Abstract
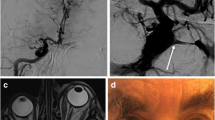
Intracranial endovascular procedures are less invasive and relatively safe; however, these procedures do carry a risk of complications, such as thromboembolization, arterial injury, and vessel occlusion. We present a case of carotid-cavernous fistula development secondary to injury of the cavernous segment of the internal carotid artery (ICA) during stent angioplasty and its treatment by transarterial coil embolization. Probable causes of this complication and its treatment method are discussed. To the best of our knowledge, this is the first report of such a case.




Similar content being viewed by others
References
Ahn JY, Lee BH, Joo JY (2003) Stent-assisted Guglielmi detachable coils embolisation for the treatment of a traumatic carotid cavernous fistula. J Clin Neurosci 10:96–98
Chaer RA, Trocciola S, DeRubertis B, Lin SC, Kent KC, Faries PL (2006) Cerebral ischemia associated with PercuSurge balloon occlusion balloon during carotid stenting: Incidence and possible mechanisms. J Vasc Surg 43:946–952 discussion 952
Chiam PT, Samuelson RM, Mocco J, Hanel RA, Siddiqui AH, Hopkins LN, Levy EI (2008) Navigability trumps all: stenting of acute middle cerebral artery occlusions with a new self-expandable stent. AJNR Am J Neuroradiol
Eddleman CS, Surdell D, Miller J, Shaibani A, Bendok BR (2007) Endovascular management of a ruptured cavernous carotid artery aneurysm associated with a carotid cavernous fistula with an intracranial self-expanding microstent and hydrogel-coated coil embolization: case report and review of the literature. Surg Neurol 68:562–567
Friedman JA, Kallmes DF, Wijdicks EF (2004) Thalamic hemorrhage following carotid angioplasty and stenting. Neuroradiology 46:399–403
Georganos SA, Guilbert F, Salazkin I, Gevry G, Raymond J (2004) Surgical construction of an in vivo carotid siphon model to test neurovascular devices. Neurosurgery 54:1239–1243 discussion 1243
Kim JK, Ahn JY, Lee BH, Chung YS, Chung SS, Kim OJ, Kim WC, Joo JY (2004) Elective stenting for symptomatic middle cerebral artery stenosis presenting as transient ischaemic deficits or stroke attacks: short term arteriographical and clinical outcome. J Neurol Neurosurg Psychiatry 75:847–851
Kim SH, Qureshi AI, Boulos AS, Bendok BR, Levy EL, Yahia AM, Guterman LR, Hopkins LN (2003) Intracranial stent placement for the treatment of a carotid-cavernous fistula associated with intracranial angioplasty. Case report. J Neurosurg 98:1116–1119
Kocer N, Kizilkilic O, Albayram S, Adaletli I, Kantarci F, Islak C (2002) Treatment of iatrogenic internal carotid artery laceration and carotid cavernous fistula with endovascular stent-graft placement. AJNR Am J Neuroradiol 23:442–446
Koyanagi M, Nishi S, Hattori I, Horikawa F, Iwasaki K (2004) Stent-supported coil embolization for carotid artery pseudoaneurysm as a complication of endovascular surgery—case report. Neurol Med Chir (Tokyo) 44:544–547
Layton KF, Hise JH, Thacker IC (2008) Recurrent intracranial stenosis induced by the Wingspan stent: comparison with balloon angioplasty alone in a single patient. AJNR Am J Neuroradiol 29:1050–1052
Lopez-Quinones M, Bargallo X, Blasco J, Real MI, Gonzalez S, Bunesch L, Gilabert R (2006) Iatrogenic carotid-jugular arteriovenous fistula: color Doppler sonographic findings and treatment with covered stent. J Clin Ultrasound 34:301–305
Macdonald S (2007) Brain injury secondary to carotid intervention. J Endovasc Ther 14:219–231
Men S, Ozturk H, Hekimoglu B, Sekerci Z (2003) Traumatic carotid-cavernous fistula treated by combined transarterial and transvenous coil embolization and associated cavernous internal carotid artery dissection treated with stent placement. Case report. J Neurosurg 99:584–586
Mollers MO, Reith W (2004) Intracranial arteriovenous fistula caused by endovascular stent-grafting and dilatation. Neuroradiology 46:323–325
Moron FE, Klucznik RP, Mawad ME, Strother CM (2005) Endovascular treatment of high-flow carotid cavernous fistulas by stent-assisted coil placement. AJNR Am J Neuroradiol 26:1399–1404
Nicita-Mauro V, Maltese G, Nicita-Mauro C, Basile G (2007) Vascular aging and geriatric patient. Minerva Cardioangiol 55:497–502
Serbinenko FA (1971) Occlusion of the cavernous portion of the carotid artery with a balloon as a method of treating carotid-cavernous anastomosis. Vopr Neirokhir 35:3–9
Terada T, Tsuura M, Matsumoto H, Masuo O, Tsumoto T, Yamaga H, Ohura Y, Itakura T (2006) Hemorrhagic complications after endovascular therapy for atherosclerotic intracranial arterial stenoses. Neurosurgery 59:310–318 discussion 310–318
Theron J, Guimaraens L, Coskun O, Sola T, Martin JB, Rufenacht DA (1998) Complications of carotid angioplasty and stenting. Neurosurg Focus 5:e4
Vanninen RL, Manninen HI, Rinne J (2003) Intrasellar latrogenic carotid pseudoaneurysm: endovascular treatment with a polytetrafluoroethylene-covered stent. Cardiovasc Intervent Radiol 26:298–301
Zaidat OO, Wolfe T, Hussain SI, Lynch JR, Gupta R, Delap J, Torbey MT, Fitzsimmons BF (2008) Interventional acute ischemic stroke therapy with intracranial self-expanding stent. Stroke 39:2392–2395
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
This paper reports an imaginative and technically challenging case describing an endovascular approach in which a high-flow CCF was closed by using detachable coils that were introduced into the cavernous sinus from a venous and an arterial approach, while preserving the ICA and restoring the normal hemispheric ICA flow. Most interestingly, none of this was originally planned, but rather executed “à la Carte” to sequentially solve ensuing problems. However, contrary to the authors claim, there have been several case reports of patients with direct CCFs as a result of iatrogenic internal carotid artery laceration associated with intracranial angioplasty [1–3] or after transsphenoidal surgery for pituitary adenoma [4, 5] treated by stent placement and stent-assisted coiling placement.
After the analysis of the morphology of the fistula, we believe that the complication derived from both stent-related problems (the use of a coronary stent, stent oversize and stiffness, which may result in arterial rupture) and patient-related problems (calcification, plaque rupture and tortuousness of ICA due to age). As one might conclude in this case, identification of appropriate candidates for treatment remains a challenge. Collaterally, would the authors systematically advise a brain CT angiogram as a pre-treatment work-up tool in older patients to find out ICA calcifications?
Additionally, an accurate measure of the size of the ICA is essential, because this allows a correct choice of the size of the stent to be deployed. It is known that a high-pressure inflation is often performed in coronary stent placement to optimize the stent apposition to the arterial wall. However, in the case of intracranial vessels, the potential risk of rupture from high-pressure inflations may be greater due to a lack of surrounding supportive tissue in the subarachnoid space. But, considering the risk of vessel-wall rupture, the maximal pressure in the balloon may not be as important as the rate of inflation. The question of what constitutes a safe inflation pressure and rate in the intracranial vessels is an important one. Equally, with balloon-expandable stents, as used in this patient, adequate predilatation of the vessel may be crucial. Predilatation prepares a route of atraumatic passage for the balloon-mounted stent and reduces the resistance to expansion of the stent during inflation. Vascular biomechanics are important to define differences between cerebral arteries and extracranial vessels and partly explain the technical challenges facing cerebral artery revascularization compared with revascularization of coronary arteries. In terms of a safe high-flow fistula embolisation, it may be important to consider the use of a balloon that could be insufflated inside the stent to prevent coils from herniating through open cells of the stent into the parent artery. These are issues that are open to discussion.
Finally, the authors could have commented on the newly available covered, or self-expanding stents as a conceptual idea to surmount these complications in the future, and perhaps compare this case with their center’s experience with the new intracranial devices. We agree that covered stents may be technically difficult to deliver, especially in elderly patients with tortuous vessels, as it was the case here.
Overall, this paper raises the question of the intracranial use of coronary stent. Stents are very useful devices that allow initial reconstruction of the damaged segment of the ICA and then controlled coil deposition into the cavernous sinus in CCF. Balloon-expandable coronary stents used “off-label” or with modified coronary devices in approval studies showed a wide range of complication rates and variable short-term follow-up results and raised doubts concerning the clinical effectiveness of the treatment [6–10].
References
1. Weber W, Henkes H, Berg-Dammer E, Esser J, Kuhne D. (2001) Cure of a direct carotid cavernous fistula by endovascular stent deployment. Cerebrovasc Dis 12:272–275
2. Kim SH, Qureshi AI, Boulos AS et al (2003) Intracranial stent placement for the treatment of a carotid-cavernous fistula associated with intracranial angioplasty: case report. J Neurosurg 98:1116–119
3. Mollers MO, Reith W.(2004) Intracranial arteriovenous fistula caused by endovascular stent-grafting and dilatation. Neuroradiology 46: 323–325
4. Kocer N, Kizilkilic O, Albayram S, Adelatli I, Kantarci F, Islak C (2002) Treatment of iatrogenic internal carotid artery laceration and carotid cavernous fistula with endovascular stent-graft placement. AJNR Am J Neuroradiol 23:442–446
5. Vannien RL, Manninen HI, Rinne J (2003) Intrasellar latrogenic carotid pseudoaneurysm: endovascular treatment with a polytetrafluoroethylene-covered stent. Cardiovasc Intervent Radiol 26:298–301
6. SSYLVIA Study Investigators (2004) Stenting of Symptomatic Atherosclerotic Lesions in the Vertebral or Intracranial Arteries (SSYLVIA): study results. Stroke 35:1388–1392
7. du Mesnil de Rochemont, Turowski B, Buchkremer M, Sitzer M, Zanella FE, Berkefeld J (2004) Recurrent symptomatic high-grade intracranial stenoses: safety and efficacy of undersized stents—initial experience. Radiology 231:45–49
8. Weber W, Mayer TE, Henkes H, Kis B, Hamann GF, Schulte-Altedornenburg G, Brückmann H, Kuehne D (2005) Stentangioplasty of intracranial vertebral and basilar artery stenoses in symptomatic patients. Eur J Radiol 55:231–236
9. Yu W, Smith WS, Singh V, Ko NU, Cullen SP, Dowd CF, Halbach VV, Higashida RT (2005) Long-term outcome of endovascular stenting for symptomatic basilar artery stenosis. Neurology 64:1055–1057
10. Chow MM, Masaryk TJ, Woo HH, Mayberg MR, Rasmussen PA (2005) Stent-assisted angioplasty of intracranial vertebrobasilar atherosclerosis: midterm analysis of clinical and radiologic predictors of neurological morbidity and mortality. AJNR Am J Neuroradiol 26(4):869–874
Oscar L. Alves
Portugal
Rights and permissions
About this article
Cite this article
Yoon, W.K., Kim, Y.W., Kim, S.R. et al. Transarterial coil embolization of a carotid-cavernous fistula which occurred during stent angioplasty. Acta Neurochir 151, 849–854 (2009). https://doi.org/10.1007/s00701-009-0351-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-009-0351-0