Abstract
Background
Previously, we reported on our single centre results regarding the diagnostic yield of stereotactic needle biopsies of brain lesions. The yield then (1996–2006) was 89.4%. In the present study, we review and evaluate our experience with intraoperative frozen-section histopathologic diagnosis on-demand in order to improve the diagnostic yield.
Methods
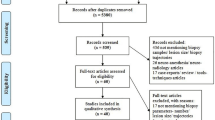
One hundred sixty-four consecutive frameless biopsy procedures in 160 patients (group 1, 2006–2010) were compared with the historic control group (group 2, n = 164 frameless biopsy procedures). Diagnostic yield, as well as demographics, morbidity and mortality, was compared. Statistical analysis was performed by Student's t, Mann–Whitney U, Chi-square test and backward logistic regression when appropriate.
Results
Demographics were comparable. In group 1, a non-diagnostic tissue specimen was obtained in 1.8%, compared to 11.0% in group 2 (p = 0.001). Also, both the operating time and the number of biopsies needed were decreased significantly. Procedure-related mortality decreased from 3.7% to 0.6% (p = 0.121). Multivariate analysis only proved operating time (odds ratio (OR), 1.012; 95% confidence interval (CI), 1.000–1.025; p = 0.043), a right-sided lesion (OR, 3.183; 95% CI, 1.217–8.322; p = 0.018) and on-demand intraoperative histology (OR, 0.175; 95% CI, 0.050–0.618; p = 0.007) important factors predicting non-diagnostic biopsies.
Conclusions
The importance of a reliable pathological diagnosis as obtained by biopsy must not be underestimated. We believe that when performing stereotactic biopsy for intracranial lesions, next to minimising morbidity, one should strive for as high a positive yield as possible. In the present single centre retrospective series, we have shown that using a standardised procedure and careful on-demand intraoperative frozen-section analysis can improve the diagnostic yield of stereotactic brain biopsy procedures as compared to a historical series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In an earlier report, we demonstrated our single centre results with both frame-based and frameless neuronavigational image-guided techniques in the context of needle biopsies of brain lesions [7]. We reported no differences in diagnostic yield, complications and biopsy-related mortality between both techniques, as corroborated by others [36, 40, 41].
On the matter of diagnostic yield, we discussed the possible importance of intraoperative frozen-section or cytological smear preparations. Our previous results, when no intraoperative histological diagnosis was readily available, showed an overall diagnostic yield of 89.4%, which is on the lower spectrum of yield reported by others [1, 9, 11, 12, 17, 19, 34, 36, 40]. We believe that neurosurgeons should strive for as high a diagnostic yield as possible, respecting the possible morbidity or even mortality, although small, the patient confronts when undergoing an intracranial biopsy procedure. Since several authors have shown the benefit of intraoperative histopathologic diagnosis and/or the use of modern intraoperative imaging techniques, improving the diagnostic yield up to as high as 99.2% [4, 14, 20, 22, 31, 32], we implemented intraoperative histopathologic diagnosis into our standardised biopsy procedure in order to possibly improve on our results.
In the present study, we reviewed and evaluated our experience with the use of intraoperative frozen-section diagnosis on-demand, when the neurosurgeon performing the biopsy on macroscopic observation was hesitant about the pathologic nature of the tissue sample.
Patients and methods
We reviewed a consecutive series of patients who had undergone an image-guided stereotactic intracranial biopsy procedure at the Erasmus MC from November 2006 until January 2010. This series of patients succeeded the series of 465 uninterrupted cerebral biopsies, of which 164 were frameless biopsy procedures, published in our earlier report [7]. The data were prospectively gathered, but reviewed in a retrospective manner. One hundred sixty-four frameless biopsy procedures were performed in 160 patients.
Patient and pre-operative neuroimaging characteristics
Age, gender, post-operative biopsy-related complications (morbidity) and mortality, duration of hospital stay as well as operating time, biopsy method used, number of biopsies and complications were extracted from case notes and operative reports. The site of the targeted lesion was obtained from pre-operative computed tomographic or magnetic resonance (MR) imaging. The eventual diagnosis was obtained from the pathological report, from which the diagnostic yield was determined.
Operative technique
The techniques of frameless image-guided stereotactic biopsies applied in our centre have been described previously [7]. One hundred sixty-four biopsies were performed using the frameless stereotaxy protocol under general anaesthesia and head-fixation in a three-point Mayfield clamp. Intraoperative image guidance and the surgical plan were obtained using the Stealth Treon™ system (Medtronic Inc., Minneapolis, MN, USA). Tissue samples approximately 8-mm-long and 1-mm-thick were thus obtained.
In general, four biopsies were obtained at the pre-operatively suggested target, as well as two to four more biopsies at a site proximal to the target on the same biopsy trajectory. The macroscopic aspect of the biopsy was assessed, and it was considered pathological when one or more of the following was observed: (1) glazy/oedematous aspect, (2) haemorrhagic component and (3) dark-greyish aspect. A brain tissue sample was regarded normal when clearly white matter was observed. Intraoperative freeze sectioning was performed, only then when the surgeon was uncertain about the pathologic nature of the tissue sample, i.e. the macroscopic appearance of the acquired tissue resembled normal brain. If diagnostic tissue was not obtained, all parameters and measurements were rechecked to ensure accurate localisation, after which, a repeat biopsy sample could then be sent, via the same or a new trajectory, if need be.
Statistical analysis
Statistical analysis was performed with SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA). The present 164 biopsies, with the abovementioned standardised procedure and intraoperative histopathologic diagnosis on-demand (group 1), were compared to the historic control of 164 frameless biopsies that were reported previously and did not include intraoperative diagnosis (group 2). Continuous data were compared using the Student's t test for parametric data. For non-parametric data, the Mann–Whitney U test was used. These are presented as mean values ± standard deviations, unless otherwise specified. Proportions were compared with Chi-square and Fisher's exact test and presented as percentages. p values <0.05 were considered statistically significant. In order to analyse factors relating to the risk of a non-diagnostic biopsy, the variables selected were dichotomised and initially explored univariately as described above. Variables for which there was not a high probability of association (p > 0.10) were excluded from the final regression model. Backward stepwise logistic regression was used for this purpose, and odds ratios (OR) and 95% confidence intervals (CI) are presented.
Results
In Table 1, patient and peri-operative characteristics of stereotactic biopsies in patients of group 1 and 2 are shown. There were no differences in age and gender distribution. The peri-operative complication rate was also similar. Interestingly, the number of biopsies taken and the overall operating time both decreased significantly (p < 0.001 and p < 0.001, respectively) when comparing with the historical group 2.
The location of the lesion intended for biopsy was not significantly different when compared to side and anatomical site. Left- and right-sided lesions were equally divided (group 1 vs. group 2, 39.0% and 36.0% vs. 39.6% and 40.9%, respectively). In patients of group 1, the three most often biopsied tumours were frontal (22.5%), parietal (22.0%) and thalamic (14.0%) lesions.
Post-operative complications occurred in 14 (8.5%) and 19 (11.6%) of operations in groups 1 and 2, respectively. Of these, four symptomatic haemorrhages in each group (2.4%) were diagnosed by post-operative computed tomography. There was no statistically significant difference between groups 1 and 2 in the frequency of occurrence of post-operative complications. In the most recent patients (group 1), there was one death (0.6%) attributable to the surgical procedure, i.e. death occurring within 30 days as a result of symptomatic post-operative haemorrhage or oedema. There were six biopsy-related deaths (3.7%) in group 2, which did not reach statistical significance (p = 0.121, Fisher's exact).
Diagnostic yield
The overall diagnostic yield of group 1 was 98.2%, i.e. a histological diagnosis was established in 161 of 164 biopsy procedures, whereas in three (1.8%), the biopsy was non-diagnostic. In one patient, this resulted in a repeated biopsy procedure that resulted in the diagnosis of a lymphoma. The second and third patient underwent a subsequent craniotomy when a glioblastoma and metastasis of lung carcinoma was diagnosed, respectively. In 15 cases (8.9%), the surgeon judged the tissue obtained to resemble normal brain and therefore requested for an intraoperative frozen-section diagnosis by the neuropathologist. When non-diagnostic, this prompted for another tissue sample in the chosen trajectory. In the period from August 1996 until October 2006, i.e. group 2, when there was no availability of intraoperative histopathologic diagnosis, the diagnostic yield was only 89.0%, which is statistically lower compared with group 1 diagnostic yield (p = 0.001). Table 2 shows the histological diagnoses that were made on the tissue samples taken in both groups. On average, 7.4 (range, 1–19) and 9.0 (1–24) tissue samples were taken during the biopsy procedure in groups 1 and 2, respectively (p < 0.001, Table 1).
Table 3 shows the results of the univariate analysis performed to establish the factors related to obtaining a non-diagnostic biopsy specimen (n = 21). In the subsequent multivariate regression analysis, only operating time (OR, 1.012; 95% CI, 1.000–1.025; p = 0.043), a right-sided lesion (OR, 3.183; 95% CI, 1.217–8.322; p = 0.018) and the use of on-demand intraoperative histopathologic examination (OR, 0.175; 95% CI, 0.050–0.618; p = 0.007) showed to be important factors.
Discussion
Previously, we have shown the diagnostic yield of stereotactic biopsy either by frame-based or frameless techniques to be equal, as were the morbidity and mortality related to the procedure [7]. The overall diagnostic yield in the previous report was 89.4%, which might be regarded lying on the lower spectrum of the yield obtained by others [1, 9, 11, 12, 17, 19, 34, 36, 40]. The present study suggests that by using on-demand frozen-section analysis of tissue specimens begotten by biopsy, the diagnostic yield can be dramatically improved (98.2%).
Several other authors have corroborated these results, i.e. performing intraoperative frozen-section or cytological smear preparations will increase the rate on a reliable histopathological diagnosis up to as high as 99.2% [4, 14, 17, 29, 31, 38]. McDermott and Bernstein, in Neuro-oncology: The Essentials (p. 115), actually state ‘[…] The management of the failed biopsy begins in the operating room where intraoperative examination of tissue is mandatory to ensure that diagnostic tissue is in fact obtained […]’. Nevertheless, the five most recent reports, illustrating diagnostic yields of 99.3% [35], 94% [30], 90.6% [5], 89.8% [1] and 83.6% [37], do not mention intraoperative pathologic confirmation. Also, in our series, we were not able to perform intraoperative cytological studies in all biopsy procedures. This was primarily due to logistic considerations, such as pressure on the operating theatre regarding time and the unavailability of adequate neuropathologic support on all biopsies. Therefore, we turned to on-demand frozen-section analysis, i.e. the surgeon performing the biopsy assessed the tissue specimen macroscopically as normal brain or pathological tissue sample and, when uncertain, requested the neuropathologist for intraoperative confirmation. Apparently, concluded from the results shown in the present study, there is no need for an intraoperative cytological preparation, and therefore, a neuropathologist standby for every stereotactic cerebral biopsy procedure when an experienced surgeon evaluates the tissue samples obtained. These results are corroborated by the recent article of Shooman et al. who on top of this state that routine intraoperative neuropathological examination is not needed at all [35].
Table 4 shows the diagnostic yield, complication rates, deaths and methods used to ensure a greater diagnostic yield in the most recent biopsy series. Since 2001, a total of 12,038 biopsy procedures are collected in the literature, with an overall diagnostic yield ranging from 83.6% to 100%. Positron emission tomography imaging, MR perfusion and MR imaging spectroscopy integrated into the planning for stereotactic biopsy procedures to determine the trajectory and selection of the appropriate target promise to be important adjuncts to improve diagnostic yield and to decrease sampling error, especially when low-grade gliomas are involved [6, 13, 15, 24, 27, 28, 32, 33]. Recent studies show a yield of 100%, although patient numbers are relatively small [6, 13, 15, 24, 32, 33]. Additional use of metabolic imaging data acquired with MR spectroscopy, more specifically, the ratio of N-acetyl aspartate and choline-containing compounds, for target selection can potentially increase the diagnostic efficacy of biopsy procedures.
Another issue to be addressed is the diagnostic accuracy, i.e. the rate of sampling error as established by subsequent open craniotomy. In literature, accuracy rates ranging from 73% to 97% have been reported [2, 7, 17, 30, 40]. Chernov et al. compared the diagnostic efficacy of stereotactic brain biopsy performed with and without additional use of spectroscopic imaging and found that spectroscopy was superior, although not significantly due to the small number of patients, in reaching a diagnosis at all (100% vs. 90%) [6]. Diagnostic accuracy, however, could not be improved by using spectroscopy imaging (67% vs. 79%, MR imaging with and without spectroscopy, respectively).
In the present study, an important difference with the historical control was the use of on-demand intraoperative histological confirmation of pathological tissue, which was confirmed by multivariate analysis to be an important factor to decrease the chance on a non-diagnostic tissue specimen. However, due to the retrospective nature of the present study, some confounding factors should be put forward that may influence the overall results. As a result of technological advance and ease of use, the frameless stereotactic technique has been used more frequently in recent times at our neurosurgical clinic (97.6% vs. 35.3%, respectively). Although we, in concordance with others, have previously shown that this does not influence diagnostic yield [7, 36, 40, 41], Dorward et al. found disagreeing results, concluding that frameless techniques are superior to the gold standard of frame-based biopsy [8]. To exclude this possible confounding factor, we compared the most recent frameless biopsy series (group 1) with the historical control of frameless biopsies only. Furthermore, the effect of an initial learning curve cannot be ruled out. Another, more important factor might be the number of surgeons performing the biopsy procedures. These differ significantly between the historical and the present group of patients. In group 2, a total of 20 surgeons, whereas in group 1, only 15 surgeons were involved with the stereotactic biopsy procedures. In the most recent group (group 1), two surgeons (RD and JWS) performed 51.8% of surgeries and supervised another 12.8%. One might argue that due to a surgeon's increased experience, he/she is apt to prepare a biopsy trajectory and target that ensures less chance on complications and a higher chance on a positive histological diagnosis. For this, there is no evidence in recent literature as far as we are aware, although Shastri-Hurst et al. touched upon the subject in the “Results” section and found no evidence that the individual performing the biopsy most frequently had better results in terms of complication rate or non-diagnostic rate [34]. Lastly, the recent 164 cases were all histologically examined by one experienced dedicated neuropathologist (JMK), whereas in the past, three pathologists performed the histopathologic diagnosis. A single dedicated neuropathologist might be able to provide a diagnosis more often. Furthermore, the changing tumour classification and grading by the World Health Organisation might aid to construct a more proficient diagnosis nowadays.
The possible advantages of on-demand intraoperative frozen-section analysis are its cost-effectiveness concerning the consultation of a neuropathologist and the need for repeat surgery. More importantly, a non-diagnostic biopsy has an imminent effect on a patient's further treatment. On-demand histopathology, however, demands experienced and dedicated neuro-oncologic trained neurosurgeons [35]. Nevertheless, the issue of diagnostic accuracy, i.e. biopsy sampling error, remains unresolved. As described above, newly available diagnostic techniques might add to locate the adequate biopsy site and decrease sampling error.
Although tumour verification might be warranted, the treating physician should always also consider the morbidity and mortality related to the biopsy procedure. Of the 12,038 procedures in recent literature (Table 4), the average procedure-related morbidity was 4.7% (range, 0.7–16.1%), compared to our own recent series (8.5%). These vary from minor complications to devastating neurological sequelae that can influence a patients' independence. The average mortality rate was 0.9% (range, 0–3.9%) and 0.6% in recent literature and the present series, respectively, from which one might conclude that a brain biopsy is a safe procedure.
Concluding, the importance of a reliable pathological diagnosis as obtained by biopsy, notwithstanding the possibility of sampling error [25, 28], must not be underestimated. Both with regard to the possible risks for the patients, such as (increase of) neurological deficits by oedema or haemorrhage and even death, as well as with regard to the further treatment that might be warranted for each individual patient. In the present single centre retrospective series, we have shown that using a standardised procedure and careful on-demand intraoperative frozen-section analysis, when the macroscopic aspects is not clearly pathological, can improve the diagnostic yield of stereotactic brain biopsy procedures as compared to a historical series.
References
Air EL, Leach JL, Warnick RE, McPherson CM (2009) Comparing the risks of frameless stereotactic biopsy in eloquent and noneloquent regions of the brain: a retrospective review of 284 cases. J Neurosurg 111:820–824
Aker FV, Hakan T, Karadereler S, Erkan M (2005) Accuracy and diagnostic yield of stereotactic biopsy in the diagnosis of brain masses: comparison of results of biopsy and resected surgical specimens. Neuropathology 25:207–213
Bhardwaj RD, Bernstein M (2002) Prospective feasibility study of outpatient stereotactic brain lesion biopsy. Neurosurgery 51:358–361
Brainard JA, Prayson RA, Barnett GH (1997) Frozen section evaluation of stereotactic brain biopsies: diagnostic yield at the stereotactic target position in 188 cases. Arch Pathol Lab Med 121:481–484
Chen CC, Hsu PW, Erich Wu TW, Lee ST, Chang CN, Wei KC, Chuang CC, Wu CT, Lui TN, Hsu YH, Lin TK, Lee SC, Huang YC (2009) Stereotactic brain biopsy: single center retrospective analysis of complications. Clin Neurol Neurosurg 111:835–839
Chernov MF, Muragaki Y, Ochiai T, Taira T, Ono Y, Usukura M, Maruyama T, Nakaya K, Nakamura R, Iseki H, Kubo O, Hori T, Takakura K (2009) Spectroscopy-supported frame-based image-guided stereotactic biopsy of parenchymal brain lesions: comparative evaluation of diagnostic yield and diagnostic accuracy. Clin Neurol Neurosurg 111:527–535
Dammers R, Haitsma IK, Schouten JW, Kros JM, Avezaat CJ, Vincent AJ (2008) Safety and efficacy of frameless and frame-based intracranial biopsy techniques. Acta Neurochir (Wien) 150:23–29
Dorward NL, Paleologos TS, Alberti O, Thomas DG (2002) The advantages of frameless stereotactic biopsy over frame-based biopsy. Br J Neurosurg 16:110–118
Ferreira MP, Ferreira NP, Pereira Filho Ade A, Pereira Filho Gde A, Franciscatto AC (2006) Stereotactic computed tomography-guided brain biopsy: diagnostic yield based on a series of 170 patients. Surg Neurol 65(S1):27–32
Gralla J, Nimsky C, Buchfelder M, Fahlbusch R, Ganslandt O (2003) Frameless stereotactic brain biopsy procedures using the Stealth Station: indications, accuracy and results. Zentralbl Neurochir 64:166–170
Grossman R, Sadetzki S, Spiegelmann R, Ram Z (2005) Haemorrhagic complications and the incidence of asymptomatic bleeding associated with stereotactic brain biopsies. Acta Neurochir (Wien) 147:627–631
Hall WA (1998) The safety and efficacy of stereotactic biopsy for intracranial lesions. Cancer 82:1749–1755
Hemm S, Rigau V, Chevalier J, Picot MC, Bauchet L, El Fertit H, Rodriguez MA, Cif L, Vayssiere N, Zanca M, Baldet P, Segnarbieux F, Coubes P (2005) Stereotactic coregistration of 201Tl SPECT and MRI applied to brain tumor biopsies. J Nucl Med 46:1151–1157
Heper AO, Erden E, Savas A, Ceyhan K, Erden I, Akyar S, Kanpolat Y (2005) An analysis of stereotactic biopsy of brain tumors and nonneoplastic lesions: a prospective clinicopathologic study. Surg Neurol 64(Suppl 2):S82–S88
Hermann EJ, Hattingen E, Krauss JK, Marquardt G, Pilatus U, Franz K, Setzer M, Gasser T, Tews DS, Zanella FE, Seifert V, Lanfermann H (2008) Stereotactic biopsy in gliomas guided by 3-tesla 1H-chemical-shift imaging of choline. Stereotact Funct Neurosurg 86:300–307
Kaakaji W, Barnett GH, Bernhard D, Warbel A, Valaitis K, Stamp S (2001) Clinical and economic consequences of early discharge of patients following supratentorial stereotactic brain biopsy. J Neurosurg 94:892–898
Kim JE, Kim DG, Paek SH, Jung HW (2003) Stereotactic biopsy for intracranial lesions: reliability and its impact on the planning of treatment. Acta Neurochir (Wien) 145:547–554
Kongkham PN, Knifed E, Tamber MS, Bernstein M (2008) Complications in 622 cases of frame-based stereotactic biopsy, a decreasing procedure. Can J Neurol Sci 35:79–84
Krieger MD, Chandrasoma PT, Zee CS, Apuzzo ML (1998) Role of stereotactic biopsy in the diagnosis and management of brain tumors. Semin Surg Oncol 14:13–25
Kuhn SA, Romeike B, Walter J, Kalff R, Reichart R (2009) Multiplanar MRI-CT fusion neuronavigation-guided serial stereotactic biopsy of human brain tumors: proof of a strong correlation between tumor imaging and histopathology by a new technical approach. J Cancer Res Clin Oncol 135:1293–1302
Landriel F, Hem S, Hasdeu S, Kitroser M, Peña L, Ajler P, Ciraolo C, Knezevich F (2008) Biopsia estereotáctica cerebral guiada tomográficamente análisis de una serie de 192 casos. Rev Argent Neuroc 22:110–113
Levivier M, Goldman S, Pirotte B, Brucher JM, Baleriaux D, Luxen A, Hildebrand J, Brotchi J (1995) Diagnostic yield of stereotactic brain biopsy guided by positron emission tomography with [18F]fluorodeoxyglucose. J Neurosurg 82:445–452
Lunsford LD, Niranjan A, Khan AA, Kondziolka D (2008) Establishing a benchmark for complications using frame-based stereotactic surgery. Stereotact Funct Neurosurg 86:278–287
Maia AC Jr, Malheiros SM, da Rocha AJ, Stavale JN, Guimaraes IF, Borges LR, Santos AJ, da Silva CJ, de Melo JG, Lanzoni OP, Gabbai AA, Ferraz FA (2004) Stereotactic biopsy guidance in adults with supratentorial nonenhancing gliomas: role of perfusion-weighted magnetic resonance imaging. J Neurosurg 101:970–976
McDermott MW, Bernstein M (2008) Image-guided surgery. In: Bernstein M, Berger MS (eds) Neuro-oncology: the essentials. Thieme Medical Publishers, Inc, New York, pp 112–125
McGirt MJ, Woodworth GF, Coon AL, Frazier JM, Amundson E, Garonzik I, Olivi A, Weingart JD (2005) Independent predictors of morbidity after image-guided stereotactic brain biopsy: a risk assessment of 270 cases. J Neurosurg 102:897–901
Mosskin M, Ericson K, Hindmarsh T, von Holst H, Collins VP, Bergstrom M, Eriksson L, Johnstrom P (1989) Positron emission tomography compared with magnetic resonance imaging and computed tomography in supratentorial gliomas using multiple stereotactic biopsies as reference. Acta Radiol 30:225–232
Muragaki Y, Chernov M, Maruyama T, Ochiai T, Taira T, Kubo O, Nakamura R, Iseki H, Hori T, Takakura K (2008) Low-grade glioma on stereotactic biopsy: how often is the diagnosis accurate? Minim Invasive Neurosurg 51:275–279
O'Neill KS, Dyer PV, Bell BA, Wilkins PR, Uttley D, Marsh HT (1992) Is peroperative smear cytology necessary for CT-guided stereotaxic biopsy? Br J Neurosurg 6:421–427
Owen CM, Linskey ME (2009) Frame-based stereotaxy in a frameless era: current capabilities, relative role, and the positive- and negative predictive values of blood through the needle. J Neurooncol 93:139–149
Paleologos TS, Dorward NL, Wadley JP, Thomas DG (2001) Clinical validation of true frameless stereotactic biopsy: analysis of the first 125 consecutive cases. Neurosurgery 49:830–835
Pirotte B, Goldman S, Massager N, David P, Wikler D, Vandesteene A, Salmon I, Brotchi J, Levivier M (2004) Comparison of 18F-FDG and 11C-methionine for PET-guided stereotactic brain biopsy of gliomas. J Nucl Med 45:1293–1298
Pirotte BJ, Lubansu A, Massager N, Wikler D, Goldman S, Levivier M (2007) Results of positron emission tomography guidance and reassessment of the utility of and indications for stereotactic biopsy in children with infiltrative brainstem tumors. J Neurosurg 107:392–399
Shastri-Hurst N, Tsegaye M, Robson DK, Lowe JS, Macarthur DC (2006) Stereotactic brain biopsy: an audit of sampling reliability in a clinical case series. Br J Neurosurg 20:222–226
Shooman D, Belli A, Grundy PL (2010) Image-guided frameless stereotactic biopsy without intraoperative neuropathological examination. J Neurosurg. doi:10.3171/2009.12.JNS09573
Smith JS, Quinones-Hinojosa A, Barbaro NM, McDermott MW (2005) Frame-based stereotactic biopsy remains an important diagnostic tool with distinct advantages over frameless stereotactic biopsy. J Neurooncol 73:173–179
Teixeira MJ, Fonoff ET, Mandel M, Alves HL, Rosemberg S (2009) Stereotactic biopsies of brain lesions. Arq Neuropsiquiatr 67:74–77
Tilgner J, Herr M, Ostertag C, Volk B (2005) Validation of intraoperative diagnoses using smear preparations from stereotactic brain biopsies: intraoperative versus final diagnosis–influence of clinical factors. Neurosurgery 56:257–265
Ulm AJ, Bova FJ, Friedman WA (2001) Stereotactic biopsy aided by a computer graphics workstation: experience with 200 consecutive cases. Surg Neurol 56:366–371
Woodworth G, McGirt MJ, Samdani A, Garonzik I, Olivi A, Weingart JD (2005) Accuracy of frameless and frame-based image-guided stereotactic brain biopsy in the diagnosis of glioma: comparison of biopsy and open resection specimen. Neurol Res 27:358–362
Woodworth GF, McGirt MJ, Samdani A, Garonzik I, Olivi A, Weingart JD (2006) Frameless image-guided stereotactic brain biopsy procedure: diagnostic yield, surgical morbidity, and comparison with the frame-based technique. J Neurosurg 104:233–237
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The colleagues of Rotterdam compared the diagnostic yield of frameless stereotactic biopsies with or without the possibility of frozen section and smear preparation assessment during biopsy. The option of asking a neuropathologist to the OR clearly decreased non-diagnostic samples in the final neuropathological evaluation: 1.8% (3 of 164 frameless biopsies 2006-2010) vs. 11% (18 of 160 frameless biopsies 1996-2006). The average numbers of samples were 7.4 vs. 9.0 per patient. Neurosurgeons assessed the macroscopic appearance of the samples as pathologic (oedematous, hemorrhagic, or dark-grayish) - or as normal brain, the only indication for the intra-operative freezesectioning.
The risk of 11% of repeat biopsy and delayed therapy would require reduction – but how?
1. Instant and routine microscopic verification of the presence of representative samples with a putative first diagnosis in the OR – in real life? Neurosurgical units are served by a few neuropathologists at best – often by one or two. Are they willing to walk from their microscopy desks with piles of slide trays to the OR in the other end of the building or in the next one? Few units really have a neuropathologist sitting in the OR until the verification is done.
2. On-demand microscopic assessment in the OR of dubious samples only – as cleverly arranged above.
3. Transfer of fresh samples to the neuropathology unit – and waiting for tens of minutes a phone call from a neuropathologist.
Juha E Jääskeläinen
Kuopio Finland
Financial disclosures and conflicts of interest
The authors have no financial interest in any materials or equipment used in the study.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Dammers, R., Schouten, J.W., Haitsma, I.K. et al. Towards improving the safety and diagnostic yield of stereotactic biopsy in a single centre. Acta Neurochir 152, 1915–1921 (2010). https://doi.org/10.1007/s00701-010-0752-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-010-0752-0