Abstract
Background
Our aim was to describe the pattern of ventriculostomy-related infection (VRI) development using a dynamic approach.
Study design
Retrospective longitudinal study.
Methods
We analyzed the files of 449 neurosurgical patients who underwent placement of external ventricular drain (EVD). During the study period, CSF sampling was performed on a daily base setting. VRI was defined as a positive CSF culture resulting in antibiotic treatment. For VRI patients, we arbitrary defined day 0 (D0) as the day antibiotic treatment was started. In these patients, we compared dynamic changes in clinical and biological parameters at four pre-determined time points: (D-4, D-3, D-2, D-1) with those of D0. For all CSF-positive cultures, we compared CSF biochemical markers’ evolution pattern between VRI patients and the others, considered as a control cohort.
Results
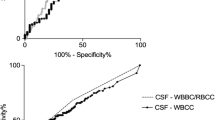
Thirty-two suffered from VRI. Peripheral white blood cell count did not differ between D-4-D0. Median body temperature, CSF cell count, median Glasgow Coma Scale, CSF protein, and glucose concentrations were significantly different between D-4, D-3, D-2, and D0. At D0, 100 % of CSF samples yielded organisms in culture. The physician caring for the patient decided to treat VRI based upon positive CSF culture in only 28 % (9/32) of cases. In the control cohort, CSF markers’ profile trends to normalize, while it worsens in the VRI patients.
Conclusions
We showed that clinical symptoms and biological abnormalities of VRI evolved over time. Our data suggest that VRI decision to treat relies upon a bundle of evidence, including dynamic changes in CSF laboratory exams combined with microbiological analysis.





Similar content being viewed by others

References
Aronin SI, Peduzzi P, Quagliarello VJ (1998) Community-acquired bacterial meningitis: risk stratification for adverse clinical outcome and effect of antibiotic timing. Ann Intern Med 129(11):862–869
Berger C, Schwarz S, Schaebitz WR, Aschoff A, Schwab S (2002) Serum procalcitonin in cerebral ventriculitis. Crit Care Med 30(8):1778–1781
Bogdahn U, Lau W, Hassel W, Gunreben G, Mertens HG, Brawanski A (1992) Continuous-pressure controlled, external ventricular drainage for treatment of acute hydrocephalus—evaluation of risk factors. Neurosurgery 31(5):898–903, discussion 903–904
Carbonnelle E (2009) Laboratory diagnosis of bacterial meningitis: usefulness of various tests for the determination of the etiological agent. Médecine Mal Infect 39(7–8):581–605
Clark WC, Muhlbauer MS, Lowrey R, Hartman M, Ray MW, Watridge CB (1989) Complications of intracranial pressure monitoring in trauma patients. Neurosurgery 25(1):20–24
Hader WJ, Steinbok P (2000) The value of routine cultures of the cerebrospinal fluid in patients with external ventricular drains. Neurosurgery 46(5):1149–1153, discussion 1153–1155
Hoefnagel D, Dammers R, Ter Laak-Poort MP, Avezaat CJJ (2008) Risk factors for infections related to external ventricular drainage. Acta Neurochir (Wien) 150(3):209–214, discussion 214
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36(5):309–332
Khatib R, Riederer KM, Clark JA, Khatib S, Briski LE, Wilson FM (1995) Coagulase-negative staphylococci in multiple blood cultures: strain relatedness and determinants of same-strain bacteremia. J Clin Microbiol 33(4):816–820
Korinek A-M, Reina M, Boch AL, Rivera AO, De Bels D, Puybasset L (2005) Prevention of external ventricular drain-related ventriculitis. Acta Neurochir (Wien) 147(1):39–45, discussion 45–46
Leverstein-van Hall MA, Hopmans TEM, van der Sprenkel JWB, Blok HEM, van der Mark WAMA, Hanlo PW, Bonten MJM (2010) A bundle approach to reduce the incidence of external ventricular and lumbar drain-related infections. J Neurosurg 112(2):345–353
Lozier AP, Sciacca RR, Romagnoli MF, Connolly ES Jr (2002) Ventriculostomy-related infections: a critical review of the literature. Neurosurgery 51(1):170–181, discussion 181–182
Lyke KE, Obasanjo OO, Williams MA, O’Brien M, Chotani R, Perl TM (2001) Ventriculitis complicating use of intraventricular catheters in adult neurosurgical patients. Clin Infect Dis Off Publ Infect Dis Soc Am 33(12):2028–2033
Mayhall CG, Archer NH, Lamb VA, Spadora AC, Baggett JW, Ward JD, Narayan RK (1984) Ventriculostomy-related infections. A prospective epidemiologic study. N Engl J Med 310(9):553–559
Meredith FT, Phillips HK, Reller LB (1997) Clinical utility of broth cultures of cerebrospinal fluid from patients at risk for shunt infections. J Clin Microbiol 35(12):3109–3111
Muttaiyah S, Ritchie S, Upton A, Roberts S (2008) Clinical parameters do not predict infection in patients with external ventricular drains: a retrospective observational study of daily cerebrospinal fluid analysis. J Med Microbiol 57(Pt 2):207–209
Paramore CG, Turner DA (1994) Relative risks of ventriculostomy infection and morbidity. Acta Neurochir (Wien) 127(1–2):79–84
Pfausler B, Beer R, Engelhardt K, Kemmler G, Mohsenipour I, Schmutzhard E (2004) Cell index--a new parameter for the early diagnosis of ventriculostomy (external ventricular drainage)-related ventriculitis in patients with intraventricular hemorrhage? Acta Neurochir (Wien) 146(5):477–481
Pfisterer W, Mühlbauer M, Czech T, Reinprecht A (2003) Early diagnosis of external ventricular drainage infection: results of a prospective study. J Neurol Neurosurg Psychiatry 74(7):929–932
Schade RP, Schinkel J, Roelandse FWC, Geskus RB, Visser LG, van Dijk JMC, Van Dijk MC, Voormolen JHC, Van Pelt H, Kuijper EJ (2006) Lack of value of routine analysis of cerebrospinal fluid for prediction and diagnosis of external drainage-related bacterial meningitis. J Neurosurg 104(1):101–108
Scheithauer S, Bürgel U, Ryang Y-M, Haase G, Schiefer J, Koch S, Häfner H, Lemmen S (2009) Prospective surveillance of drain associated meningitis/ventriculitis in a neurosurgery and neurological intensive care unit. J Neurol Neurosurg Psychiatry 80(12):1381–1385
Schlenk F, Frieler K, Nagel A, Vajkoczy P, Sarrafzadeh AS (2009) Cerebral microdialysis for detection of bacterial meningitis in aneurysmal subarachnoid hemorrhage patients: a cohort study. Crit Care Lond Engl 13(1):R2
Stenager E, Gerner-Smidt P, Kock-Jensen C (1986) Ventriculostomy-related infections—an epidemiological study. Acta Neurochir (Wien) 83(1–2):20–23
Walti LN, Conen A, Coward J, Jost GF, Trampuz A (2013) Characteristics of infections associated with external ventricular drains of cerebrospinal fluid. J Infect 66(5):424–431
Wyler AR, Kelly WA (1972) Use of antibiotics with external ventriculostomies. J Neurosurg 37(2):185–187
Zabramski JM, Whiting D, Darouiche RO, Horner TG, Olson J, Robertson C, Hamilton AJ (2003) Efficacy of antimicrobial-impregnated external ventricular drain catheters: a prospective, randomized, controlled trial. J Neurosurg 98(4):725–730
Funding
Support was provided solely from institutional and/or departmental sources.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The diagnosis of a ventriculostomy-related CSF infection is a common problem in neurosurgical patients. The neurological impact of the initial pathology, the presence of ventricular blood, and comorbidities in ICU patients may lead to a regrettable delay in diagnosis and treatment. The authors provide a service by retrospectively analyzing a group of patients with ventriculostomies several days prior to the diagnosis of CSF infection. Daily samples from the ventricular drainage system combined with neurological status and body temperature allowed the initiation of antibiotic therapy prior to the positive results from microbiological cultures in a significant number of patients. These parameters were also able to exclude from treatment cases in which CSF samples were only contaminated. While experienced clinicians have already internalized the obvious parameters of significance from this study, it is nice to have it presented to us statistically in a large group of patients with an appropriate comparison group.
Zvi Harry Rappaport
Petah Tiqva, Israel
Rights and permissions
About this article
Cite this article
Mounier, R., Lobo, D., Cook, F. et al. Clinical, biological, and microbiological pattern associated with ventriculostomy-related infection: a retrospective longitudinal study. Acta Neurochir 157, 2209–2217 (2015). https://doi.org/10.1007/s00701-015-2574-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2574-6