Abstract
Background
Elbow flexion and shoulder abduction are the primary goals in brachial plexus surgery; however, reinnervation of the triceps is also an objective to be considered, as restoration of elbow extension improves the stabilization of the elbow and can provide a more powerful grasp. This study aims to demonstrate the author’s experience with restoration of elbow extension function in cases of brachial plexus surgery in adults.
Methods
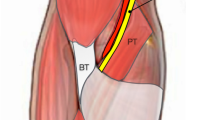
Records of 25 patients sustaining traumatic brachial plexus injuries who were treated surgically with reinnervation of the triceps were reviewed. Nine techniques were employed, including posterior cord reconstruction and nerve transfers using donors such as the ipsilateral C7 root, phrenic nerve, medial pectoral nerve, intercostal nerves, the spinal accessory nerve, and a motor fascicle of the ulnar nerve. The targeted structure was the radial nerve or the branch to the long head of the triceps.
Findings
Twenty-one subjects (83%) obtained triceps reinnervation, and good results (M3 or better) were observed in 19 cases (76%). M4 grade was noted in 36% of the cases, M3 grade in 40%, M2 grade in 8%, M1 grade in 8%, and M0 grade in 8% of the patients. The best outcomes were observed in the cases presenting a C5 to C7 palsy and those in which the nerve to the triceps was chosen as the transfer target.
Conclusions
Reinnervation of the triceps can be achieved in most patients if adequate donor and recipient nerves are carefully selected based on an individual case-specific decision.




Similar content being viewed by others
References
Bhardwaj P, Bhardwaj N (2009) Motor grading of elbow flexion—is Medical Research Council grading good enough? J Brachial Plex Peripher Nerve Inj 13; 4:3
Bekler H, Wolfe VM, Rosenwasser MP (2009) A cadaveric study of ulnar nerve innervation of the medial head of triceps brachii. Clin Orthop Relat Res 467:235–238
Belzberg AJ, Dorsi MJ, Storm PB, Moriarity JL (2004) Surgical repair of brachial plexus: a multinational survey of experienced peripheral nerve surgeons. J Neurosurg 101:365–376
Bengtson KA, Spinner RJ, Bishop AT, Kaufman KR, Coleman-Wood K, Kircher MF, Shin AY (2008) Measuring outcomes in adult brachial plexus reconstruction. Hand Clin 24:410–415
Bertelli JA, Ghizoni MF (2010) Reconstruction of complete palsies of the adult brachial plexus by root grafting using long grafts and nerve transfers to target nerves. J Hand Surg Am 35:1640–1646
Bertelli JA, Santos MA, Kechele PR, Ghizoni MF, Duarte H (2007) Triceps motor nerve branches as a donor or receiver in nerve transfers. Neurosurgery 61(Suppl 2):333–338
Colbert SH, Mackinnon S (2006) Posterior approach for double nerve transfer for restoration of shoulder function in upper brachial plexus palsy. Hand 1:71–77
Doi K, Shigetomi M, Kaneko K, Soo-Heong T, Hiura Y, Hattori Y, Kawakami F (1997) Significance of elbow extension in reconstruction of prehension with reinnervated free-muscle transfer following complete brachial plexus avulsion. Plast Reconstr Surg 100:364–372
Flores LP (2006) Epidemiological study of the traumatic brachial plexus injuries in adults. Arq Neuropsiquiatr 64:88–94
Goubier JN, Teboul F (2007) Transfer of the intercostal nerves to the nerve of the long head of the triceps to recover elbow extension in brachial plexus palsy. Tech Hand Up Extrem Surg 11:139–141
Handling MA, Curtis AS, Miller SL (2010) The origin of the long head of the triceps: a cadaveric study. J Shoulder Elbow Surg 19:69–72
Kawano K, Nagano A, Ochiai N, Kondo T, Mikami Y, Tajiri Y (2007) Restoration of elbow function by intercostal nerve transfer for obstetrical paralysis with co-contraction of the biceps and the triceps. J Hand Surg Eur 32(4):421–426
Madsen M, Marx RG, Millett PJ, Rodeo SA, Sperling JW, Warren RF (2006) Surgical anatomy of the triceps brachii tendon: anatomical study and clinical correlations. Am J Sports Med 34:1839–1843
Mumenthaler M (1969) Some clinical aspects of peripheral nerve lesions. Eur Neurol 2:257–268
O’Brien DF, Park TS, Noetzel MJ, Wheatherly T (2006) Management of birth brachial plexus palsy. Childs Nerv Syst 22:103–112
Shenaq SM, Kim JY, Armenta AH, Nath RK, Cheng E, Jedrisiak K (2004) The surgical treatment of obstetric brachial plexus palsy. Plast Reconstr Surg 113:54E–67E
Terzis JK, Kokkalis ZT (2010) Restoration of elbow extension after primary reconstruction in obstetric brachial plexus palsy. J Pediatr Orthop 30:161–168
Vekris MD, Beris AE, Lykissas MG, Korompilias AV, Vekris AD, Soucacos PN (2008) Restoration of elbow function in severe brachial plexus paralysis via muscle transfers. Injury 39(Suppl 3):S15–S22
Zheng MX, Xu WD, Qiu YQ, Xu JG, Gu YD (2010) Phrenic nerve transfer for elbow flexion and intercostal nerve transfer for elbow extension. J Hand Surg (Am) 35:1304–1309
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
Brachial plexus injuries due to some kinds of lesions have characteristics that need to be understood by neurosurgeons. For closed stretch injuries in cases of both neurapraxia and axonotmesis, reversible lesion functional regeneration usually occurs spontaneously, but the most serious problem is root avulsion lesions. In case of total avulsion the diagnostic as well as treatment options are difficult and in some aspects controversial. Decision-making depends on the preoperative neurological, radiological, and electrophysiological examinations. Horner signs and pseudomeningocele and electrophysiological study (electromyography and sensory nerve conduction examination) usually indicate the root avulsion. The treatment modality in such situations is limited and according to Kline (1) it is the definite diagnosis of root avulsion (false-positive signs of root avulsion 10%, false-negative 32%). According to Mehta (2), open surgery, however, gives us the chance to confirm the type of lesion. In case of partial avulsion, partial mending is possible by means of direct intraplexal repair or neurotization, if applicable. Elbow extension is one of the major restoration challenges, especially in cases of obstetric brachial plexus palsy, and early intraplexus reconstruction of the posterior cord can give excellent results. Terzis' article (3) provides the modern trends in brachial plexus closed injury treatment for C5–C7 spinal root palsy in order to obtain triceps function restoration. The conclusions and message from this article are somewhat limited by the heterogeneity of the different treatment options (9 different techniques were used for 25 patients). On the one hand, it shows that there are many possible options for treating patients and that each case should be considered and approached individually. On the other hand, we have learned from the article that the radial nerve branch of the long head of the triceps is more amenable to repair with nerve transfer methods than the radial nerve. Moreover, the article conveys the message that using the intercostal nerves as donors does not give good results. The paper is well documented, and I would like to point out the good methodology used by the author for patient selection (CT myelography as well as electrophysiology and the British MRC grading scale). Unfortunately, only a short comment is available about the microsurgical methods used in process of nerve repair. As we know, in some cases, progress in microsurgery of the peripheral nerves has made it possible for us to perform side-to-end anastomosis to avoid sacrificing the donor nerve. It is important when using the phrenic nerve as donor, especially in post-traumatic or congenital cases, when only one phrenic nerve functions satisfactorily. I also feel that the role of post-surgical rehabilitation should have been stressed as well in this undoubtedly interesting article.
References
1. Dubuisson AS, Kline DG (2002) Brachial plexus injury: A survey of 100 consecutive cases from a single service. Neurosurgery 51(3):673–681
2. Mehta VS, Banerji AK, Tripathi RP (1993) Surgical treatment of brachial plexus injuries. Br J Neurosurg 7:491–500
3. Terzis JK, Kokkalis ZT (2010) Restoration of elbow extension after primary reconstruction in obstetric brachial plexus palsy. J Pediatr Orthop 30:161–168
Andrzej Radek Lodz
Poland
Rights and permissions
About this article
Cite this article
Flores, L.P. Triceps Brachii Reinnervation in Primary Reconstruction of the Adult Brachial Plexus: Experience in 25 Cases. Acta Neurochir 153, 1999–2007 (2011). https://doi.org/10.1007/s00701-011-1080-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1080-8