Abstract
Background
A hybrid operating room (OR) equipped with robotic angiographic fluoroscopy system has become prevalent in neurosurgery. The level of necessity of the hybrid OR in treating cerebrovascular diseases (CVD) is rarely discussed.
Objective
The authors proposed a scoring and classification system to evaluate the cerebrovascular procedures according to the level of treatment necessity for CVD in a hybrid OR and shared our 5-year experiences.
Methods
From December 2009 to January 2016, the registry of cerebrovascular procedures performed in the hybrid OR was retrieved. A scoring system was used to evaluate the importance of the surgical and interventional components of a cerebrovascular procedure performed in the hybrid OR. The score of either component ranged from 1, 1.5, to 2 (1 = no role, 1.5 = supplementary or informative, 2 = important or therapeutic). The total score of a procedure was by multiplying two individual scores. Levels of necessity were classified into level A (important), level B (beneficial), and level C (replaceable).
Results
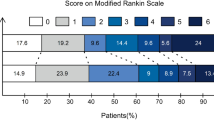
A total of 1027 cerebrovascular procedures were performed during this period: diagnostic angiography in 328, carotid artery stenting in 286, aneurysm coiling in 128, intra-operative DSA in 101, aspiration of ICH under image guidance in 79, intra-arterial thrombolysis/thrombectomy in 51, intracranial angioplasty/stenting in 30, hybrid surgery/serial procedures in 19, and rescue surgery during embolization in 5. According to the scoring system, hybrid surgery and serial procedures scored the highest points (2 × 2). The percentages distributed at each level: levels A (2.3%), B (17.5%), and C (80.2%).
Conclusion
This study conveys a concept of what a hybrid OR equipped with robotic angiographic fluoroscopy system is capable of and its potential. For cerebrovascular diseases, hybrid OR exerts its value via hybrid surgery or avoiding patient transportation in serial procedures (level A), via providing real-time high-quality angiography and image guidance (level B), which constituted about 20% of the cases. The subspecialty of the group using the hybrid OR directly reflects on the number of procedures categorized in each level. In a hybrid OR, innovative treatment strategies for difficult-to-treat CVD can be developed.



Similar content being viewed by others
References
Ashour R, See AP, Dasenbrock HH, Khandelwal P, Patel NJ, Belcher B, Aziz-Sultan MA (2016) Refinement of the hybrid neuroendovascular operating suite: current and future applications. World Neurosurg 91:6–11
Dammann P, Jagersberg M, Kulcsar Z, Radovanovic I, Schaller K, Bijlenga P (2017) Clipping of ruptured intracranial aneurysms in a hybrid room environment—a case-control study. Acta Neurochir 159:1291–1298
Dehdashti AR, Thines L, Da Costa LB, terBrugge KG, Willinsky RA, Wallace MC, Tymianski M (2009) Intraoperative biplanar rotational angiography during neurovascular surgery. Technical note. J Neurosurg 111:188–192
Elijovich L, Higashida RT, Lawton MT, Duckwiler G, Giannotta S, Johnston SC, Cerebral Aneurysm Rerupture After Treatment I (2008) Predictors and outcomes of intraprocedural rupture in patients treated for ruptured intracranial aneurysms: the CARAT study. Stroke 39:1501–1506
Fandino J, Taussky P, Marbacher S, Muroi C, Diepers M, Fathi AR, Remonda L (2013) The concept of a hybrid operating room: applications in cerebrovascular surgery. Acta Neurochir Suppl 115:113–117
Fong YW, Hsu SK, Huang CT, Hsieh CT, Chen MH, Huang JS, Chang CJ, Su IC (2018) Impact of intraoperative 3-dimensional volume-rendering rotational angiography on clip repositioning rates in aneurysmal surgery. World Neurosurg 114:e573–e580
Iihara K, Satow T, Matsushige T, Kataoka H, Nakajima N, Fukuda K, Isozaki M, Maruyama D, Nakae T, Hashimoto N (2013) Hybrid operating room for the treatment of complex neurovascular and brachiocephalic lesions. J Stroke Cerebrovasc Dis 22:e277–e285
Katz JM, Gologorsky Y, Tsiouris AJ, Wells-Roth D, Mascitelli J, Gobin YP, Stieg PE, Riina HA (2006) Is routine intraoperative angiography in the surgical treatment of cerebral aneurysms justified? A consecutive series of 147 aneurysms. Neurosurgery 58:719–727 discussion 719-727
Killory BD, Nakaji P, Gonzales LF, Ponce FA, Wait SD, Spetzler RF (2009) Prospective evaluation of surgical microscope-integrated intraoperative near-infrared indocyanine green angiography during cerebral arteriovenous malformation surgery. Neurosurgery 65:456–462 discussion 462
Kotowski M, Sarrafzadeh A, Schatlo B, Boex C, Narata AP, Pereira VM, Bijlenga P, Schaller K (2013) Intraoperative angiography reloaded: a new hybrid operating theater for combined endovascular and surgical treatment of cerebral arteriovenous malformations: a pilot study on 25 patients. Acta Neurochir 155:2071–2078
Leng LZ, Rubin DG, Patsalides A, Riina HA (2013) Fusion of intraoperative three-dimensional rotational angiography and flat-panel detector computed tomography for cerebrovascular neuronavigation. World Neurosurg 79:504–509
Marbacher S, Mendelowitsch I, Gruter BE, Diepers M, Remonda L, Fandino J (2018) Comparison of 3D intraoperative digital subtraction angiography and intraoperative indocyanine green video angiography during intracranial aneurysm surgery. J Neurosurg:1–8
Matsumae M, Koizumi J, Fukuyama H, Ishizaka H, Mizokami Y, Baba T, Atsumi H, Tsugu A, Oda S, Tanaka Y, Osada T, Imai M, Ishiguro T, Yamamoto M, Tominaga J, Shimoda M, Imai Y (2007) World's first magnetic resonance imaging/x-ray/operating room suite: a significant milestone in the improvement of neurosurgical diagnosis and treatment. J Neurosurg 107:266–273
Matsumae M, Koizumi J, Tsugu A, Inoue G, Nishiyama J, Yoshiyama M, Tominaga J, Atsumi H (2011) Multimodality imaging suite: neo-futuristic diagnostic imaging operating suite marks a significant milestone for innovation in medical technology. Acta Neurochir Suppl 109:215–218
Murayama Y, Saguchi T, Ishibashi T, Ebara M, Takao H, Irie K, Ikeuchi S, Onoue H, Ogawa T, Abe T (2006) Endovascular operating suite: future directions for treating neurovascular disease. J Neurosurg 104:925–930
Murayama Y, Irie K, Saguchi T, Ishibashi T, Ebara M, Nagashima H, Isoshima A, Arakawa H, Takao H, Ohashi H, Joki T, Kato M, Tani S, Ikeuchi S, Abe T (2011) Robotic digital subtraction angiography systems within the hybrid operating room. Neurosurgery 68:1427–1432 discussion 1433
Murayama Y, Arakawa H, Ishibashi T, Kawamura D, Ebara M, Irie K, Takao H, Ikeuchi S, Ogawa T, Kato M, Kajiwara I, Nishimura S, Abe T (2013) Combined surgical and endovascular treatment of complex cerebrovascular diseases in the hybrid operating room. J Neurointerv Surg 5:489–493
Orth RC, Wallace MJ, Kuo MD, Technology Assessment Committee of the Society of Interventional R (2008) C-arm cone-beam CT: general principles and technical considerations for use in interventional radiology. J Vasc Interv Radiol 19:814–820
Pfaff J, Herweh C, Pham M, Schonenberger S, Bosel J, Ringleb PA, Heiland S, Bendszus M, Mohlenbruch M (2016) Mechanical thrombectomy using a combined CT/C-arm X-ray system. J Neurointerv Surg 8:621–625
Schaller K, Kotowski M, Pereira V, Rufenacht D, Bijlenga P (2011) From intraoperative angiography to advanced intraoperative imaging: the Geneva experience. Acta Neurochir Suppl 109:111–115
Shalit MN, Israeli Y, Matz S, Cohen ML (1982) Experience with intraoperative CT scanning in brain tumors. Surg Neurol 17:376–382
Shen SC, Tsuei YS, Chen WH, Shen CC (2015) Hybrid surgery for dural arteriovenous fistula in the neurosurgical hybrid operating suite. J Neurointerv Surg 7:e6
Shih YT, Chen WH, Lee WL, Lee HT, Shen CC, Tsuei YS (2013) Hybrid surgery for symptomatic chronic total occlusion of carotid artery: a technical note. In: Neurosurgery 73:onsE117–123; discussion onsE123
Tang G, Cawley CM, Dion JE, Barrow DL (2002) Intraoperative angiography during aneurysm surgery: a prospective evaluation of efficacy. J Neurosurg 96:993–999
Tang CL, Liao CH, Chen WH, Shen SC, Lee CH, Lee HT, Tsuei YS (2016) Endoscope-assisted transsphenoidal puncture of the cavernous sinus for embolization of carotid-cavernous fistula in a neurosurgical hybrid operating suite. J Neurosurg:1–5
Tronnier VM, Wirtz CR, Knauth M, Lenz G, Pastyr O, Bonsanto MM, Albert FK, Kuth R, Staubert A, Schlegel W, Sartor K, Kunze S (1997) Intraoperative diagnostic and interventional magnetic resonance imaging in neurosurgery. Neurosurgery 40:891–900 discussion 900-892
Tsuei YS, Liao CH, Lee CH, Liang YJ, Chen WH, Yang SF (2018) Intraprocedural arterial perforation during neuroendovascular therapy: preliminary result of a dual-trained endovascular neurosurgeon in the neurosurgical hybrid operating room. J Chin Med Assoc 81:31–36
Wallace MJ, Kuo MD, Glaiberman C, Binkert CA, Orth RC, Soulez G, Technology Assessment Committee of the Society of Interventional R (2009) Three-dimensional C-arm cone-beam CT: applications in the interventional suite. J Vasc Interv Radiol 20:S523–S537
Wang CY, Wei LC, Tsuei YS, Chen WH, Shen YC (2016) Intraorbital arteriovenous fistula of the ophthalmic vein-embolization using the thombosed superior ophthalmic vein approach. Can J Ophthalmol 51:e34–e37
Acknowledgements
We thank Hong-Hsin Lin, Shih-Ruei Huang, and Meng-Ju Lee for their technical assistance in the neurosurgical hybrid operating suite in Taichung Veterans General Hospital.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (IRB TCVGH No. CE17084A) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this retrospective study, formal consents were not required.
Additional information
This article is part of the Topical Collection on Vascular Neurosurgery - Other
Electronic supplementary material
Supplementary Figure 1
Rescue EVD surgery for intra-procedural arterial perforation (IPAP) during coiling. (Level A) (A) CTA showed an unruptured aneurysm at the AComA, about 6 mm in dome size. The aneurysm is indicated by the red arrow in this fig. (B) In deploying the first framing coil, aneurysm rupture occurred. Contrast extravasation was noted (yellow arrow). (C) Arrested intracranial blood flow secondary to increased intracranial pressure was detected in the following DSA. (D) Intra-operative photo showed immediate conversion to rescue EVD surgery without moving the patient in the hybrid OR. (E) After EVD insertion, intracranial blood flow restored and allowed completion of aneurysm coiling until there was no further extravasation (F) Final DSA showed adequate aneurysm coiling and patent flow in bilateral anterior cerebral arteries. The blue arrow indicated the ventricular catheter. (PNG 2843 kb)
Supplementary Figure 2
Dyna-CT guided aspiration of ICH in the hybrid OR. (Level B) (A) Pre-operative non-contrast brain CT revealed a left putaminal hemorrhage, about 35 mL. (B) A frontal burr hole was made at the left Kocher’s point, and the ICH location was re-confirmed by Dyna-CT scan. In the workstation, the trajectory of the catheter insertion was a straight line connecting the burr hole and the center of the ICH. The depth of insertion was also calculated. (C) The central region of the ICH was chosen as a target, indicated by the red spot. (D) The direction of fluoroscopic projections of the robotic arm was parallel to the pre-determined trajectory. Under fluoroscopic guidance, the stylet-attached catheter was advanced and projected as a point to confirm correct trajectory. (E) Gentle aspiration of the ICH was performed through the catheter. (F) Intra-operative Dyna-CT showed the ICH volume was immediately reduced to 8 ml (23%). CT scan on post-operative day 3 showed the ICH volume decreased to 1 ml (3%) after direct infusion of urokinase through the catheter. (PNG 2409 kb)
Supplementary Figure 3
A left MCA complex aneurysm treated in the hybrid OR. (Level B) (A and B) CT angiography showed a left MCA complex aneurysm with ICA/ACA junction involvement and distal M1 dilatation. (C) Intra-operative 3D DSA simulated the actual operative view. (D) Intra-operative 3D DSA was performed by a robotic C-arm rotation for data acquisition (E) Post-operative 3D DSA confirmed adequate clip position. (F) Pre- and intra-operative DSA showed no obvious differences in blood flow velocity to the distal MCA territory after clipping surgery. (PNG 3619 kb)
Supplementary Figure 4
A 4-cm AVM at right motor and sensory cortex with hemorrhage treated in the hybrid OR. (Level B) (A) Brain CT scan revealed an unusual location of hemorrhage at eloquent region. (B) 3D CT angiography revealed a MCA-supplied AVM with two large draining veins to the superior sagittal sinus. (C, D, and E) Illustrative fluoroscopic roadmap views assisted in AVM localization before skin incision and before craniotomy. (F) DSA showed multiple MCA branches supplied the AVM. (G) After temporary clipping of two main feeding arteries (red arrows), intra-operative DSA roadmap view assisted in confirming additional feeder (indicated by Rhoton dissector/blue arrow) to the nidus. (H) Intra-operative DSA showed no residual AVM after the excision. (PNG 2172 kb)
Rights and permissions
About this article
Cite this article
Liao, CH., Chen, WH., Lee, CH. et al. Treating cerebrovascular diseases in hybrid operating room equipped with a robotic angiographic fluoroscopy system: level of necessity and 5-year experiences. Acta Neurochir 161, 611–619 (2019). https://doi.org/10.1007/s00701-018-3769-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3769-4