, Jahangiri A, Cioffi G, Ostrom Q, Anderson JE, Badve C, Barnholtz-Sloan J, Sloan AE, Erickson BJ, Decker PA, Kosel ML, LaChance D, Eckel-Passow J, Jenkins R, Villanueva-Meyer J, Rice T, Wrensch M, Wiencke JK, Oberheim Bush NA, Taylor J, Butowski N, Prados M, Clarke J, Chang S, Chang E, Aghi M, Theodosopoulos P, McDermott M, Berger MS (2020) Association of Maximal Extent of Resection of Contrast-Enhanced and Non-Contrast-Enhanced Tumor With Survival Within Molecular Subgroups of Patients With Newly Diagnosed Glioblastoma. JAMA Oncol 6:495–503. https://doi.org/10.1001/jamaoncol.2019.6143
Mor V, Laliberte L, Morris JN, Wiemann M (1984) The Karnofsky Performance Status Scale. An examination of its reliability and validity in a research setting. Cancer 53:2002–2007. https://doi.org/10.1002/1097-0142(19840501)53:9<2002::aid-cncr2820530933>3.0.co;2-w
Nazar CE, Lacassie HJ, Lopez RA, Munoz HR (2009) Dexamethasone for postoperative nausea and vomiting prophylaxis: effect on glycaemia in obese patients with impaired glucose tolerance. Eur J Anaesthesiol 26:318–321. https://doi.org/10.1097/EJA.0b013e328319c09b
Oppenlander ME, Wolf AB, Snyder LA, Bina R, Wilson JR, Coons SW, Ashby LS, Brachman D, Nakaji P, Porter RW, Smith KA, Spetzler RF, Sanai N (2014) An extent of resection threshold for recurrent glioblastoma and its risk for neurological morbidity. J Neurosurg 120:846–853. https://doi.org/10.3171/2013.12.JNS13184
Rethinasamy R, Alias A, Kandasamy R, Raffiq A, Looi MC, Hillda T (2019) Deep Vein Thrombosis and the Neurosurgical Patient. Malays J Med Sci 26:139–147. https://doi.org/10.21315/mjms2019.26.5.13
Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS (2011) An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg 115:3–8. https://doi.org/10.3171/2011.2.JNS10998
Schipmann S, Akalin E, Doods J, Ewelt C, Stummer W, Suero Molina E (2016) When the Infection Hits the Wound: Matched Case-Control Study in a Neurosurgical Patient Collective Including Systematic Literature Review and Risk Factors Analysis. World Neurosurg 95:178–189. https://doi.org/10.1016/j.wneu.2016.07.093
Schultz H, Rasmussen BK, Kristensen PL, Jensen AK, Pedersen-Bjergaard U (2018) Early incidence of glucocorticoid-induced diabetes in patients with brain tumors: a retrospective study of the first 7 days of treatment. Neurooncol Pract 5:170–175. https://doi.org/10.1093/nop/npx027
Senders JT, Goldhaber NH, Cote DJ, Muskens IS, Dawood HY, De Vos F, Gormley WB, Smith TR, Broekman MLD (2018) Venous thromboembolism and intracranial hemorrhage after craniotomy for primary malignant brain tumors: a National Surgical Quality Improvement Program analysis. J Neurooncol 136:135–145. https://doi.org/10.1007/s11060-017-2631-5
Sharma M, Bellamkonda S, Mohapatra S, Meola A, Jia X, Mohammadi A, Angelov L, Barnett GH, Vogelbaum M, Ahluwalia MS (2018) Correlation Between the Residual Tumor Volume, Extent of Tumor Resection, and O(6)-Methylguanine DNA Methyltransferase Status in Patients with Glioblastoma. World Neurosurg 116:e147–e161. https://doi.org/10.1016/j.wneu.2018.04.134
Thakkar JP, Dolecek TA, Horbinski C, Ostrom QT, Lightner DD, Barnholtz-Sloan JS, Villano JL (2014) Epidemiologic and molecular prognostic review of glioblastoma. Cancer Epidemiol Biomarkers Prev 23:1985–1996. https://doi.org/10.1158/1055-9965.EPI-14-0275
von Kanel R, Mills PJ, Dimsdale JE (2001) Short-term hyperglycemia induces lymphopenia and lymphocyte subset redistribution. Life Sci 69:255–262. https://doi.org/10.1016/s0024-3205(01)01127-4
Wang YY, Hu SF, Ying HM, Chen L, Li HL, Tian F, Zhou ZF (2018) Postoperative tight glycemic control significantly reduces postoperative infection rates in patients undergoing surgery: a meta-analysis. BMC Endocr Disord 18:42. https://doi.org/10.1186/s12902-018-0268-9
Yuksel S, Ugras GA, Sirin K, Turan Y, Kurucu S (2020) Stress hyperglycemia and glycemic control in critical neurosurgical patients: A retrospective study. Ann Med Res 27:2298–2305. https://doi.org/10.5455/annalsmedres.2020.05.451
Acknowledgements
We would like to thank Dr. Kevin Petrecca, Dr. David Sinclair, and Dr. Abbas Sadikot for their comments. We also acknowledge Dr. Marie-Christine Guiot for assistance in identifying GBM patients from the neuropathology register. We also extend our gratitude to all the members of the healthcare team involved in brain tumor patient care at the MNH, including the neurosurgeons, nursing team, occupational therapists, physiotherapists, respiratory therapists and social workers.
Funding
This study recognizes funding from McGill University Health Centre Department of Neurosurgery Foundation, granted to Dr. Roberto Jose Diaz. All authors of this study have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tumor – Glioma
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jatana, S., Mohammad, A.H., Al-Saadi, T.D. et al. Characterization of perioperative glycemic status and dexamethasone use with associated postoperative complications in glioblastoma patients. Acta Neurochir 165, 1031–1040 (2023). https://doi.org/10.1007/s00701-023-05541-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05541-6