Abstract
Objective
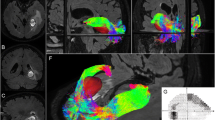
Resection of gliomas invading primary motor cortex and subcortical motor pathway is difficult in both surgical decision-making and functional outcome prediction. In this study, magnetic resonance (MR) diffusion tensor imaging (DTI) data were used to perform tractography to visualize pyramidal tract (PT) along its whole length in a stereoscopic virtual reality (VR) environment. The potential value of its clinical application was evaluated.
Methods
Both three-dimensional (3-D) magnetic resonance imaging (MRI) and DTI datasets were obtained from 45 eligible patients with suspected cerebral gliomas and then transferred to the VR system (Dextroscope; Volume Interactions Pte. Ltd., Singapore). The cortex and tumor were segmented and reconstructed via MRI, respectively, while the tractographic PTs were reconstructed via DTI. All those were presented in a stereoscopic 3-D display synchronously, for the purpose of patient-specific presurgical planning and surgical simulation in each case. The relationship between increasing amplitude of the number of effective fibers of PT (EPT) at affected sides and the patients’ Karnofsky Performance Scale (KPS) at 6 months was addressed out.
Results
In VR presurgical planning for gliomas, surgery was aided by stereoscopic 3-D visualizing the relative position of the PTs and a tumor. There was no significant difference between pre- and postsurgical EPT in this population. A positive relationship was proved between EPT increasing amplitude and 6-month KPS.
Conclusions
3-D stereoscopic visualization of tractography in this VR environment enhances the operators to well understand the anatomic information of intra-axial tumor contours and adjacent PT, results in surgical trajectory optimization initially, and maximal safe tumor resection finally. In accordance to the EPT increasing amplitude, surgeon can predict the long-term motor functional outcome.





Similar content being viewed by others
Abbreviations
- DEC:
-
Directionally encoded color
- DTI:
-
Diffusion tensor imaging
- EPT:
-
Effective fibers of pyramidal tract
- fMRI:
-
Functional magnetic resonance imaging
- HGG:
-
High-grade glioma
- KPS:
-
Karnofsky Performance Scale
- LGG:
-
Low-grade glioma
- MRI:
-
Magnetic resonance imaging
- PT:
-
Pyramidal tract
- ROI:
-
Region of interest
- VR:
-
Virtual reality
References
Berman JI, Berger MS, Chung SW, Nagarajan SS, Henry RG (2007) Accuracy of diffusion tensor magnetic resonance imaging tractography assessed using intraoperative subcortical stimulation mapping and magnetic source imaging. J Neurosurg 107:488–494
Chen X, Weigel D, Ganslandt O, Fahlbusch R, Buchfelder M, Nimsky C (2007) Diffusion tensor-based fiber tracking and intraoperative neuronavigation for the resection of a brainstem cavernous angioma. Surg Neurol 68:285–291, discussion 291
Ciccarelli O, Parker GJ, Toosy AT, Wheeler-Kingshott CA, Barker GJ, Boulby PA, Miller DH, Thompson AJ (2003) From diffusion tractography to quantitative white matter tract measures: a reproducibility study. Neuroimage 18:348–359
Clark CA, Barrick TR, Murphy MM, Bell BA (2003) White matter fiber tracking in patients with space-occupying lesions of the brain: a new technique for neurosurgical planning? Neuroimage 20:1601–1608
Cusimano MD (2003) Virtual reality surgery: neurosurgery and the contemporary landscape a three-dimensional interactive virtual dissection model to simulate transpetrous surgical avenues. Neurosurgery 53:1010–1011, Author reply 1011-1012
Dellani PR, Glaser M, Wille PR, Vucurevic G, Stadie A, Bauermann T, Tropine A, Perneczky A, von Wangenheim A, Stoeter P (2007) White matter fiber tracking computation based on diffusion tensor imaging for clinical applications. J Digit Imaging 20:88–97
Golaszewski SM, Zschiegner F, Siedentopf CM, Unterrainer J, Sweeney RA, Eisner W, Lechner-Steinleitner S, Mottaghy FM, Felber S (2002) A new pneumatic vibrator for functional magnetic resonance imaging of the human sensorimotor cortex. Neurosci Lett 324:125–128
Hakyemez B, Kilic E, Uysal S, Akgun M, Yucel K (2003) Functional magnetic resonance imaging in lesions in or near the sensorimotor cortex. Tani Girisim Radyol 9:287–294
Kinoshita M, Yamada K, Hashimoto N, Kato A, Izumoto S, Baba T, Maruno M, Nishimura T, Yoshimine T (2005) Fiber-tracking does not accurately estimate size of fiber bundle in pathological condition: initial neurosurgical experience using neuronavigation and subcortical white matter stimulation. Neuroimage 25:424–429
Kockro RA, Serra L, Tseng-Tsai Y, Chan C, Yih-Yian S, Gim-Guan C, Lee E, Hoe LY, Hern N, Nowinski WL (2000) Planning and simulation of neurosurgery in a virtual reality environment. Neurosurgery 46:118–135, discussion 135-117
Kunnatiranont R, Laothamatas J, Asavaphatiboon S, Worapruckjaru L, Kumkrua C, Kampangtip A (2002) Localization of sensorimotor cortex by using functional magnetic resonance imaging: comparison between finger tapping and palm scratching in normal volunteer. J Med Assoc Thai 85:1264–1272
Leclercq D, Duffau H, Delmaire C, Capelle L, Gatignol P, Ducros M, Chiras J, Lehericy S (2010) Comparison of diffusion tensor imaging tractography of language tracts and intraoperative subcortical stimulations. J Neurosurg 112(3):503–511
Lo CY, Chao YP, Chou KH, Guo WY, Su JL, Lin CP (2007) DTI-based virtual reality system for neurosurgery. Conf Proc IEEE Eng Med Biol Soc 2007:1326–1329
Nimsky C, Ganslandt O, Hastreiter P, Wang R, Benner T, Sorensen AG, Fahlbusch R (2005) Preoperative and intraoperative diffusion tensor imaging-based fiber trackinvg in glioma surgery. Neurosurgery 56:130–137, discussion 138
Nimsky C, Grummich P, Sorensen AG, Fahlbusch R, Ganslandt O (2005) Visualization of the pyramidal tract in glioma surgery by integrating diffusion tensor imaging in functional neuronavigation. Zentralbl Neurochir 66:133–141
Oishi K, Zilles K, Amunts K, Faria A, Jiang H, Li X, Akhter K, Hua K, Woods R, Toga AW, Pike GB, Rosa-Neto P, Evans A, Zhang J, Huang H, Miller MI, van Zijl PC, Mazziotta J, Mori S (2008) Human brain white matter atlas: identification and assignment of common anatomical structures in superficial white matter. Neuroimage 43:447–457
Okada T, Mikuni N, Miki Y, Kikuta K, Urayama S, Hanakawa T, Fushimi Y, Yamamoto A, Kanagaki M, Fukuyama H, Hashimoto N, Togashi K (2006) Corticospinal tract localization: integration of diffusion-tensor tractography at 3-T MR imaging with intraoperative white matter stimulation mapping—preliminary results. Radiology 240:849–857
Paternostro-Sluga T, Grim-Stieger M, Posch M, Schuhfried O, Vacariu G, Mittermaier C, Bittner C, Fialka-Moser V (2008) Reliability and validity of the Medical Research Council (MRC) scale and a modified scale for testing muscle strength in patients with radial palsy. J Rehabil Med 40:665–671
Qiu TM, Zhang Y, Wu JS (2008) Preliminary application of pyramidal tractography in evaluating prognosis of patients with hypertensive intracerebral hemorrhage. Acta Neurochir Suppl 105:165–170
Spicer MA, Apuzzo ML (2003) Virtual reality surgery: neurosurgery and the contemporary landscape. Neurosurgery 52:489–497, discussion 496-487
Spicer MA, van Velsen M, Caffrey JP, Apuzzo ML (2004) Virtual reality neurosurgery: a simulator blueprint. Neurosurgery 54:783–797, discussion 797-788
Stadie AT, Kockro RA, Reisch R, Tropine A, Boor S, Stoeter P, Perneczky A (2008) Virtual reality system for planning minimally invasive neurosurgery. Technical note. J Neurosurg 108:382–394
Stadlbauer A, Nimsky C, Buslei R, Salomonowitz E, Hammen T, Buchfelder M, Moser E, Ernst-Stecken A, Ganslandt O (2007) Diffusion tensor imaging and optimized fiber tracking in glioma patients: histopathologic evaluation of tumor-invaded white matter structures. Neuroimage 34:949–956
Stadlbauer A, Polking E, Prante O, Nimsky C, Buchfelder M, Kuwert T, Linke R, Doelken M, Ganslandt O (2009) Detection of tumour invasion into the pyramidal tract in glioma patients with sensorimotor deficits by correlation of (18)F-fluoroethyl-L-tyrosine PET and magnetic resonance diffusion tensor imaging. Acta Neurochir (Wien) 151:1061–1069
Sullivan EV, Rohlfing T, Pfefferbaum A (2008) Quantitative fiber tracking of lateral and interhemispheric white matter systems in normal aging: relations to timed performance. Neurobiol Aging 31(3):464–481
Sunaert S (2006) Presurgical planning for tumor resectioning. J Magn Reson Imaging 23:887–905
Tronnier VM, Staubert A, Bonsanto MM, Wirtz CR, Kunze S (2000) Virtual reality in neurosurgery. Radiologe 40:211–217
Wakana S, Caprihan A, Panzenboeck MM, Fallon JH, Perry M, Gollub RL, Hua K, Zhang J, Jiang H, Dubey P, Blitz A, van Zijl P, Mori S (2007) Reproducibility of quantitative tractography methods applied to cerebral white matter. Neuroimage 36:630–644
Wong GK, Zhu CX, Ahuja AT, Poon WS (2007) Craniotomy and clipping of intracranial aneurysm in a stereoscopic virtual reality environment. Neurosurgery 61:564–568, discussion 568-569
Wu JS, Zhou LF, Tang WJ, Mao Y, Hu J, Song YY, Hong XN, Du GH (2007) Clinical evaluation and follow-up outcome of diffusion tensor imaging-based functional neuronavigation: a prospective, controlled study in patients with gliomas involving pyramidal tracts. Neurosurgery 61:935–948, discussion 948-939
Yc Goha K (2005) Virtual reality applications in neurosurgery. Conf Proc IEEE Eng Med Biol Soc 4:4171–4173
Yi ZQ, Li L, Mo DP, Zhang JY, Zhang Y, Bao SD (2008) Preoperative surgical planning and simulation of complex cranial base tumors in virtual reality. Chin Med J (Engl) 121:1134–1136
Zhang W, Olivi A, Hertig SJ, van Zijl P, Mori S (2008) Automated fiber tracking of human brain white matter using diffusion tensor imaging. Neuroimage 42:771–777
Zhao X, Wang M, Gao W, Liu H (2005) White matter fiber tracking method by vector interpolation with diffusion tensor imaging data in human brain. Conf Proc IEEE Eng Med Biol Soc 6:5786–5789
Acknowledgments
We sincerely thank Mr. Jian-bing Shi for technical support in the MRI manipulation. This project was sponsored by the Ministry of Health of China (2007–2009) and Shanghai government, P. R. China (NO. 07QA14008).
Statement of authorship
This prospective clinical study was approved by local ethics committee before commencing.
Disclosure
We have no personal financial interest regarding the DTI-based Virtual Reality System described in this paper. None of the authors has received any funding from Dextroscope, Volume Interactions.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Comment
This article demonstrates the use the authors have found for preoperative planning and rehearsing of surgery of intra-axial cerebral tumors based on virtual reality technology.These are exciting times for Neurosurgery. Developing technology applied to obtaining information regarding not only shear anatomy of the brain but mostly its inherent functions has significantly impacted with the way surgery for these invasive tumors is conducted.
Most information regarding preoperative location of cerebral function is provided by MRI-based technology. That is the case for DTI, tractography, functional MRI, and all adjuncts being developed from here on.
The Dextroscope is an interesting add-on. It enables us to preoperatively reconstruct the anatomy of the lesion to be approached in relationship to the actual cranial and cerebral anatomy of the patient. What has been done here is to add up the information depicting the anatomy of the white matter tracts of the brain namely the pyramidal tracts. The authors then preoperatively assess the EPTs, that is, the number of fibers actually conveying information in a continuous way along the whole cerebral motor pathway and compare this number before and after surgery. Not unexpectedly, patients who end up with higher EPTs seem to fare better from the motor standpoint.
As the authors point out, there are several limitations to the transposition of this information directly into surgery. Fiber tracking technology is still quite dependent on the mathematic algorithm chosen for its representation. Secondly, there is no way one can depend exclusively on this information during surgery because of the shift produced by the manipulation of the brain and the CSF spaces. This aspect can only be circumvented with the use of intraoperative MRI done with the purpose of reacquiring the same sequences enabling the re-reconstruction of the white matter fibers as surgery goes along. This is still a morose and complex technique, and it was not applied in the current series.
Finally, there is nothing in this technique which enables the surgeon to better differentiate between normal and abnormal tissue and certainly nothing updating him on the level of function of the tissue being manipulated. This can only be pursued with the use of DBS.All in all, this virtual reality technology seems to play an interesting part in teaching residents as well as in helping out surgeons actually plan their best trajectory and strategy for a specific case. However, the same comments which apply to the use of neuronavigation are also appropriate regarding this technology. These techniques demonstrate the immense steps taken to help localize anatomy and function within the brain. Their use is ever so more important if based on a sound and strong traditional apprenticeship of the anatomy of the brain based on repeated laboratory cadaver dissections.
For all the above reasons, I think it is a little far-fetched to try to pass the idea that the use of the Dextroscope separates from intraoperative functional imaging and deep brain simulation is a recommendable solution for patients with this type of tumors. Just out of curiosity I would ask the authors to explain what they think is the application of this technique for aneurysms, as stated in the text.
The authors should consider shortening the length of the text and clearing some of the issues raised above.
Maybe this can be turned into a technical report. As it is I think the article does not add much to previous articles published on the matter and has the risk of conveying the idea that the use of the Dextroscope is a safe way to avoid intraoperative injury to deep eloquent areas of the brain. I think we should wait for possible changes and reconsider then.
Manuel Cunha e Sa
Almada, Portugal
Tian-ming Qiu and Yi Zhang contributed to this paper equally.
Rights and permissions
About this article
Cite this article
Qiu, Tm., Zhang, Y., Wu, JS. et al. Virtual reality presurgical planning for cerebral gliomas adjacent to motor pathways in an integrated 3-D stereoscopic visualization of structural MRI and DTI tractography. Acta Neurochir 152, 1847–1857 (2010). https://doi.org/10.1007/s00701-010-0739-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-010-0739-x