Abstract
Background
Temporary occlusion of an intracranial artery during microvascular anastomosis is a major risk factor in cerebrovascular surgery. A new laser vascular welding technique that minimizes the occlusion time of the recipient vessel has been developed and is described in this report.
Method
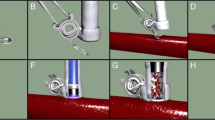
A new minimally occlusive technique of end-to-side microvascular anastomosis was developed employing a diode laser in association with the application of a chromophore in our experimental model of double end-to-side anastomosis. The implantation of a vein graft on the patent carotid artery was obtained through the application of three interrupted sutures at each anastomotic site; the carotid was then clamped, two arteriotomies were performed, followed by the application of a fourth suture and of the laser welding procedure on each anastomosis. Monitoring of the temperature at the site of the anastomosis was introduced in order to control the welding technique.
Findings
The time of the clamping of the carotid artery was 12 min to perform two end-to-side anastomoses (i.e., 6 min for each anastomosis). All bypasses were patent after a follow-up of 90 days and histological study confirmed good preservation of the vascular wall.
Conclusions
Our laser-assisted technique of vascular anastomosis reduces the duration of the clamping of the recipient artery down to 6 min. This technique can minimize the risk of cerebral ischemia associated with occlusion of a recipient artery in intracranial bypass procedures, promoting an improved vascular healing process with a lower risk of thrombosis and occlusion.









Similar content being viewed by others
References
Bass LS, Treat MR (1995) Laser tissue welding: a comprehensive review of current and future clinical applications. Lasers Surg Med 17:315–349. doi:10.1002/lsm.1900170402
Bremmer JP, Verweij BH, Van der Zwan A, Reinert MM, Mansvelt Beck HJ, Tulleken CAF (2007) Sutureless nonocclusive bypass surgery in combination with an expanded polytetrafluoroethylene graft. Laboratory investigation. J Neurosurg 107:1190–1197. doi:10.3171/JNS-07/12/1190
Gelli R, Pini R, Toncelli F, Chiarugi C, Reali UM (1997) Vessel wall recovery after diode laser assisted microvascular anastomosis: Clinical and histological analysis on long term follow-up. J Reconstr Microsurg 13:199–205. doi:10.1055/s-2007-1006405
McNally-Heintzelman KM (2003) Laser tissue welding. In: Vo-Dinh T (ed) Biomedical photonics handbook. CRC Press, Boca Raton, pp 39–45
Phillips AB, Ginsburg BY, Shin SJ, Soslow R, Ko W, Poppas DP (1999) Laser welding for vascular anastomosis using albumin solder: an approach for MIDCAB. Lasers Surg Med 24:264–268. doi:10.1002/(SICI)1096-9101(1999)24:4<264::AID-LSM3>3.0.CO;2-#
Puca A, Albanese A, Esposito G, Maira G, Tirpakova B, Rossi G, Mannocci A, Pini R (2006) Diode laser-assisted carotid bypass surgery: an experimental study with morphological and immunohistochemical evaluations. Neurosurgery 59:1286–1294. doi:10.1227/01.NEU.0000249217.27214.EC
Rossi F, Pini R, Menabuoni L (2007) Experimental and model analysis on the temperature dynamics during diode laser welding of the cornea. J Biomed Opt 12:014031. doi:10.1117/1.2437156
Streefkerk HJ, Van der Zwan A, Verdaasdonk RM, Beck HJ, Tulleken CA (2003) Cerebral revascularization. Adv Tech Stand Neurosurg 28:145–225
Tulleken CAF, Van der Zwan A, Van Rooij WJ, Pareira Ramos LM (1998) High-flow bypass using nonocclusive excimer laser-assisted end-to-side anastomosis of the external carotid artery to the P1 segment of the posterior cerebral artery via the sylvian route. Technical note. J Neurosurg 88:925–927
Zeebregts CJ, Heijmen RH, van den Dungen JJ, van Schilfgaarde R (2003) Non-suture methods of vascular anastomosis. Br J Surg 90:261–271. doi:10.1002/bjs.4063
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
In this interesting, well-planned, effectively executed, and well written in vivo experimental study in a rabbit model of the two-end-to-side anastomoses, the authors continued their interest in using a low-power laser to perform carotid bypass. The goal of the study was to examine the efficacy and safety of the laser-welding technique to establish anastomoses between a jugular vein graft and the carotid artery. The authors found that their technique was not only efficient and safe, but also significantly decreased the time of carotid artery occlusion. The results were presented clearly and convincingly and were supported by properly chosen figures. The discussion was concise and informative. In summary, it is an interesting study that presents a new tool for vascular surgery.
R.M. Pluta
NIH Bethesda, MD, USA
Rights and permissions
About this article
Cite this article
Puca, A., Esposito, G., Albanese, A. et al. Minimally occlusive laser vascular anastomosis (MOLVA): experimental study. Acta Neurochir 151, 363–368 (2009). https://doi.org/10.1007/s00701-009-0219-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-009-0219-3