Abstract
Purpose
To evaluate the predictors of a difficult Pringle maneuver (PM) in laparoscopic liver resection (LLR) and to assess alternative procedures to PM.
Methods
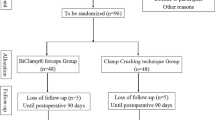
Data from patients undergoing LLR between 2013 and 2020 were reviewed retrospectively. Univariate and multivariate analyses were performed and the outcomes of patients who underwent PM or alternative procedures were compared.
Results
Among 106 patients who underwent LLR, PM could not be performed in 18 (17.0%) because of abdominal adhesions in 14 (77.8%) and/or collateral flow around the hepatoduodenal ligament in 5 (27.8%). Multivariate analysis revealed that Child–Pugh classification B (p = 0.034) and previous liver resection (p < 0.001) were independently associated with difficulty in performing PM in LLR. We evaluated pre-coagulation of liver tissue using microwave tissue coagulators, saline irrigation monopolar, clamping of the hepatoduodenal ligament using an intestinal clip, and hand-assisted laparoscopic surgery as alternatives procedures to PM. There were no significant differences in blood loss (p = 0.391) or transfusion (p = 0.518) between the PM and alternative procedures.
Conclusions
Child–Pugh classification B and previous liver resection were identified as predictors of a difficult PM in LLR. The alternative procedures were found to be effective.



Similar content being viewed by others
Change history
09 August 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00595-022-02572-x
References
Kaneko H, Otsuka Y, Kubota Y, Wakabayashi G. Evolution and revolution of laparoscopic liver resection in Japan. Ann Gastroenterol Surg. 2017;1:33–43.
Otsuka Y, Tsuchiya M, Maeda T, Katagiri T, Isii J, Tamura A, Yamazaki K, et al. Laparoscopic hepatectomy for liver tumors: proposals for standardization. JHPBS. 2009;16:720–5.
Ciria R, Cherqui D, Geller DA, Briceno J, Wakabayashi G. Comparative short-term benefits of laparoscopic liver resection: 9000 cases and climbing. Ann Surg. 2016;263:761–77.
Abu Hilal M, Aldrighetti L, Dagher I, Edwin B, Ivan Troisi R, Alikhanov R, et al. The Southampton Consensus Guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg. 2018;268:11–8.
Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection–2,804 patients. Ann Surg. 2009;250:831–41.
Cho JY, Han HS, Wakabayashi G, Soubrane O, Geller D, O’Rourke N, et al. Practical guidelines for performing laparoscopic liver resection based on the second international laparoscopic liver consensus conference. Surg Oncol. 2018;27:A5-9.
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261:619–29.
Otsuka Y, Kaneko H, Cleary SP, Buell JF, Cai X, et al. What is the best technique in parenchymal transection in laparoscopic liver resection? Comprehensive review for the clinical question on the 2nd international consensus conference on laparoscopic liver resection. J Hepatobiliary Pancreat Sci. 2015;22:363–70.
Viganò L, Laurent A, Tayar C, Tomatis M, Ponti A, Cherqui D. The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg. 2009;250:772–82.
Gigot J, Glineur D, Santiago Azagra J, Goergen M, Ceuterick M, Morino M, et al. Hepatobiliary and pancreatic section of the royal Belgian society of surgery and the Belgian group for endoscopic surgery. Laparoscopic liver resection for malignant liver tumors: preliminary results of a multicenter European study. Ann Surg. 2002;236:90–7.
Ercolani G, Ravaioli M, Grazi GL, Cescon M, Del Gaudio M, Vetrone G, et al. Use of vascular clamping in hepatic surgery: lessons learned from 1260 liver resections. Arch Surg. 2008;143:380–7.
Elias D, Lasser P, Debaene B, Doidy L, Billard V, Spencer A, et al. Intermittent vascular exclusion of the liver (without vena cava clamping) during major hepatectomy. Br J Surg. 1995;82:1535–9.
Weiss MJ, Ito H, Araujo RL, Zabor EC, Gonen M, D’Angelica MI, et al. Hepatic pedicle clamping during hepatic resection for colorectal liver metastases: no impact on survival or hepatic recurrence. Ann Surg Oncol. 2013;20:285–94.
Gurusamy KS, Sheth H, Kumar Y, Sharma D, Davidson BR. Methods of vascular occlusion for elective liver resections. Cochrane Database Syst Rev. 2009;1:CD007632.
Komeda K, Hayashi M, Inoue Y, Shimizu T, Asakuma M, Hirokawa F, et al. Clinical usefulness of endo intestinal clips during Pringle’s maneuver in laparoscopic liver resection: a technical report. Surg Laparosc Endosc Percutan Tech. 2013;23:e103–5.
Dua MM, Worhunsky DJ, Hwa K, Poultsides GA, Norton JA, Visser BC. Extracorporeal Pringle for laparoscopic liver resection. Surg Endosc. 2015;29:1348–55.
Kaneko H, Tsuchiya M, Otsuka Y, Yajima S, Minagawa T, Watanabe M, et al. Laparoscopic hepatectomy for hepatocellular carcinoma in cirrhotic patients. J Hepatobiliary Pancreat Surg. 2009;16:433–8.
Wakabayashi T, Felli E, Memeo R, Mascagni P, Abe Y, Kitagawa Y, et al. Short-term outcomes of laparoscopic repeat liver resection after open liver resection: a systematic review. Surg Endosc. 2019;33:2083–92.
Uchida H, Yukio Iwashita Y, Saga K, Takayama H, Watanabe K, Endo Y, et al. Benefit of laparoscopic liver resection in high body mass index patients. World J Gastroenterol. 2016;22:3015–22.
Kubota Y, Otsuka Y, Tsuchiya M, Katagiri T, Ishii J, Maeda T, et al. Efficacy of laparoscopic liver resection in colorectal liver metastases and the influence of preoperative chemotherapy. World J Surg Oncol. 2014;12:351.
Kaneko H, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, Yamazaki K. Application of devices for safe laparoscopic hepatectomy. HPB. 2008;10:219–24.
Yamanaka N, Okamoto E, Oriyama T, Fujimoto J, Furukawa K, Kawamura E, et al. A prediction scoring system to select the surgical treatment of liver cancer. Further refinement based on 10 years of use. Ann Surg. 1994;219:342–6.
Tokunaga Y, Sasaki H, Matsueda S, Kawasahi T, Saito T. Clinical role of laparoscopic hepatectomy using vessel sealer and soft coagulation for small hepatic tumors suspected of malignancy. Hepatogastroenterology. 2009;56:1714–8.
Wakabayashi G. What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? Hepatobiliary Surg Nutr. 2016;5:281–9.
Van der Poel MJ, Barkhatov L, Fuks D, Berardi G, Cipriani F, Aljaiuossi A, et al. Multicentre propensity score-matched study of laparoscopic versus open repeat liver resection for colorectal liver metastases. Br J Surg. 2019;106:783–9.
Gutt CN, Oniu T, Schemmer P, Mehrabi A, Buchler MW. Fewer adhesions induced by laparoscopic surgery? Surg Endosc. 2004;18:898–906.
Belli G, Cioffi L, Fantini C, D’Agostino A, Russo G, Limongelli P, et al. Laparoscopic redo surgery for recurrent hepatocellular carcinoma in cirrhotic patients: feasibility, safety, and results. Surg Endosc. 2009;23:1807–11.
Gon H, Kido M, Tanaka M, Kuramitsu K, Komatsu S, Awazu M, et al. Laparoscopic repeat hepatectomy is a more favorable treatment than open repeat hepatectomy for contralateral recurrent hepatocellular carcinoma cases. Surg Endosc. 2021;35:2896–906.
Vizzutti F, Arena U, Romanelli RG, Rega L, Foschi M, Colagrande S, et al. Liver stiffness measurement predicts severe portal hypertension in patients with HCV-related cirrhosis. Hepatology. 2007;45:1290–7.
Thabut D, Bureau C, Layese R, Bourcier V, Hammouche M, Cagnot C, Marcellin P, et al. Validation of Baveno VI criteria for screening and surveillance of esophageal varices in patients with compensated cirrhosis and a sustained response to antiviral therapy. Gastroenterology. 2019;156(4):997–1009.
Huang M, Lee W, Wang W, Wei PL, Chen RJ. Hand-assisted laparoscopic hepatectomy for solid tumor in the posterior portion of the right lobe: initial experience. Ann Surg. 2003;238:674–9.
Kim S, Lim S, Ha Y, et al. Laparoscopic-assisted combined colon and liver resection for primary colorectal cancer with synchronous liver metastases: initial experience. World J Surg. 2008;32:2701–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original publication was revised due to errors in affilations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nakada, S., Otsuka, Y., Ishii, J. et al. Predictors of a difficult Pringle maneuver in laparoscopic liver resection and evaluation of alternative procedures to assist bleeding control. Surg Today 52, 1688–1697 (2022). https://doi.org/10.1007/s00595-022-02538-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02538-z