Abstract
Background
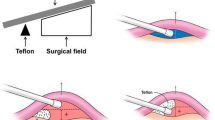
Hemifacial spasm (HFS) is caused by tortuous offending vessels near the facial nerve root exit zone. However, the definitive mechanism of offending vessel formation remains unclear. We hypothesized that vascular angulation and tortuosity, probably caused by uneven vertebral artery blood flow, result in vascular compression of the facial nerve root exit zone.
Methods
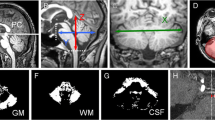
The authors observed two anatomical characteristics of the vertebrobasilar arterial system in 120 subjects in the surgical group and 188 controls. The presence of the dominant vertebral artery (DVA) and laterality of the vertebrobasilar junction (VBJ) were observed. We also analyzed the morphological characteristics of the surgical group showing the presence of DVA. The morphological characteristics were classified into three types: type I had the VBJ and DVA on the same side, type II had the VBJ within 2 mm of the midline, and type III had the VBJ opposite the DVA.
Result
The DVA was more prevalent in the surgical group than in the control group (71 % versus 54 %, P < 0.05). The surgical group patients with HFS on the left were more likely to have a DVA on the left (P < 0.05) and with HFS on the right were more likely to have a DVA on the right (P < 0.01) compared with controls. The direction of the VBJ was more common on the same side as the DVA, which corresponds with the laterality of the HFS. In the surgical group with the DVA and HFS on the same side, type I was predominant, but in the surgical group with a contralateral DVA and HFS, type III was predominant.
Conclusion
The presence of a DVA and shifting of the VBJ on the same side plays a role in the angulation and tortuosity of vessels in the perivertebrobasilar junction, resulting in neurovascular compression of the facial nerve root exit zone and thereby causing HFS.



Similar content being viewed by others
References
Barker FG, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD (1995) Microvascular decompression for hemifacial spasm. J Neurosurg 82:201–210
Choi HJ, Lee SH, Choi SK, Rhee BA (2012) Hemifacial spasm developed after contralateral vertebral artery ligation. J Korean Neurosurg Soc 51:59–61
Chuang YM, Huang YC, Hu HH, Yang CY (2006) Toward a further elucidation: role of vertebral artery hypoplasia in acute ischemic stroke. Eur Neurol 55:193–197
Cloud GC, Markus HS (2003) Diagnosis and management of vertebral artery stenosis. QJM: Mon J AssocPhys 96:27–54
Guan HX, Zhu J, Zhong J (2011) Correlation between idiopathic hemifacial spasm and the MRI characteristics of the vertebral artery. J Clin Neurosci 18:528–530
Hong JM, Chung CS, Bang OY, Yong SW, Joo IS, Huh K (2009) Vertebral artery dominance contributes to basilar artery curvature and peri-vertebrobasilar junctional infarcts. J Neurol Neurosurg Psychiatry 80:1087–1092
Hyun SJ, Kong DS, Park K (2010) Microvascular decompression for treating hemifacial spasm: lessons learned from a prospective study of 1,174 operations. Neurosurg Rev 33:325–334, discussion 334
Jeng JS, Yip PK (2004) Evaluation of vertebral artery hypoplasia and asymmetry by color-coded duplex ultrasonography. Ultrasound Med Biol 30:605–609
Nagahiro S, Takada A, Matsukado Y, Ushio Y (1991) Microvascular decompression for hemifacial spasm. Patterns of vascular compression in unsuccessfully operated patients. J Neurosurg 75:388–392
Nagashima H, Orz Y, Okudera H, Kobayashi S, Ichinose Y (2001) Remission of hemifacial spasm after proximal occlusion of vertebrobasilar dissecting aneurysm with coils: case report. J Clin Neurosci: Off J Neurosurg Soc Australas 8:43–45
Naraghi R, Hastreiter P, Tomandl B, Bonk A, Huk W, Fahlbusch R (2004) Three-dimensional visualization of neurovascular relationships in the posterior fossa: technique and clinical application. J Neurosurg 100:1025–1035
Ogiwara M, Shimizu T (2004) Surface rendered three-dimensional MR imaging for the evaluation of trigeminal neuralgia and hemifacial spasm. J Clin Neurosci 11:840–844
Park JH, Kim JM, Roh JK (2007) Hypoplastic vertebral artery: frequency and associations with ischaemic stroke territory. J Neurol Neurosurg Psychiatry 78:954–958
Sato K, Ezura M, Takahashi A, Yoshimoto T (2001) Fusiform aneurysm of the vertebral artery presenting hemifacial spasm treated by intravascular embolization: case report. Surg Neurol 56:52–55
Wake-Buck AK, Gatenby JC, Gore JC (2012) Hemodynamic characteristics of the vertebrobasilar system analyzed using MRI-based models. PLoS One 7:e51346
Zhang DP, Zhang SL, Zhang HT, Zhang SJ (2012) Vertebral artery dominance, brainstem auditory evoked potential, and vertigo of vascular origin. Neurol Res 34:498–503
Acknowledgments
All authors certify that we have no financial interest in the subject matter discussed in this article.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The authors of this interesting article analyze the vertebrobasilar arterial system in 120 patients operated on for hemifacial spasm (HFS) and compare the anatomical findings with a control group of 188 patients. Two variables were analyzed in particular, the dominant vertebral artery (DVA) and the laterality of the vertebrobasilar junction (VBJ). Moreover, they propose a classification of the the DVA-VBJ into type I (same side), type II (2 mm off the midline), and type III (opposite side). The authors postulate that an even blood flow within the vertebrobasilar system leads to significant tortuosity and consequent neurovascular conflict. This is not a completely novel hypothesis; previous authors have demonstrated higher flow rates with a duplex on the side of the neurovascular conflict in patients with HFS. Angiographic analysis of the posterior fossa circulation in patients with HFS has demonstrated significant trunk anomalies; moreover, the anomalies of the main trunk can lead to abnormaly located perforators, which in turn can make mobilization of the vessel difficult. Surgical strategies in these difficult cases can be different from the standard microvascular decompression, and at times sling trasposition at the level of the vertebrobasilar system may be indicated. Still, the reported outcome is quite good with control of the spasm in nearly 80 % of cases. The authors should be congratulated for their effort to anatomically classify vertebrobasilar system abnormalities associated with HFS.
Jibril Osman Farah
Liverpool, UK
Rights and permissions
About this article
Cite this article
Park, JS., Koh, EJ., Choi, HY. et al. Characteristic anatomical conformation of the vertebral artery causing vascular compression against the root exit zone of the facial nerve in patients with hemifacial spasm. Acta Neurochir 157, 449–454 (2015). https://doi.org/10.1007/s00701-014-2338-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2338-8