Abstract
Purpose
Inflammation-, nutrition-, and liver fibrosis-related markers are recognized as prognostic for hepatocellular carcinoma (HCC) patients. This study, therefore, assessed the preoperative prognostic utility of the combination of these markers in patients with HCC.
Methods
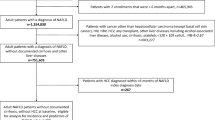
This single-center retrospective study included patients who underwent hepatic resection for HCC between 2004 and 2017. A total of 454 patients were divided into training (n = 334) and validation (n = 120) cohorts by random sampling. The predictive impact on surgical outcomes was evaluated using receiver operating characteristic (ROC) curves of these prognostic values in the training cohort.
Results
The prognostic nutritional index (PNI) and aspartate aminotransferase-to-platelet ratio index (APRI) were the strongest diagnostic values (areas under the ROC curves: 0.627 and 0.646, respectively). A scoring system (over 0–2 points) was developed using optimal cutoff values (for PNI < 46.5 scored as 1 point; for APRI > 0.98 scored as 1 point). An increased PNI-APRI score was an independent prognostic factor for both the overall and disease-free survival in HCC patients. Finally, the clinical feasibility of the PNI-APRI score was confirmed in the validation cohort.
Conclusions
The PNI-APRI score is a useful marker for predicting surgical outcomes of HCC patients.



Similar content being viewed by others
Abbreviations
- AFP:
-
Alpha-fetoprotein
- ALT:
-
Alanine aminotransferase
- APRI:
-
Aspartate aminotransferase-to-platelet ratio index
- AST:
-
Aspartate aminotransferase
- AUC:
-
Area under the curve
- CONUT:
-
Controlling nutritional status
- CRP:
-
C-reactive protein
- CI:
-
Confidence interval
- DCP:
-
Des-gamma-carboxy prothrombin
- DFS:
-
Disease-free survival
- FIB-4:
-
Fibrosis-4 (index)
- HCC:
-
Hepatocellular carcinoma
- ICG-R15:
-
Indocyanine green dye retention rate at 15 min
- LMR:
-
Lymphocyte–monocyte ratio
- MELD:
-
Model for end-stage liver disease
- mGPS:
-
Modified Glasgow Prognostic Score
- NLR:
-
Neutrophil–lymphocyte ratio
- OS:
-
Overall survival
- PALBI:
-
Platelet–albumin–bilirubin (score)
- PLR:
-
Platelet-to-lymphocyte ratio
- PNI:
-
Prognostic nutritional index
- ROC:
-
Receiver operating characteristic
References
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. The Lancet. 2018;391(10127):1301–14.
Itoh S, Morita K, Ueda S, Sugimachi K, Yamashita Y, Gion T, et al. Long-term results of hepatic resection combined with intraoperative local ablation therapy for patients with multinodular hepatocellular carcinomas. Ann Surg Oncol. 2009;16(12):3299–307.
Roayaie S, Jibara G, Tabrizian P, Park JW, Yang J, Yan L, et al. The role of hepatic resection in the treatment of hepatocellular cancer. Hepatology. 2015;62(2):440–51.
Harimoto N, Yoshizumi T, Shimagaki T, Nagatsu A, Motomura T, Harada N, et al. Inflammation-based prognostic score in patients with living donor liver transplantation for hepatocellular carcinoma. Anticancer Res. 2016;36(10):5537–42.
Itoh S, Yugawa K, Shimokawa M, Yoshiya S, Mano Y, Takeishi K, et al. Prognostic significance of inflammatory biomarkers in hepatocellular carcinoma following hepatic resection. BJS Open. 2019;3(4):500–8.
Ohira M, Yoshizumi T, Yugawa K, Kosai-Fujimoto Y, Inokuchi S, Motomura T, et al. Association of inflammatory biomarkers with long-term outcomes after curative surgery for mass-forming intrahepatic cholangiocarcinoma. Surg Today. 2020;50(4):379–88.
Liu PH, Hsu CY, Hsia CY, Lee YH, Chiou YY, Huang YH, et al. ALBI and PALBI grade predict survival for HCC across treatment modalities and BCLC stages in the MELD Era. J Gastroenterol Hepatol. 2017;32(4):879–86.
Vallet-Pichard A, Mallet V, Nalpas B, Verkarre V, Nalpas A, Dhalluin-Venier V, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection comparison with liver biopsy and fibrotest. Hepatology. 2007;46(1):32–6.
Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38(2):518–26.
Yugawa K, Maeda T, Kinjo N, Kawata K, Ikeda S, Edahiro K, et al. (2021) Prognostic impact of lymphocyte-c-reactive protein ratio in patients who underwent surgical resection for hepatocellular carcinoma. J Gastrointest Surg
Kokudo N, Takemura N, Hasegawa K, Takayama T, Kubo S, Shimada M, et al. Clinical practice guidelines for hepatocellular carcinoma: the Japan Society of Hepatology 2017 (4th JSH-HCC guidelines) 2019 update. Hepatol Res. 2019;49(10):1109–13.
Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Tanaka K, et al. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol. 2015;22(3):803–10.
Gao F, Li X, Geng M, Ye X, Liu H, Liu Y, et al. Pretreatment neutrophil-lymphocyte ratio: an independent predictor of survival in patients with hepatocellular carcinoma. Medicine (Baltimore). 2015;94(11):e639.
Mano Y, Yoshizumi T, Yugawa K, Ohira M, Motomura T, Toshima T, et al. Lymphocyte-to-monocyte ratio is a predictor of survival after liver transplantation for hepatocellular carcinoma. Liver Transpl. 2018;24(11):1603–11.
Wang Y, Attar BM, Fuentes HE, Jaiswal P, Tafur AJ. Evaluation of the prognostic value of platelet to lymphocyte ratio in patients with hepatocellular carcinoma. J Gastrointest Oncol. 2017;8(6):1065–71.
Takagi K, Domagala P, Polak WG, Buettner S, Ijzermans JNM. Prognostic significance of the controlling nutritional status (CONUT) score in patients undergoing hepatectomy for hepatocellular carcinoma: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19(1):211.
Abe T, Tashiro H, Kobayashi T, Hattori M, Kuroda S, Ohdan H. Glasgow prognostic score and prognosis after hepatectomy for hepatocellular carcinoma. World J Surg. 2017;41(7):1860–70.
Imai D, Maeda T, Shimokawa M, Wang H, Yoshiya S, Takeishi K, et al. Prognostic nutritional index is superior as a predictor of prognosis among various inflammation-based prognostic scores in patients with hepatocellular carcinoma after curative resection. Hepatol Res. 2020;50(1):101–9.
Ha SY, Choi S, Park S, Kim JM, Choi GS, Joh JW, et al. Prognostic effect of preoperative neutrophil-lymphocyte ratio is related with tumor necrosis and tumor-infiltrating lymphocytes in hepatocellular carcinoma. Virchows Arch. 2020;477(6):807–16.
Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010;9:69.
Okamura Y, Ashida R, Yamamoto Y, Ito T, Sugiura T, Uesaka K. FIB-4 index is a predictor of background liver fibrosis and long-term outcomes after curative resection of hepatocellular carcinoma. Ann Surg Oncol. 2016;23(Suppl 4):467–74.
Sonohara F, Yamada S, Tanaka N, Tashiro M, Sunagawa Y, Morimoto D, et al. Comparison of non-invasive liver reserve and fibrosis markers: Implications for surgery and prognosis for hepatocellular carcinoma. Hepatol Res. 2019;49(11):1305–15.
Marasco G, Colecchia A, Silva G, Rossini B, Eusebi LH, Ravaioli F, et al. Non-invasive tests for the prediction of primary hepatocellular carcinoma. World J Gastroenterol. 2020;26(24):3326–43.
Kawasaki T, Takeshita A, Souda K, Kobayashi Y, Kikuyama M, Suzuki F, et al. Serum thrombopoietin levels in patients with chronic hepatitis and liver cirrhosis. Am J Gastroenterol. 1999;94(7):1918–22.
Tabrizian P, Jibara G, Shrager B, Schwartz M, Roayaie S. Recurrence of hepatocellular cancer after resection: patterns, treatments, and prognosis. Ann Surg. 2015;261(5):947–55.
Acknowledgements
Source of funding is not applicable. The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yugawa, K., Maeda, T., Nagata, S. et al. A novel combined prognostic nutritional index and aspartate aminotransferase-to-platelet ratio index-based score can predict the survival of patients with hepatocellular carcinoma who undergo hepatic resection. Surg Today 52, 1096–1108 (2022). https://doi.org/10.1007/s00595-021-02440-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02440-0