Abstract
Background
A larger defect in the annulus fibrosus following lumbar discectomy is a well-known risk factor for reherniation. Procedures intended to prevent reherniation by sealing or occluding the annular defect warrant study in high-risk patients. This study sought to determine 3-year results of lumbar discectomy with a bone-anchored annular closure device (ACD) or lumbar discectomy only (controls) in patients at high risk for reherniation.
Methods
This multicenter randomized trial enrolled patients with sciatica due to lumbar intervertebral disc herniation who failed conservative treatment. Patients with large annular defects after lumbar limited microdiscectomy were intraoperatively randomly assigned to receive ACD or control. Clinical and imaging follow-up was performed at routine intervals over 3 years. Main outcomes included rate of reherniations, reoperations, and endplate changes; leg and back pain scores on a visual analogue scale; Oswestry Disability Index (ODI); Physical Component Summary (PCS) and Mental Component Summary (MCS) scores from the SF-36; and adverse events adjudicated by a data safety monitoring board.
Results
Among 554 randomized patients, the modified intent-to-treat population consisted of 272 patients in which ACD implantation was attempted and 278 receiving control; device implantation was not attempted in 4 patients assigned to ACD. Outcomes at 3 years favored ACD for symptomatic reherniation (14.8% vs. 29.5%; P < 0.001), reoperation (11.0% vs. 19.3%; P = 0.007), leg pain (21 vs. 30; P < 0.01), back pain (23 vs. 30; P = 0.01), ODI (18 vs. 23; P = 0.02), PCS (47 vs. 44; P < 0.01), and MCS (52 vs. 49; P < 0.01). The frequency of all-cause serious adverse events was comparable between groups (42.3% vs. 44.5%; P = 0.61).
Conclusions
The addition of a bone-anchored ACD in patients with large annular defects following lumbar discectomy reduces the risk of reherniation and reoperation, and has a similar safety profile over 3-year follow-up compared with lumbar limited discectomy only.
Trial registration
ClinicalTrials.gov NCT01283438
Similar content being viewed by others
Introduction
Lumbar discectomy is an effective surgery for chronic sciatica secondary to intervertebral disc herniation. However, symptom recurrence following surgery is a common risk that is influenced by patient- and surgery-related factors such as male sex, disc degeneration, and large post-surgical annular defect size [8]. Patients with a post-surgical annular defect of at least 6 mm in width have a reherniation risk nearly three times higher compared with patients with smaller defects [13]. Consequently, adjunctive treatments intended to contain the nucleus pulposus within the disc space following discectomy have been studied. So far, results have been disappointing with sutures, fibrin glue, and polyethylene plug due to the failure of these materials to chronically withstand high intradiscal pressures [1, 2, 5, 7]. An implantable device intended to provide a more durable repair has been developed. This annular closure device (ACD) anchors into the adjacent vertebral body and occludes the damaged annulus fibrosus with a polymer mesh. Results from case series [4, 11, 12, 15] and a recent randomized trial [17] with this device have demonstrated clinically important reductions in reherniation and reoperation rates through 2 years. In this report, we extend these findings by presenting 3-year results from a randomized trial of 554 patients who received lumbar discectomy with bone-anchored annular closure or lumbar microdiscectomy only.
Materials and methods
This was a multicenter, multinational, randomized controlled trial to determine the effectiveness and safety of lumbar discectomy with a bone-anchored implant designed to provide annulus fibrosus occlusion in patients at high risk for reherniation (ClinicalTrials.gov NCT01283438). Local ethics committees reviewed and approved the protocol. All participants provided written informed consent before trial participation. The design [9] and 2-year primary endpoint results [17] of this trial have previously been described. This report presents 3-year clinical and radiographic results from the trial.
Preoperative imaging included magnetic resonance imaging (MRI) with T1- and T2-weighted axial and sagittal images, index-level low-dose multiplanar computed tomography (CT), and anteroposterior/lateral and flexion/extension x-rays. Important eligibility criteria for the study included diagnosis of a single-level lumbar disc herniation identified on preoperative imaging, and concurrent clinical findings (positive straight leg raise or femoral stretch test) with leg pain (≥ 40 on a 0–100 visual analogue scale) that were not responsive to at least 6 weeks of conservative treatment, and at least moderate disability (≥ 40 on the Oswestry Disability Index). A complete list of study entry criteria is provided in Supplement Table 1. Patients meeting these criteria were treated with limited lumbar microdiscectomy but were not yet enrolled in the study. When the discectomy procedure was completed, the final study entry criterion was applied. Patients with a large defect in the annulus fibrosus, defined as 4–6-mm height and 6–10-mm width, were enrolled in the study and randomly allocated (1:1) to receive discectomy only (controls) or to additionally receive a bone-anchored ACD with a mesh occlusion component (Barricaid, Intrinsic Therapeutics, Woburn, MA, USA) designed to physically block the annular defect. Patients with large annular defects were specifically targeted for this trial given their well-known high risk of reherniation after lumbar discectomy [13]. Following randomization, no additional disc material was removed in either treatment group. When annular defects of ineligible size were intraoperatively identified, the discectomy procedure was completed in the usual fashion and patients were discontinued from the study.
Clinical and imaging follow-up occurred at 6 weeks, 3 months, 6 months, and at annual intervals for 3 years and included MRI, low-dose CT, and AP/lateral and flexion/extension x-rays. Patients in this study will remain in follow-up for 5 years. A schematic that lists the clinical and imaging tests performed at each study interval is provided in Supplement Table 2. Symptomatic reherniation was defined as a reherniation (protrusion, extrusion, or sequestration) that was confirmed during a reoperation, or identified on imaging with associated recurrent or new lumbar pain, leg pain, or neurological deficit. Reoperation included any repeat procedure at the index level of herniation including discectomy, supplemental fixation, fusion, or device explant. Key radiographic assessment by x-ray and CT included disc height, device status, and vertebral endplate changes (VEPC). Imaging evaluations were read by an independent core laboratory radiologist who was blinded to clinical outcomes. Clinical outcome parameters included leg and back pain severity, Oswestry Disability Index (ODI), SF-36 Physical Component Summary (PCS) score, and SF-36 Mental Component Summary (MCS) score. The minimal important differences (MID) were defined as a ≥ 20-point decrease from baseline for leg pain [14], ≥ 20-point decrease from baseline for back pain [14], ≥ 15-point decrease from baseline for ODI [6], ≥ 5.7-point increase from baseline for PCS [18], and ≥ 6.3-point increase from baseline for MCS [18]. Neurological status and adverse events were assessed at each follow-up visit. Investigators classified adverse events by seriousness and relation to the device or procedure. Neither patients, surgeons, outcome assessors nor imaging core laboratory readers were blinded to group allocation, with the exception of patients in the Netherlands due to regional regulations. An independent data safety monitoring board provided safety oversight during the study and adjudicated all adverse events.
Statistical analyses were performed on a modified intention-to-treat population consisting of randomized patients in whom the intended procedure was attempted. Preoperative group characteristics were reported as mean and standard deviation for continuous variables, and count and percentage for categorical variables. Group comparisons were performed with Student’s t test for continuous data, Fisher’s exact test for categorical data, and log-rank tests for survival data. In patients who underwent a reoperation prior to the 3-year follow visit, leg pain, back pain, ODI, PCS, and MCS values at 3 years were substituted with baseline values. Statistical significance was set at P < 0.05 and hypothesis testing was two-sided. Statistical analyses were performed using SAS v9.4 (SAS Institute, Cary, NC, USA) and R v3.3.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 554 patients were randomly allocated to receive ACD (n = 276) or control (n = 278) at 21 hospitals (Study Group Appendix Table 4)) between December 2010 and October 2014. Annular closure device implantation was not attempted in four patients because of the close proximity of the nerve root and the associated potential risk. Therefore, the modified intention-to-treat population included 272 ACD patients and 278 control patients. Among the ACD group were 5 patients in which the device was unsuccessfully implanted due to incomplete entry of the occlusion mesh into the disc space (n = 4) or nerve root injury (n = 1). The mean age of all enrolled patients was 43 ± 11 years and 59% were men. Disc herniation was most commonly identified at L5-S1 (56%) or L4-L5 (41%). Patients typically presented with severe leg pain (overall mean 81 ± 15), severe disability (overall mean ODI 59 ± 13), and moderate back pain (overall mean 56 ± 31) (Table 1). Overall, 415 (75%) patients (207 ACD, 208 control) returned for clinical follow-up at 3 years (Fig. 1).
Enrollment and randomization of patients. Among 554 randomized patients, 276 were allocated to annular closure device (ACD) and 278 to control. Owing to 4 patients in whom ACD implant was not attempted, the modified intent-to-treat population consisted of 272 patients with attempted ACD implant and 278 patients assigned to control. Compliance with clinical follow-up at 3 years was 76% with ACD and 75% with controls
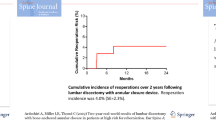
The risk of symptom recurrence through 3 years was lower in patients treated with ACD versus controls; the cumulative incidence of symptomatic reherniation was 8.4% vs. 17.4% at 1 year, 10.7% vs. 23.4% at 2 years, and 14.8% vs. 29.5% at 3 years (log-rank P < 0.001 at 3 years) (Fig. 2). Similarly, reoperations were less frequent in the ACD group, with cumulative reoperation rates of 6.7% vs. 12.9% at 1 year, 9.0% vs. 16.4% at 2 years, and 11.0% vs. 19.3% at 3 years (log-rank P < 0.001 at 3 years) (Fig. 3). There were 38 reoperations in 29 ACD patients and 70 reoperations in 51 control patients. Reoperation strategies between groups were similar with repeat discectomy performed most frequently (Table 2).
Patient-reported outcomes favored those treated with the ACD. Comparing ACD with controls, mean values at 3 years were 21 vs. 30 (mean difference = − 8, 95% CI = − 2 to − 15, P < 0.01) for leg pain, 23 vs. 30 (mean difference = − 7, 95% CI = − 1 to − 12, P = 0.01) for back pain, and 18 vs. 23 (mean difference = − 5, 95% CI = − 1 to − 9, P = 0.02) for ODI. Health-related quality of life scores at 3 years was higher in the ACD group; PCS scores were 47 vs. 44 (mean difference = 3, 95% CI = 1 to 5, P < 0.01) and MCS scores were 52 vs. 49 (mean difference = 3, 95% CI = 1 to 5, P < 0.01). The percentage of patients achieving the MID was statistically greater in the ACD group for leg pain, ODI, PCS, and MCS; no statistical difference between groups was noted for back pain (P = 0.08) (Fig. 4).
Percentage of patients achieving the minimal clinically important difference (MID) in patient-reported outcomes through 3 years. MID defined as improvement from baseline of at least 20 points for leg pain, 20 points for back pain, 15 points for Oswestry Disability Index (ODI), 5.7 points for Physical Component Score (PCS), and 6.3 points for Mental Component Score (MCS), respectively (all reported on 0–100 scale). Statistical significance between treatment groups denoted as *P < 0.05 or †P < 0.01. ACD, annular closure device
Disc height decreased by approximately 30% in each group relative to baseline. Average disc height at 3 years was 6.3 ± 2.2 mm with ACD and 6.4 ± 2.2 mm with controls (P = 0.64). Vertebral endplate changes were identified by the imaging core laboratory in 89% of ACD patients and in 41% of controls (P < 0.001). The median VEPC areas at 2- and 3-year follow-up were 0.42 cm3 and 0.49 cm3 with ACD, 0.29 cm2 and 0.42 cm2 for controls. Neither the frequency, area, nor growth trajectory of VEPC was associated with clinical sequelae.
Neurological function deterioration relative to baseline was reported in 2.0% of ACD patients and 4.3% of controls at 3 years (P = 0.26). Serious adverse events related to the device or procedure occurred in 10.7% of the ACD group and in 18.7% of controls (P = 0.008), and were mainly attributable to lumbar disc reherniation (Table 3). Serious adverse events due to device deficiency were reported in 12 (4.4%) patients in the ACD group and included mesh migration (n = 5), mesh detachment (n = 3), anchor migration (n = 3), and anchor fracture (n = 1). Reherniation was identified at the time of reoperation in four of these patients. The frequency of all serious adverse events (Supplement Table 3) and all adverse events regardless of seriousness (Supplement Table 4) was comparable between groups.
Discussion
A large unrepaired defect in the annulus fibrosus at completion of a lumbar discectomy procedure places patients at high risk for reherniation [13], which requires a reoperation in most cases to adequately resolve radicular symptoms [16]. In this randomized trial of high-risk patients, implantation with a bone-anchored ACD following limited lumbar discectomy reduced the risk of reherniation and reoperation and therefore achieved a better long-term pain and disability relief with associated higher levels of health-related quality of life compared with lumbar discectomy only. There were some specific risks to the ACD only, which included implantation difficulties, radiographic device deficiencies such as migration, mesh detachment, and VEPC. However, the overall safety profile was generally comparable between groups. These results suggest that lumbar discectomy with additional ACD implantation is an effective and safe procedure over 3-year follow-up in well-selected patients at high risk for reherniation owing to a large post-surgical annular defect.
Perhaps the most important finding of this trial relates to the ability of the ACD to lower the risk of recurrent herniation and reoperation among high-risk patients. This finding is notable given the previous failures of alternative annular defect closure methods such as sutures or fibrin glue [1, 2, 5, 7]. The fact that the mesh occlusion component is attached to an anchor within the vertebral body is the likely differentiating characteristic that offers a more durable annular occlusion. Several different mechanisms of device failure occurred, including mesh detachment, device migration, and anchor fracture. Most device failures were observed on follow-up imaging with no associated patient symptoms. However, device failure was associated with clinical sequelae in 4% of patients. All anchor migrations were observed within 3 months of surgery; two in patients with low regional bone density and one in a patient with multiple risk factors (heavy smoking, obesity, diabetes). It appears that device deficiencies, biomechanical forces, and/or patient characteristics may be causative factors involved in observed ACD failures.
Vertebral endplate changes detected on CT were more common among patients treated with ACD versus controls. While a detailed accounting of the association of VEPC with clinical outcomes is beyond the scope of this paper, the key findings warrant discussion. A noncontrolled study of 85 patients undergoing lumbar discectomy with or without additional ACD reported similar results where VEPC prevalence was higher in patients treated with ACD (52% vs. 10%), yet the reherniation rate on imaging irrespective of symptoms was lower with ACD (5% vs. 50%) [3]. Our group previously reported 2-year data from the current trial [10], which arrived at similar conclusions as with the current 3-year data. The presence of VEPC was not associated with patient-reported outcomes (leg pain, back pain, ODI) at 3 years after lumbar discectomy. Further, VEPC growth appears to be self-limiting with larger defects growing at the slowest rates. Based on the 3-year results of this trial, VEPCs occur more commonly with ACD, stabilize over time, and are not associated with adverse clinical sequelae.
Patient-reported outcomes statistically favored the ACD group at 3 years. However, the clinical implications of these findings are unclear since the mean differences between groups ranged from 0.3 to 0.6 MID units, depending on the outcome. A likely explanation for these modest differences is that this was a trial of a device intended to prevent, not treat, herniation recurrence. Since lumbar discectomy results in a durable surgical repair in 70–80% of cases, the benefit of an ACD would be realized only in the subsample of patients in which a reherniation was prevented but would not be anticipated to impact patient-reported outcomes otherwise. Based on the incidence of events and the risk reduction achieved with ACD, the number of patients needed to treat with ACD to prevent one symptomatic reherniation is 7; the number needed to treat to prevent one reoperation is 12.
Important strengths of this study were the multicenter randomized design, large sample size sufficient to detect even rare adverse events, and comprehensive independent review of imaging and adverse events during the trial. There are also several limitations of this study. First, these results are not applicable to all patients undergoing lumbar discectomy, but only the approximately 30% of cases at high risk of reherniation due to a large post-surgical annular defect [13]. The ACD is not intended to be used in patients with smaller defects since treatment with a permanent implant is difficult to justify in this population due to the relatively low risk of reherniation. Second, lack of patient and outcome-assessor blinding to treatment allocation may have biased patient-reported outcomes or the decision to reoperate. Third, while CT imaging with core laboratory reading is a strength of this trial, it may also be perceived as a limitation since the application of CT findings to routine clinical practice is unclear. Finally, longer follow-up is needed in this younger patient population to determine the durability of effect with ACD and to ensure there are no concerning late-onset safety- or device-related complications. While there was no association of VEPC with clinical complications over 3 years among patients who received ACD, this should be confirmed in long-term follow-up.
Conclusion
The addition of a bone-anchored ACD to lumbar discectomy in patients with large post-surgical annular defects reduces the risk of reherniation and reoperation, with a better long-term pain and disability relief over 3-year follow-up compared with lumbar discectomy only. While the ACD was associated with distinct risks such as implantation difficulties, device migration, mesh detachment, and VEPC, the overall risk of complications was comparable between groups.
References
Ahlgren BD, Lui W, Herkowitz HN, Panjabi MM, Guiboux JP (2000) Effect of anular repair on the healing strength of the intervertebral disc: a sheep model. Spine (Phila Pa 1976) 25:2165–2170
Bailey A, Araghi A, Blumenthal S, Huffmon GV, Anular Repair Clinical Study G (2013) Prospective, multicenter, randomized, controlled study of anular repair in lumbar discectomy: two-year follow-up. Spine (Phila Pa 1976) 38:1161–1169. https://doi.org/10.1097/BRS.0b013e31828b2e2f
Barth M, Fontana J, Thome C, Bouma GJ, Schmieder K (2016) Occurrence of discal and non-discal changes after sequestrectomy alone versus sequestrectomy and implantation of an anulus closure device. J Clin Neurosci 34:288–293. https://doi.org/10.1016/j.jocn.2016.09.013
Bouma GJ, Barth M, Ledic D, Vilendecic M (2013) The high-risk discectomy patient: prevention of reherniation in patients with large anular defects using an anular closure device. Eur Spine J 22:1030–1036. https://doi.org/10.1007/s00586-013-2656-1
Bron JL, van der Veen AJ, Helder MN, van Royen BJ, Smit TH, Skeletal Tissue Engineering Group A, Research Institute M (2010) Biomechanical and in vivo evaluation of experimental closure devices of the annulus fibrosus designed for a goat nucleus replacement model. Eur Spine J 19:1347–1355. https://doi.org/10.1007/s00586-010-1384-z
Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25:2940–2952 discussion 2952
Heuer F, Ulrich S, Claes L, Wilke HJ (2008) Biomechanical evaluation of conventional anulus fibrosus closure methods required for nucleus replacement. Laboratory investigation. J Neurosurg Spine 9:307–313. https://doi.org/10.3171/SPI/2008/9/9/307
Kim KT, Lee DH, Cho DC, Sung JK, Kim YB (2015) Preoperative risk factors for recurrent lumbar disk herniation in L5-S1. J Spinal Disord Tech 28:E571–E577. https://doi.org/10.1097/BSD.0000000000000041
Klassen PD, Hes R, Bouma GJ, Eustacchio S, Barth M, Kursumovic A, Jadik S, Heidecke V, Bostelmann R, Thomé C, Vajkoczy P, Köhler HP, Fandino J, Assaker R, van de Kelft E, Fröhlich S, van den Brink W, Perrin J, Wolfs J, Arts M, Martens F (2016) A multicenter, prospective, randomized study protocol to demonstrate the superiority of a bone-anchored prosthesis for anular closure used in conjunction with limited discectomy to limited discectomy alone for primary lumbar disc herniation. Int Clin Trials 3:120–131
Kursumovic A, Kienzler JC, Bouma GJ, Bostelmann R, Heggeness M, Thome C, Miller LE, Barth M, RCTsg AC (2018) Morphology and clinical relevance of vertebral endplate changes following limited lumbar discectomy with or without bone-anchored annular closure. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0000000000002632
Kursumovic A, Rath S (2017) Performance of an annular closure device in a ‘real-world’, heterogeneous, at-risk, lumbar discectomy population. Cureus 9:e1824. https://doi.org/10.7759/cureus.1824
Ledic D, Vukas D, Grahovac G, Barth M, Bouma GJ, Vilendecic M (2015) Effect of anular closure on disk height maintenance and reoperated recurrent herniation following lumbar diskectomy: two-year data. J Neurol Surg A Cent Eur Neurosurg 76:211–218. https://doi.org/10.1055/s-0034-1393930
Miller LE, McGirt MJ, Garfin SR, Bono CM (2018) Association of annular defect width after lumbar discectomy with risk of symptom recurrence and reoperation: systematic review and meta-analysis of comparative studies. Spine (Phila Pa 1976) 43:E308–E315. https://doi.org/10.1097/BRS.0000000000002501
Ostelo RW, de Vet HC (2005) Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol 19:593–607. https://doi.org/10.1016/j.berh.2005.03.003
Parker SL, Grahovac G, Vukas D, Vilendecic M, Ledic D, McGirt MJ, Carragee EJ (2016) Effect of an annular closure device (Barricaid) on same-level recurrent disk herniation and disk height loss after primary lumbar discectomy: two-year results of a multicenter prospective cohort study. Clin Spine Surg 29:454–460. https://doi.org/10.1097/BSD.0b013e3182956ec5
Ran J, Hu Y, Zheng Z, Zhu T, Zheng H, Jing Y, Xu K (2015) Comparison of discectomy versus sequestrectomy in lumbar disc herniation: a meta-analysis of comparative studies. PLoS One 10:e0121816. https://doi.org/10.1371/journal.pone.0121816
Thome C, Klassen PD, Bouma GJ, Kursumovic A, Fandino J, Barth M, Arts M, van den Brink W, Bostelmann R, Hegewald A, Heidecke V, Vajkoczy P, Frohlich S, Wolfs J, Assaker R, Van de Kelft E, Kohler HP, Jadik S, Eustacchio S, Hes R, Martens F, Annular Closure RCTSG (2018) Annular closure in lumbar microdiskectomy for prevention of reherniation: a randomized clinical trial. Spine J. https://doi.org/10.1016/j.spinee.2018.05.003
Ware JE Jr (2000) SF-36 health survey update. Spine (Phila Pa 1976) 25:3130–3139
Acknowledgments
On behalf of the Annular Closure RCT Study Group
Funding
This research was financially supported by Intrinsic Therapeutics, Inc. (Woburn, MA, USA).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
P. Klassen, L. Miller, R. Assaker, and C. Thomé disclose consultancy with Intrinsic Therapeutics. J. C. Kienzler, V. Heidecke, and S. Fröhlich have nothing to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine - Other
Electronic supplementary material
ESM 1
(DOCX 64 kb)
Appendix
Appendix
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kienzler, J.C., Klassen, P.D., Miller, L.E. et al. Three-year results from a randomized trial of lumbar discectomy with annulus fibrosus occlusion in patients at high risk for reherniation. Acta Neurochir 161, 1389–1396 (2019). https://doi.org/10.1007/s00701-019-03948-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-03948-8