Abstract
Objective
The purpose of this study was to evaluate cognitive functions in patients undergoing extracranial-intracranial (EC-IC) bypass surgery for cerebral ischemia.
Population and methods
From August 2003 to January 2009, 276 patients with occluded internal carotid arteries (ICA) were screened. Forty of these met the criteria for a low-flow EC-IC bypass. These patients were identified based on evidence of exhausted vasomotor reactivity (VMR) using the Doppler CO2 test and CT perfusion. These patients were invited to have a complete battery of neuropsychological tests preoperatively and 12 months after surgery. Complete neurocognitive testing was finished in 20 patients.
Results
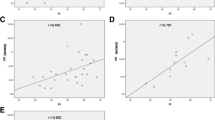
This group of 20 patients showed preoperative cognitive impairment ranging from mild to medium-severe. There were no cases of stroke ipsilateral to the operated side during the follow-up period. VMR improvement was seen in all patients within 6 months of surgery. A comparison using a paired t-test demonstrated significant improvement 12 months after surgery in the following neuropsychological tests: WAIS-R (p = 0.01), Number Collection Test (p = 0.02), Trail Making Test (p = 0.03), and Benton Visual Retention Test (p = 0.05). Repeat analysis of variance (ANOVA) suggested the following predictors associated with cognitive improvement:the presence of ophthalmic collateral flow (p = 0.04), preoperative amaurosis fugax (p = 0.02), and external watershed infarction detected by MRI (p = 0.04).
Conclusion
Patients with occlusion of the ICA and exhausted VMR have cognitive impairment prior to EC-IC bypass surgery. Twelve months after surgery, there is significant improvement in various areas of cognition.
Similar content being viewed by others
Abbreviations
- ANOVA:
-
Repeat analysis of variance
- ASA:
-
Anopyrin acetylsalicylic acid
- BH/HV:
-
Breath-holding/hyperventilation
- CABG:
-
Coronary artery bypass graft
- CAS:
-
Internal carotid artery stenting
- CEA:
-
Carotid endarterectomy
- VMR:
-
Vasomotor reactivity
- DSA:
-
Digital subtraction angiography
- EC-IC bypass:
-
Extracranial-intracranial bypass
- ICA:
-
Internal carotid artery
- MRI:
-
Magnetic resonance imaging
- PCA:
-
Principle component analysis
- STA:
-
Superficial temporal artery
- TCD:
-
Transcranial Doppler
- TIA:
-
Transient ischemic attack
- WAIS-R:
-
Wechsler Adult Intelligence Scale-Revised
References
Aaslid R, Eden A, Ringelstein EB (1986) Transcranial Doppler sonography. Springer, Wien
Adams HP, Powers WJ, Grubb RL, Clarke WR, Woolson RF (2001) Preview of a new trial of extracranial-to-intracranial arterial anastomosis: the carotid occlusion surgery study. Neurosurg Clin N Am 12(3):613–624
Bakker FC, Klijn CJM, Jennekens-Schnikel A, Kappelle LJ (2000) Cognitive disorders in patients with occlusive disease of the carotid artery—a systematic review of the literature. J Neurol 247:669–676
Bakker FC, Klijn CJM, Jennekens-Schinkel A, van der Tweel I, van der Grond J, van Huffelen AC, Tulleken CAF, Kappelle LJ (2003) Cognitive impairment is related to cerebral lactate in patients with carotid artery occlusion and ipsilateral transient ischemic attacks. Stroke 34:1419–1424
Bakker FC, Klijn CJM, van der Grond J, Kappell LJ, Jennekens-Schinkel A (2004) Cognition and quality of life in patients with carotid artery occlusion. A follow-up study. Neurology 62:2230–2235
Beneš V, Kramář F, Mohapl M, Stejskal L (2003) Karotická endarterektomie. In: Beneš V et al Ischémie mozku. Chirurgická a endovaskulární terapie. Galén pp 96-98
Binder LM, Tanabe CT, Waller F, Wooster NE (1982) Behavioral effects of superficial temporal artery to middle cerebral artery bypass surgery: preliminary report. Neurology 32:422–424
Bishop CFR, Powell S, Insall M (1986) The effect of internal carotid artery occlusion on middle cerebral artery blood flow at rest and response to hypercapnia. Lancet 1:710–712
Brown GC, Ewing JR, Weiss SM, Robertson WM, Welch KMA (1983) Neuropsychological correlates of regional cerebral blood flow in candidates for extracranial to intracranial bypass. J Cereb Blood Flow Metab 3(suppl l):S594–S595
Caplan LR, Hennerici M (1998) Impaired clearence of emboli (washout) is an important link between hypoperfusion, embolism and ischemic stroke. Arch Neurol 55:1475–1482
Delaney RC, Wallace JD, Egelko S (1980) Transient cerebral ischemic attacks and neuropsychological deficit. J Clin Neuropsychol 2:107–114
Desmond DW, Moroney JT, Sano M, Stern Y (2002) Incidence of dementia after ischemic stroke. Stroke 33:2254–2260
Drinkwater JE, Thopson SK, Lumley JSP (1984) Cerebral function before and after extra-intracranial carotid bypass. J Neurol Neurosurg Psychiatry 47:1041–1043
Dull RA, Brown GG, Shatz MW, Diaz FG, Ausman JI (1982) Preoperative neurobehavioral impairment in cerebral revascularisation candidates. J Clin Neuropsychol 4:151–165
EC/IC Bypass Study Group (1985) Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med 313:1191–1200
Fearn SJ, Pole R, Wesnes K, Faragher EB, Hooper TL (2001) Cerebral injury during cardiopulmonary bypass; emboli impair memory. J Thorac Cardiovasc Surg 121:1150–1160
Garret MC, Komotar JR, Sarke RM, Merkow MB, Otten ML, Sciacca RR, Connoly ES (2009) The efficacy of direct extracranial-intracranial bypass in the treatment of symptomatic hemodynamic failure secondary to athero-occlusive disease: A systematic review. Clin Neurol Neurosurg 111:319–326
Ghogawala Z, Westerveld M, Amin-Hanjani S (2008) Cognitive outcomes after carotid revascularization: the role of cerebral emboli and hypoperfusion. Neurosurgery 62:385–395
Grubb RL Jr, Derdeyn CP, Fritsch SM, Carpenter DA, Yundt KD, Videen TO, Spitznagel EL, Powers WJ (1998) Importance of hemodynamic factors in the prognosis of symptomatic carotid occlusion. JAMA 280:1055–1060
Hachinski V (1994) Vascular dementia: a radical redefinition. Dementia 5:130–132
Hamster W, Diener HC (1984) Neuropsychological changes associated with stenoses or occlusions of the carotid arteries. Eur Arch Psychiatr Neurol Sci 5:69–73
Haynes RB, Mukherjee J, Sackett DL, Taylor DW, Barnett JH, Peerles SJ (1987) Functional status changes following medical or surgical treatment for cerebral ischemia. Results of the extracranial-intracranial bypass study. JAMA 257:2043–2046
Hoeffner EG, Case I, Jain R, Gujar SK, Shah GV, Deveikis JP, Carlos RC, Thompson BG, Harrigan MR, Mukherji SK (2004) Cerebral perfusion CT: technique and clinical applications. Radiology 231:632–644
Iwama T, Hashimoto N, Hayashida K (2001) Cerebral hemodynamic parameters for patients with neurological improvements after extracranial-intracranial arterial bypass surgery: evaluation using positron emission tomography. Neurosurgery 48:504–512
Jacques S, Garner JT (1976) Reversal of aphasia with superficial temporal artery to middle cerebral artery anastomosis. Surg Neurol 5:143–145
Jinnouchi J, Toyoda K, Inoue T, Fujimoto S, Gotoh S, Yasumori K et al (2006) Changes in brain volume 2 years after extracranial-intracranial bypass surgery: a preliminary subanalysis of the Japanese EC-IC trial. Cerebrovasc Dis 22:177–182
Kleiser B, Scholl D, Widder B (1994) Assessment of cerebrovascular reactivity by Doppler CO2 and Diamox testing: which is the appropriate method? Cerebrovasc Dis 4:134–138
Kleiser B, Widder B (1992) Course of carotid artery occlusions with impaired cerebrovascular reactivity. Stroke 23:171–174
Knosp SC, Matatko N, Wilhelm H (2004) Evaluation of brain injury after coronary artery bypass grafting. A prospective study using neuropsychological assesment and diffusion-weighted magnetic resonance imaging. Eur J Cardiothorac Surg 25:791–800
Lal BK (2007) Cognitive function after carotid artery revascularization. Vasc Endovasc Surg 41(1):5–13
Larr PJ, van der Grond J, Bremmer PJ, Klijn CJM, Hendrikse J (2008) Assessment of the contribution of the external carotid artery to brain perfusion in patients with internal carotid artery occlusion. Stroke 39:3003–3008
Lezak MD, Howieson DB, Loring, DW (2004) Neuropsychological assessment. 4th ed. Oxford Univeristy Press
Markus HS, Harrison MJG (1992) Estimation of cerebrovascular reactivity using transcranial Doppler, including the use of breath-holding as the vasodilatory stimulus. Stroke 23:668–673
Meyer JS, Rauch G, Rauch RA, Haque A (2000) Risk factors for cerebral hypoperfusion, mild cognitive impairment and dementia. Neurobiol Aging 21:161–169
Momjian-Mayor I, Baron JC (2005) The pathophysiology of watershed infarction in internal carotid artery disease. Review of cerebral perfusion studies. Stroke 36:567–577
NASCET collaborators (1999) The North American symptomatic carotid endarterectomy trial. Surgical results in 1415 patients. Stroke 30:1751–1758
Nielsen H, Hojer-Pedersen E, Gulliksen G, Haase J (1985) A neuropsychological study of twelve patients with transient ischemic attacks before and after EC/IC bypass surgery. Acta Neurol Scand 71:317–20
Nielsen H, Hojer-Pedersen E, Gulliksen G, Haase J, Enevoidsen E (1986) Reversible ischemic neurological deficit and minor strokes before and after EC/IC bypass surgery. A neuropsychological study. Acta Neurol Scand 73:615–618
Nollert G, Mohnle P, Tassan-Preil P (1995) Postoperative neuropsychological dysfunction and cerebral oxygenation during cardiac surgery. Thorac Cardiovasc Surg 43:260–264
Ogasawara K, Inoue T, Kobayashi M, Fukuda T, Komoribayashi N, Saitoh H, Yamadate K, Ogawa A (2006) Cognitive impairment associated with intraoperative and postoperative hypoperfusion without neurologic deficits in a patient undergoing carotid endarterectomy. Surg Neurol 65:577–80
Paulson GW, Kapp J, Cook W (1966) Dementia associated with bilateral carotid artery disease. Geriatrics 21:159–166
Payk TR, Wassmann H, Schumacher V, Boilbach R (1986) Psychometric studies of cerebral performance before and following extra-intracranial bypass operations. Nervenarzt 57:244–248
Peerless SJ, Charter NI, Ferguson GF (1977) Multiple-vessel occlusion in cerebrovascular disease-a further follow-up of the effects of microvascular bypass on the quality of life and the incidence of stroke. In: Schmiedek P (ed) Microsurgery for Stroke. Springer, New York, pp 251–259
Perry PM, Drinkwater J, Taylor GW (1975) Cerebral function before and after carotid endarterectomy. Br Med J 25:215–216
Pohjasvaara T, Erkinjuntti T, Vataja R, Kaste M (1997) Dementia three months after stroke: baseline frequency and effect of different definitions of dementia in the Helsinki stroke aging memory study (SAM) cohort. Stroke 28(4):785–792
Preiss M, Rodriguez M, Kawaciuková R, Laing H (2007) Neuropsychologická baterie Psychiatrického centra Praha. In: Preiss M, Rodriguez M (eds) Klinické vyšetření základních kognitivních funkcí, 2nd edn. Psychiatrické centrum Praha, Praha
Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K, Gorelick P, Harbaugh R, Katzan I, Kenton EJ, Schwamm LH (2006) Guidelines for prevention of stroke or transient ischemic attack. A statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke. Stroke 37:577–617
Sasoh M, Ogasawara K, Kuroda K, Okuguchi T, Terasaki K, Yamadate K, Ogawa A (2003) Effects of EC-IC bypass surgery on cognitive impairment in patients with hemodynamic cerebral ischemia. Surg Neurol 59:455–460
Schmiedek P, Piepgras A, Leinsinger G, Kirsch CM, Einhaupl K (1994) Improvement of cerebrovascular reserve capacity by EC-IC arterial bypass surgery in patients with ICA occlusion and hemodynamic cerebral ischemia. J Neurosurg 81:236–244
Shaw PJ, Bates D, Cartidge NE (1986) Early intellectual dysfunction following coronary bypass surgery. Q J Med 58:59–68
Tatemichi TK, Desmond DW, Prohovnik I, Eidelberg D (1995) Dementia associated with bilateral carotid occlusions: neuropsychological and haemodynamic course after extracranial to intracranial bypass surgery. J Neurol Neurosurg Psychiatry 58(5):633–6
Vajkozcy P, Horn P, Schmiedek P (1999) Standard superficial temporal artery-middle cerebral artery bypass surgery in hemodynamic cerebral ischemia: indication and technique. Operat Tech Neurosurg 2:106–115
Van Dijk D, Jansen EWL, Hijman R, Nierich AP, Diephuis JC, Moons KGM, Lahpor JR, Borst C, Keizer AM, Nathoe HM, Grobbee DE, De Jaegere PP, Kalkman CJ (2002) Cognitive outcome after off-pump and on-pump coronary artery bypass graft surgery. A randomized trial. JAMA 287:1405–1412
Van Dijk D, Keizer AMA, Diephuis JC, Durand C, Vos LJ, Hijman R (2000) Neurocognitive dysfunctions following coronary artery bypass surgery: a systematic review. J Thorac Cardiovasc Surg 120:632–639
Widder B, Kleiser B, Krapf H (1994) Course of cerebrovascular reactivity in patients with carotid artery occlusions. Stroke 25:1963–1967
Yamauchi Y, Fukuyama H, Nagahama Y, Katsumi Y, Dong Y, Konishi J, Kimura J (1996) Atrophy of the corpus callosum associated with cognitive impairment and widespread cortical hypometabolism in carotid artery occlusive disease. Arch Neurol 53:1103–9
Yaşargil MG (1969) Microsurgery applied to neurosurgery. Georg Thieme, Stuttgart, pp 105–115
Younkin D, Hungerbuhler JP, O Connor M, Goldberg H, Burke A (1985) Superficial temporal-middle cerebral artery anastomosis: effects on vascular, neurologic, and neuropsychological functions. Neurology 35:462–469
Acknowledgements
The authors acknowledge the cooperation of V. Šnorek for his suggestions from the viewpoint of a psychologist standing outside the trial, Prof. J. Hernesniemi and M. Lehečka for critical remarks, and V. Apok for her assistance with the English version of the text.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The authors present data on the haemodynamic and cognitive recovery after EC-ICbypass surgery. Since the haemodynamic assessment used in the study did not represent the state of the art, only a general improvement of vasoreactivity could be identified postoperatively. Correlation of cognitive improvement with pre- and postoperative factors suggested the presence of ophthalmic collateral flow, preoperative amaurosis fugax and preoperative watershed infarction as principal factors for cognitive recovery. The principal question that remains because of a missing control group, is that part of the cognitive improvement may represent the natural recovery phase from preoperative strokes.
H. J. Steiger
Duesseldorf, Germany
In the present study, Fiedler and coworkers report on 20 patients with chronic hemodynamic insufficiency who underwent EC-IC bypass surgery. The patients were assessed preoperatively and postoperatively over a time period of 6 months by neurological exams, functional CBF studies as well as a detailed neuropsychological testing. The authors demonstrate a significant improvement of neurological deficits and cognitive function in their patients. This is an important manuscript. The primary aim of revascularisation surgery in chronic hemodynamic insufficiency is secondary stroke prevention. The fact that neurological and neuropsychological deficits may improve in parallel to CVRC normalization is, so far, an insufficiently recognized observation. The neuropsychological assessment in this study has been performed thoroughly, leaving no doubt about the important message of the manuscript. The authors state in the Discussion Section that ´ It is the evidence of hemodynamic failure in chronic ICA occlusion that is a primary indication for EC-IC bypass. Therefore, such a significant degree of improvement in neurological symptoms postoperatively might be expected´. I would disagree. Chronic hemodynamic insufficiency describes a state with only little to moderate reduction of baseline CBF and loss of CVRC. The mechanism describing how neuropsychological deficits can improve following normalization of CVRC remains not understood. This circumstance in fact makes the results of the authors scientifically interesting.
P. Vajkoczy
Berlin, Germany
Rights and permissions
About this article
Cite this article
Fiedler, J., Přibáň, V., Škoda, O. et al. Cognitive outcome after EC-IC bypass surgery in hemodynamic cerebral ischemia. Acta Neurochir 153, 1303–1312 (2011). https://doi.org/10.1007/s00701-011-0949-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-0949-x