Abstract
Background
Intracranial multimodality monitoring (iMMM) is increasingly used in acute brain-injured patients; however, safety and reliability remain major concerns to its routine implementation.
Methods
We performed a retrospective study including all patients undergoing iMMM at a single European center between July 2016 and January 2020. Brain tissue oxygenation probe (PbtO2), alone or in combination with a microdialysis catheter and/or an 8-contact depth EEG electrode, was inserted using a triple-lumen bolt system and targeting normal-appearing at-risk brain area on the injured side, whenever possible. Surgical complications, adverse events, and technical malfunctions, directly associated with iMMM, were collected. A blinded imaging review was performed by an independent radiologist.
Results
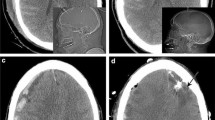
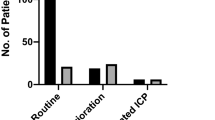
One hundred thirteen patients with 123 iMMM insertions were included for a median monitoring time of 9 [3–14] days. Of those, 93 (76%) patients had only PbtO2 probe insertion and 30 (24%) had also microdialysis and/or iEEG monitoring. SAH was the most frequent indication for iMMM (n = 60, 53%). At least one complication was observed in 67/123 (54%) iMMM placement, corresponding to 58/113 (51%) patients. Misplacement was observed in 16/123 (13%), resulting in a total of 6/16 (38%) malfunctioning PbtO2 catheters. Intracranial hemorrhage was observed in 14 iMMM placements (11%), of which one required surgical drainage. Five placements were complicated by pneumocephalus and 4 with bone fragments; none of these requires additional surgery. No CNS infection related to iMMM was observed. Seven (6%) probes were accidentally dislodged and 2 probes (2%) were accidentally broken. Ten PbtO2 probes (8%) presented a technical malfunction after a median of 9 [ranges: 2–24] days after initiation of monitoring and 4 of them were replaced.
Conclusions
In this study, a high occurrence of complications related to iMMM was observed, although most of them did not require specific interventions and did not result in malfunctioning monitoring.


Similar content being viewed by others
Availability of data and material
All the data are available on demand at mejdi.albarajraji@gmail.com.
Code availability
Not applicable.
References
Chin JH, Vora N (2014) The global burden of neurologic diseases. Neurology 83(4):349–351. https://doi.org/10.1212/WNL.0000000000000610
Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung YC, Punchak M, Agrawal A, Adeleye AO, Shrime MG, Rubiano AM, Rosenfeld JV, Park KB (2018) Estimating the global incidence of traumatic brain injury. Journal of neurosurgery, 1–18. Advance online publication. https://doi.org/10.3171/2017.10.JNS17352
Le Roux P, Menon DK, Citerio G, Vespa P, Bader MK, Brophy GM, Diringer MN, Stocchett N, Videtta W, Armonda R, Badjatia N, Böesel J, Chesnut R, Chou S, Claassen J, Czosnyka M, De Georgia M, Figaji A, Fugate J, Helbok R, Horowitz D, Hutchinson P, Kumar M, McNett M, Miller C, Naidech A, Oddo M, Olson D, O’Phelan K, Provencio JJ, Puppo C, Riker R, Robertson C, Schmidt M, Taccone F, Neurocritical Care Society; European Society of Intensive Care Medicine (2014) Consensus summary statement of the International Multidisciplinary Consensus Conference on Multimodality Monitoring in Neurocritical Care: a statement for healthcare professionals from the Neurocritical Care Society and the European Society of Intensive Care Medicine. Intensive care medicine 40(9):1189–1209. https://doi.org/10.1007/s00134-014-3369-6
Bailey RL, Quattrone F, Curtin C, Frangos S, Maloney-Wilensky E, Levine JM, LeRoux PD (2019) The safety of multimodality monitoring using a triple-lumen bolt in severe acute brain injury. World neurosurgery 130:e62–e67. https://doi.org/10.1016/j.wneu.2019.05.195
Hawryluk G, Aguilera S, Buki A, Bulger E, Citerio G, Cooper DJ, Arrastia RD, Diringer M, Figaji A, Gao G, Geocadin R, Ghajar J, Harris O, Hoffer A, Hutchinson P, Joseph M, Kitagawa R, Manley G, Mayer S, Menon DK, Meyfroidt G, Michael DB, Oddo M, Okonkwo D, Patel M, Robertson C, Rosenfeld JV, Rubiano AM, Sahuquillo J, Servadei F, Shutter L, Stein D, Stocchetti N, Taccone FS, Timmons S, Tsai E, Ullman JS, Vespa P, Videtta W, Wright DW, Zammit C, Chesnut RM (2019) A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med 45(12):1783–1794. https://doi.org/10.1007/s00134-019-05805-9
Alali AS, Fowler RA, Mainprize TG, Scales DC, Kiss A, de Mestral C, Ray JG, Nathens AB (2013) Intracranial pressure monitoring in severe traumatic brain injury: results from the American College of Surgeons Trauma Quality Improvement Program. J Neurotrauma 30(20):1737–1746. https://doi.org/10.1089/neu.2012.2802
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ, Bratton SL, Chesnut R, Harris OA, Kissoon N, Rubiano AM, Shutter L, Tasker RC, Vavilala MS, Wilberger J, Wright DW, Ghajar J (2017) Guidelines for the management of severe traumatic brain injury. Fourth Edition Neurosurgery 80(1):6–15. https://doi.org/10.1227/NEU.0000000000001432
Farahvar A, Gerber LM, Chiu YL, Carney N, Härtl R, Ghajar J (2012) Increased mortality in patients with severe traumatic brain injury treated without intracranial pressure monitoring. J Neurosurg 117(4):729–734. https://doi.org/10.3171/2012.7.JNS111816
Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W, Petroni G, Lujan S, Pridgeon J, Barber J, Machamer J, Chaddock K, Celix JM, Cherner M, Hendrix T, Global Neurotrauma Research Group (2012) A trial of intracranial-pressure monitoring in traumatic brain injury. The New England journal of medicine 367(26):2471–2481. https://doi.org/10.1056/NEJMoa1207363
Roh D, Park S (2016) Brain multimodality monitoring: updated perspectives. Curr Neurol Neurosci Rep 16(6):56. https://doi.org/10.1007/s11910-016-0659-0
Citerio G, Oddo M, Taccone FS (2015) Recommendations for the use of multimodal monitoring in the neurointensive care unit. Curr Opin Crit Care 21(2):113–119. https://doi.org/10.1097/MCC.0000000000000179
Foreman B, Ngwenya LB, Stoddard E, Hinzman JM, Andaluz N, Hartings JA (2018) Safety and reliability of bedside, single burr hole technique for intracranial multimodality monitoring in severe traumatic brain injury. Neurocrit Care 29(3):469–480. https://doi.org/10.1007/s12028-018-0551-7
Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G (2014) The Glasgow Coma Scale at 40 years: standing the test of time. The Lancet Neurology 13(8):844–854. https://doi.org/10.1016/S1474-4422(14)70120-6
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13(10):818–829
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive care medicine 22(7):707–710. https://doi.org/10.1007/BF01709751
Samaniego EA, Hasan DM (2019) In Reply: External ventricular drain and hemorrhage in aneurysmal subarachnoid hemorrhage patients on dual antiplatelet therapy: a retrospective cohort study. Neurosurgery 84(1):E99–E100. https://doi.org/10.1093/neuros/nyy489
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36(5):309–332. https://doi.org/10.1016/j.ajic.2008.03.002
Dings J, Meixensberger J, Jäger A, Roosen K (1998) Clinical experience with 118 brain tissue oxygen partial pressure catheter probes. Neurosurgery 43(5):1082–1095. https://doi.org/10.1097/00006123-199811000-00045
Stuart RM, Schmidt M, Kurtz P, Waziri A, Helbok R, Mayer SA, Lee K, Badjatia N, Hirsch LJ, Connolly ES, Claassen J (2010) Intracranial multimodal monitoring for acute brain injury: a single institution review of current practices. Neurocrit Care 12(2):188–198. https://doi.org/10.1007/s12028-010-9330-9
van Santbrink H, Maas AI, Avezaat CJ (1996) Continuous monitoring of partial pressure of brain tissue oxygen in patients with severe head injury. Neurosurgery 38(1):21–31. https://doi.org/10.1097/00006123-199601000-00007
Tavakoli S, Peitz G, Ares W, Hafeez S, Grandh R (2017) Complications of invasive intracranial pressure monitoring devices in neurocritical care. Neurosurg Focus 43(5):E6. https://doi.org/10.3171/2017.8.FOCUS17450
Funding
The research was not supported by any company. The devices were bought by the intensive care unit and the neurosurgery department to be used in daily clinical practice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained from ethics committees of the Erasme Hospital, Free University of Brussels, Brussels, Belgium: file EC P2020/019.
Additional declarations for articles in life science journals that report the results of studies involving humans and/or animals
Not applicable.
Consent to participate
For this type of study, formal consent is not required.
Consent for publication
Consent to submit has been received from all co-authors and responsible authorities at the institute/organization where the work has been carried out before the work is submitted.
Competing interests
Fabio Silvio Taccone received lecture fees from Integra Lifescience. All other authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mejdeddine Al Barajraji and Elisa Bogossian equally contributed as first authors.
Sophie Schuind and Sami Barrit equally contributed as senior authors.
This article is part of the Topical Collection on Neurosurgical intensive care
Rights and permissions
About this article
Cite this article
Al Barajraji, M., Bogossian, E., Dewitte, O. et al. Safety profile of an intracranial multimodal monitoring bolt system for neurocritical care: a single-center experience. Acta Neurochir 163, 3259–3266 (2021). https://doi.org/10.1007/s00701-021-04992-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-021-04992-z