Abstract
Background
Cerebrospinal fluid (CSF) shunt-associated infection is one of the most frequent complications of CSF shunt surgery. We evaluated our institutional guideline for the treatment of shunt-associated infections.
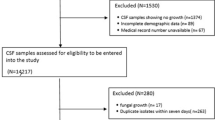
Methods
We retrospectively analysed all 92 episodes of shunt-associated infections in 78 patients treated in our institution from 2002 to 2008. All patients underwent urgent surgery, i.e. removal of the complete shunt hardware or externalisation of the distal tubing in cases with an infection restricted to the distal shunt (10 %), placement of an external ventricular drainage as necessary and antibiotic therapy. Standard empirical first-line antibiotic treatment consisted of a combination of flucloxacillin and cefuroxime.
Results
We observed 38 % early (<1 month after shunt surgery) and 20 % late infections (> 1 year after shunt placement). Coagulase-negative staphylococci (CoNS) were isolated in 38 %. In 38 % no pathogens could be isolated. Of cases with a first shunt infection, 58 % were initially treated with flucloxacillin/cefuroxime. Only 53 % of all infections were treated successfully with the first course of antibiotics. Only 51 % of bacterial isolates were sensitive to empirical first-line antibiotics. Twenty percent of infections caused by sensitive bacterial isolates nevertheless required second-line antibiotic therapy.
Conclusions
Urgent surgery for shunt removal and antibiotic therapy will usually cure a shunt-associated infection. The choice of antibiotics should reflect the spectrum of pathogens seen at one’s institution, paying particular attention to the role of CoNS isolates, and in vitro sensitivity testing results.

Similar content being viewed by others
References
Albright AL, Haines SJ, Taylor FH (1988) Function of parietal and frontal shunts in childhood hydrocephalus. J Neurosurg 69:883–886
Baird C, O’Connor D, Pittman T (1999) Late shunt infections. Pediatr Neurosurg 31:269–273
Borgbjerg BM, Gjerris F, Albeck MJ, Borgesen SE (1995) Risk of infection after cerebrospinal fluid shunt: an analysis of 884 first-time shunts. Acta Neurochir (Wien) 136:1–7
Brook I (2002) Meningitis and shunt infection caused by anaerobic bacteria in children. Pediatr Neurol 26:99–105
Brown EM, Edwards RJ, Pople IK (2006) Conservative management of patients with cerebrospinal fluid shunt infections. Neurosurgery 58:657–665, discussion 657–665
Conen A, Walti LN, Merlo A, Fluckiger U, Battegay M, Trampuz A (2008) Characteristics and treatment outcome of cerebrospinal fluid shunt-associated infections in adults: a retrospective analysis over an 11-year period. Clin Infect Dis 47:73–82
Dougherty SH (1988) Pathobiology of infection in prosthetic devices. Rev Infect Dis 10:1102–1117
Fey PD (2010) Modality of bacterial growth presents unique targets: how do we treat biofilm-mediated infections? Curr Opin Microbiol 13:610–615
Forouzesh A, Moise PA, Sakoulas G (2009) Vancomycin ototoxicity: a reevaluation in an era of increasing doses. Antimicrob Agents Chemother 53:483–486
Gandelman G, Frishman WH, Wiese C, Green-Gastwirth V, Hong S, Aronow WS, Horowitz HW (2007) Intravascular device infections: epidemiology, diagnosis, and management. Cardiol Rev 15:13–23
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16:128–140
James HE, Walsh JW, Wilson HD, Connor JD, Bean JR, Tibbs PA (1980) Prospective randomized study of therapy in cerebrospinal fluid shunt infection. Neurosurgery 7:459–463
James HE, Bejar R, Gluck L, Coen R, Merritt A, Mannino F, Bromberger P, Saunders B, Schneider H (1984) Ventriculoperitoneal shunts in high risk newborns weighing under 2000 grams: a clinical report. Neurosurgery 15:198–202
Kanev PM, Sheehan JM (2003) Reflections on shunt infection. Pediatr Neurosurg 39:285–290
Key CB, Rothrock SG, Falk JL (1995) Cerebrospinal fluid shunt complications: an emergency medicine perspective. Pediatr Emerg Care 11:265–273
Kontny U, Hofling B, Gutjahr P, Voth D, Schwarz M, Schmitt HJ (1993) CSF shunt infections in children. Infection 21:89–92
Kulkarni AV, Drake JM, Lamberti-Pasculli M (2001) Cerebrospinal fluid shunt infection: a prospective study of risk factors. J Neurosurg 94:195–201
Leib SL, Boscacci R, Gratzl O, Zimmerli W (1999) Predictive value of cerebrospinal fluid (CSF) lactate level versus CSF/blood glucose ratio for the diagnosis of bacterial meningitis following neurosurgery. Clin Infect Dis 29:69–74
Mancao M, Miller C, Cochrane B, Hoff C, Sauter K, Weber E (1998) Cerebrospinal fluid shunt infections in infants and children in Mobile, Alabama. Acta Paediatr 87:667–670
McCann MT, Gilmore BF, Gorman SP (2008) Staphylococcus epidermidis device-related infections: pathogenesis and clinical management. J Pharm Pharmacol 60:1551–1571
McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ (2003) Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis 36:858–862
McLaurin RL, Frame PT (1987) Treatment of infections of cerebrospinal fluid shunts. Rev Infect Dis 9:595–603
Odio C, McCracken GH Jr, Nelson JD (1984) CSF shunt infections in pediatrics. A seven-year experience. Am J Dis Child 138:1103–1108
Oprica C, Nord CE (2005) European surveillance study on the antibiotic susceptibility of Propionibacterium acnes. Clin Microbiol Infect 11:204–213
Pritchard L, Baker C, Leggett J, Sehdev P, Brown A, Bayley KB (2010) Increasing vancomycin serum trough concentrations and incidence of nephrotoxicity. Am J Med 123:1143–1149
Prusseit J, Simon M, von der Brelie C, Heep A, Molitor E, Volz S, Simon A (2009) Epidemiology, prevention and management of ventriculoperitoneal shunt infections in children. Pediatr Neurosurg 45:325–336
Rowin ME, Patel VV, Christenson JC (2003) Pediatric intensive care unit nosocomial infections: epidemiology, sources and solutions. Crit Care Clin 19:473–487
Sabatier C, Ferrer R, Valles J (2009) Treatment strategies for central venous catheter infections. Expert Opin Pharmacother 10:2231–2243
Schuhmann MU, Ostrowski KR, Draper EJ, Chu JW, Ham SD, Sood S, McAllister JP (2005) The value of C-reactive protein in the management of shunt infections. J Neurosurg 103:223–230
Shapiro S, Boaz J, Kleiman M, Kalsbeck J, Mealey J (1988) Origin of organisms infecting ventricular shunts. Neurosurgery 22:868–872
Spanu G, Karussos G, Adinolfi D, Bonfanti N (1986) An analysis of cerebrospinal fluid shunt infections in adults. A clinical experience of twelve years. Acta Neurochir (Wien) 80:79–82
Thompson TP, Albright AL (1998) Propionibacterium [correction of Proprionibacterium] acnes infections of cerebrospinal fluid shunts. Childs Nerv Syst 14:378–380
Younger JJ, Christensen GD, Bartley DL, Simmons JC, Barrett FF (1987) Coagulase-negative staphylococci isolated from cerebrospinal fluid shunts: importance of slime production, species identification, and shunt removal to clinical outcome. J Infect Dis 156:548–554
Zimmerli W, Lew PD, Waldvogel FA (1984) Pathogenesis of foreign body infection. Evidence for a local granulocyte defect. J Clin Invest 73:1191–1200
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
von der Brelie, C., Simon, A., Gröner, A. et al. Evaluation of an institutional guideline for the treatment of cerebrospinal fluid shunt-associated infections. Acta Neurochir 154, 1691–1697 (2012). https://doi.org/10.1007/s00701-012-1329-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1329-x