Abstract
Background
The extent of resection (EOR) is a crucial outcome parameter in transsphenoidal pituitary surgery (TSS), and is linked to endocrinological outcome, postoperative morbidity, and mortality. We aimed to build a robust, quantitative, and easily reproducible imaging score able to predict EOR in TSS.
Methods
The ratio (R) between the maximum horizontal adenoma diameter and intercarotid distance at the horizontal C4 segment was used to stratify our patient series in four classes: class I R ≤ 0.75, class II 0.75 < R ≤ 1.25, and class III R ≥ 1.25. Class IV included adenomas which completely encased the internal carotid artery. The resulting score was internally validated for robustness.
Results
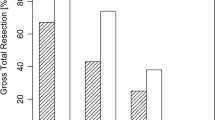
One hundred sixteen patients were included in the study, of which 96 (83%) for derivation and 20 (17%) for validation. EOR showed significant differences between grades (grade I, 100%; II, 97.9%; III, 94.2%; IV, 87.2%; all P < 0.05). The same applied to residual volume (RV) (grade I, 0 cm3; II, 0.08 cm3; III, 1.11 cm3; IV, 1.63 cm3; all P < 0.05). Differences in gross total resection (GTR) were statistically significant among classes I, II, and III (P < 0.05). The incidence of residual adenoma in the cavernous sinus increased also constantly from grade I up to grade IV although a significant difference was only found between grades III and II (P = 0.004). The score performed equally well in the validation cohort. Inter-observer agreement was high, with intraclass correlation coefficients > 0.89 for measurement of both the horizontal tumor diameter and the ICD among two independent raters (P < 0.001).
Conclusions
The proposed score is a simple and reproducible tool which reliably predicts surgical outcome including EOR, RV, and GTR of pituitary adenoma patients undergoing TSS.


Similar content being viewed by others
References
Banu MA, Rathman A, Patel KS, Souweidane MM, Anand VK, Greenfield JP, Schwartz TH (2014) Corridor-based endonasal endoscopic surgery for pediatric skull base pathology with detailed radioanatomic measurements. Neurosurgery 10(Suppl 2):273–293; discussion 293. https://doi.org/10.1227/NEU.0000000000000252
Bouthillier A, van Loveren HR, Keller JT (1996) Segments of the internal carotid artery: a new classification. Neurosurgery 38:425–432 discussion 432-433
Cebula H, Kurbanov A, Zimmer LA, Poczos P, Leach JL, De Battista JC, Froelich S, Theodosopoulos PV, Keller JT (2014) Endoscopic, endonasal variability in the anatomy of the internal carotid artery. World Neurosurg 82:e759–e764. https://doi.org/10.1016/j.wneu.2014.09.021
Conrad J, Ayyad A, Wüster C, Omran W, Weber MM, Konerding MA, Müller-Forell W, Giese A, Oertel J (2016) Binostril versus mononostril approaches in endoscopic transsphenoidal pituitary surgery: clinical evaluation and cadaver study. J Neurosurg 125:334–345. https://doi.org/10.3171/2015.6.JNS142637
Dallapiazza RF, Grober Y, Starke RM, Laws ER, Jane JA (2015) Long-term results of endonasal endoscopic transsphenoidal resection of nonfunctioning pituitary macroadenomas. Neurosurgery 76:42–52; discussion 52-53. https://doi.org/10.1227/NEU.0000000000000563
Dehdashti AR, Ganna A, Karabatsou K, Gentili F (2008) Pure endoscopic endonasal approach for pituitary adenomas: early surgical results in 200 patients and comparison with previous microsurgical series. Neurosurgery 62:1006–1015; discussion 1015-1017. https://doi.org/10.1227/01.neu.0000325862.83961.12
Dhandapani S, Singh H, Negm HM, Cohen S, Anand VK, Schwartz TH (2016) Cavernous sinus invasion in pituitary adenomas: systematic review and pooled data meta-analysis of radiologic criteria and comparison of endoscopic and microscopic surgery. World Neurosurg 96:36–46. https://doi.org/10.1016/j.wneu.2016.08.088
Elhadi AM, Hardesty DA, Zaidi HA, Kalani MYS, Nakaji P, White WL, Preul MC, Little AS (2015) Evaluation of surgical freedom for microscopic and endoscopic transsphenoidal approaches to the sella. Neurosurgery 11(Suppl 2):69–78; discussion 78-79. https://doi.org/10.1227/NEU.0000000000000601
Hardy J, Vezina JL (1976) Transsphenoidal neurosurgery of intracranial neoplasm. Adv Neurol 15:261–273
Hardy J, Wigser SM (1965) Trans-sphenoidal surgery of pituitary fossa tumors with televised radiofluoroscopic control. J Neurosurg 23:612–619. https://doi.org/10.3171/jns.1965.23.6.0612
Hofstetter CP, Nanaszko MJ, Mubita LL, Tsiouris J, Anand VK, Schwartz TH (2012) Volumetric classification of pituitary macroadenomas predicts outcome and morbidity following endoscopic endonasal transsphenoidal surgery. Pituitary 15:450–463. https://doi.org/10.1007/s11102-011-0350-z
Juraschka K, Khan OH, Godoy BL, Monsalves E, Kilian A, Krischek B, Ghare A, Vescan A, Gentili F, Zadeh G (2014) Endoscopic endonasal transsphenoidal approach to large and giant pituitary adenomas: institutional experience and predictors of extent of resection. J Neurosurg 121:75–83. https://doi.org/10.3171/2014.3.JNS131679
Kanter AS, Dumont AS, Asthagiri AR, Oskouian RJ, Jane JA, Laws ER (2005) The transsphenoidal approach. A historical perspective. Neurosurg Focus 18:e6
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33:610–617 discussion 617-618
Meij BP, Lopes M-BS, Ellegala DB, Alden TD, Laws ER (2002) The long-term significance of microscopic dural invasion in 354 patients with pituitary adenomas treated with transsphenoidal surgery. J Neurosurg 96:195–208. https://doi.org/10.3171/jns.2002.96.2.0195
Micko ASG, Wöhrer A, Wolfsberger S, Knosp E (2015) Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J Neurosurg 122:803–811. https://doi.org/10.3171/2014.12.JNS141083
Mooney MA, Hardesty DA, Sheehy JP, Bird R, Chapple K, White WL, Little AS (2016) Interrater and intrarater reliability of the Knosp scale for pituitary adenoma grading. J Neurosurg 126:1714–1719. https://doi.org/10.3171/2016.3.JNS153044
Negm HM, Al-Mahfoudh R, Pai M, Singh H, Cohen S, Dhandapani S, Anand VK, Schwartz TH (2016) Reoperative endoscopic endonasal surgery for residual or recurrent pituitary adenomas. J Neurosurg:1–12. https://doi.org/10.3171/2016.8.JNS152709
Nishioka H, Hara T, Nagata Y, Fukuhara N, Yamaguchi-Okada M, Yamada S (2017) Inherent tumor characteristics that limit effective and safe resection of giant nonfunctioning pituitary adenomas. World Neurosurg. https://doi.org/10.1016/j.wneu.2017.07.043
Perondi GE, Isolan GR, de Aguiar PHP, Stefani MA, Falcetta EF (2013) Endoscopic anatomy of sellar region. Pituitary 16:251–259. https://doi.org/10.1007/s11102-012-0413-9
Serra C, Burkhardt J-K, Esposito G, Bozinov O, Pangalu A, Valavanis A, Holzmann D, Schmid C, Regli L (2016) Pituitary surgery and volumetric assessment of extent of resection: a paradigm shift in the use of intraoperative magnetic resonance imaging. Neurosurg Focus 40:E17. https://doi.org/10.3171/2015.12.FOCUS15564
Serra C, Maldaner N, Muscas G, Staartjes V, Pangalu A, Holzmann D, Soyka M, Schmid C, Regli L (2017) The changing sella: internal carotid artery shift during transsphenoidal pituitary surgery. Pituitary:1–7. https://doi.org/10.1007/s11102-017-0830-x
Sughrue ME, Chang EF, Gabriel RA, Aghi MK, Blevins LS (2011) Excess mortality for patients with residual disease following resection of pituitary adenomas. Pituitary 14:276–283. https://doi.org/10.1007/s11102-011-0308-1
Sylvester PT, Evans JA, Zipfel GJ, Chole RA, Uppaluri R, Haughey BH, Getz AE, Silverstein J, Rich KM, Kim AH, Dacey RG, Chicoine MR (2015) Combined high-field intraoperative magnetic resonance imaging and endoscopy increase extent of resection and progression-free survival for pituitary adenomas. Pituitary 18:72–85. https://doi.org/10.1007/s11102-014-0560-2
Taniguchi M, Hosoda K, Akutsu N, Takahashi Y, Kohmura E (2015) Endoscopic endonasal transsellar approach for laterally extended pituitary adenomas: volumetric analysis of cavernous sinus invasion. Pituitary 18:518–524. https://doi.org/10.1007/s11102-014-0604-7
Woodworth GF, Patel KS, Shin B, Burkhardt J-K, Tsiouris AJ, McCoul ED, Anand VK, Schwartz TH (2014) Surgical outcomes using a medial-to-lateral endonasal endoscopic approach to pituitary adenomas invading the cavernous sinus. J Neurosurg 120:1086–1094. https://doi.org/10.3171/2014.1.JNS131228
Acknowledgements
We thank Jorn Fierstra, MD, PhD, and Bas van Niftrik, MD, for their independent measurements used for the assessment of interrater agreement, and Nicola Podda for his graphical work (Fig. 2).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Cantonal Ethics Committee Zürich, KEK St-V-Nr 2015-0142) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
This article is part of the Topical Collection on Pituitaries
Electronic supplementary material
Supplementary Table 1
Surgical results at 3 months follow up. Values are given separately for both the derivation and validation cohort. IQR, interquartile range; SD, standard deviation; CSS, cavernous sinus space. (DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Serra, C., Staartjes, V.E., Maldaner, N. et al. Predicting extent of resection in transsphenoidal surgery for pituitary adenoma. Acta Neurochir 160, 2255–2262 (2018). https://doi.org/10.1007/s00701-018-3690-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3690-x