Abstract
Background
Peripheral nerve lesions usually are associated with neuropathic pain. In the present paper, we describe a simple scale to quantify pain after brachial plexus injuries and apply this scale to a series of patients to determine initial outcomes after reconstructive surgery.
Methods
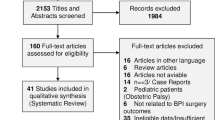
Fifty-one patients with traumatic brachial plexus avulsion injuries were treated over the period of one calendar year at one center by the same surgical team. Of these, 28 patients who were available for follow-up reported some degree of neuropathic pain radiating towards the hand or forearm and underwent reconstructive microsurgery and direct pain management, including trunk and nerve neurolysis and repair. A special pain severity rating scale was developed and used to assess patients' pain before and after surgery, over a minimum follow-up of 6 months. An independent researcher, not part of the surgical team, performed all pre- and postoperative evaluations.
Findings
Of the 28 patients with brachial plexus traction injuries who met eligibility criteria, 93% were male, and most were young (mean age, 27.6 years). The mean preoperative severity of pain using our scale was 30.9 out of a maximum of 37 (±0.76 SD), which fell to a mean of 6.9 (±0.68 SD) 6 months post-procedure. On average, pain declined by 78% across the whole series, a decline that was statistically significant (p < .001). Subset analysis revealed similar improvements across all the different parameters of pain.
Conclusions
We have designed and tested a simple and reliable method by which to quantify neuropathic pain after traumatic brachial plexus injuries. Initial surgical treatment of the paralysis—including nerve, trunk and root reconstruction, and neurolysis—comprises an effective means by which to initially treat neuropathic pain. Ablative or neuromodulative procedures, like dorsal root entry zone, should be reserved for refractory cases.

Similar content being viewed by others
References
Berman J, Anand P, Chen L, Taggart M, Birch R (1996) Pain relief from preganglionic injury to the brachial plexus by late intercostal nerve transfer. J Bone Jt Surg Br 78(5):759–760
Bertelli J, Ghizoni MF (2008) Pain after avulsion injuries and complete palsy of the brachial plexus: the possible role of nonavulsed roots in pain generation. Neurosurg 62(5):1104–1113
Burchiel KJ, Johans TJ, Ochoa J (1993) Painful nerve injuries: bridging the gap between basic neuroscience and neurosurgical treatment. Acta Neurochir Suppl (Wien) 58:131–135
Burchiel KJ, Ochoa JL (1991) Surgical management of post-traumatic neuropathic pain. Neurosurg Clin N Am 2(1):117–126
Friedman AH, Nashold BS Jr, Bronec PR (1988) Dorsal root entry zone lesions for the treatment of brachial plexus avulsion injuries: a follow-up study. Neurosurgery 22(2):369–373
Kline DG, Tasker RR (2008) Pain of nerve origin. In: Kim DH, Midha R, Murovic JA, Spinner RJ (eds) Kline & Hudson's nerve injuries, 2nd edn. Saunders, New York
Laryea J, Schon L, Belzberg A (2001) Peripheral nerve stimulators for pain control. Semin Neurosurg 12(1):125–131
Midha R, Zager EL (2008) Surgery of the peripheral nerves: a case-based approach, 1st edn. Thieme, New York
Nashold BS (1984) Current status of the DREZ operation. Neurosurgery 15:942–944
Parry CB (1984) Pain in avulsion of the brachial plexus. Neurosurgery 15:960–965
Samii M, Bear-Henney S, Lüdemann W, Tatagiba M, Blömer U (2001) Treatment of refractory pain after brachial plexus avulsion with dorsal root entry zone lesions. Neurosurgery 48(6):1269–1275, discussion 1275–1277
Sindou M, Blondet E, Emery E (2005) Microsurgical lesioning in the dorsal root entry zone for pain due to brachial plexus avulsion: a prospective series of 55 patients. J Neurosurg 102:1018–1028
Socolovsky M (2003) Conceptos actuales en la cirugía de los nervios periféricos: parte I: lesiones del plexo braquial. Rev Arg Neurocir 17(2):53–58
Taggart M (1998) Rehabilitation. In: Birch R, Bonney G, Wynn Parry CB (eds) Surgical disorders of the peripheral nerves, 1st edn. Churchill Livingstone, Edinburgh, pp 461–463
Teixeira MJ, De Souza EC, Yeng LT, Pereira WC (1999) Lesion of the Lissauer tract and of the posterior horn of the gray substance of the spinal cord and the electrical stimulation of the central nervous system for the treatment of brachial plexus avulsion pain. Arq Neuro-Psiquiatr 57(1):56–62
Thomas D, Kitchen ND (1994) Long term follow-up of dorsal root entry zone lesions in plexus avulsion. J Neurol Neurosurg Psychiatry 57:737–738
Conflicts of interest
The authors declare that they have no conflicts of interest related to the present study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonilla, G., Di Masi, G., Battaglia, D. et al. Pain and brachial plexus lesions: evaluation of initial outcomes after reconstructive microsurgery and validation of a new pain severity scale. Acta Neurochir 153, 171–176 (2011). https://doi.org/10.1007/s00701-010-0709-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-010-0709-3