Abstract
Purpose
Although robotic surgery for rectal cancer can overcome the shortcomings of laparoscopic surgery, studies focusing on abdominoperineal resection are limited. The aim of this study was to compare the operative outcomes between robotic and laparoscopic abdominoperineal resection.
Methods
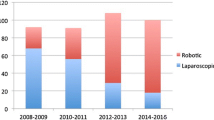
This retrospective cohort study was conducted from April 2010 to March 2020. Patients with rectal cancer who underwent robotic or laparoscopic abdominoperineal resection without lateral lymph node dissection were enrolled. The perioperative and oncological outcomes were compared.
Results
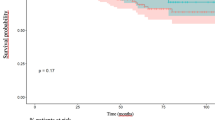
We evaluated 33 and 20 patients in the robotic and laparoscopic groups, respectively. The median operative time and blood loss were comparable between the two groups. No significant differences in the overall complication rates were noted, whereas the rates of urinary dysfunction (3% vs. 26%, p = 0.02) and perineal wound infection (9% vs. 35%, p = 0.03) in the robotic group were significantly lower in comparison to the laparoscopic group. The median postoperative hospital stay was significantly shorter in the robotic group (8 days vs. 11 days, p < 0.01). The positive resection margin rates were comparable between the two groups.
Conclusion
Robotic abdominoperineal resection demonstrated better short-term outcomes than laparoscopic surgery, suggesting that it could be a useful approach.


Similar content being viewed by others
References
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, et al. Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA. 2015;314:1346–55.
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, et al. Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA. 2015;314:1356–63.
Prete FP, Pezzolla A, Prete F, Testini M, Marzaioli R, Patriti A, et al. Robotic versus laparoscopic minimally invasive surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Surg. 2018;267:1034–46.
Hoshino N, Sakamoto T, Hida K, Sakai Y. Robotic versus laparoscopic surgery for rectal cancer: an overview of systematic reviews with quality assessment of current evidence. Surg Today. 2019;49:556–70.
Broholm M, Pommergaard H-C, Gogenur I. Possible benefits of robot-assisted rectal cancer surgery regarding urological and sexual dysfunction: a systematic review and meta-analysis. Colorectal Dis. 2014;17:375–81.
Liao G, Zhao Z, Deng H, Li X. Comparison of pathological outcomes between robotic rectal cancer surgery and laparoscopic rectal cancer surgery: a meta-analysis based on seven randomized controlled trials. Int J Med Robot. 2019;15:e2027.
Han C, Yan P, Jing W, Li M, Du B, Si M, et al. Clinical, pathological, and oncologic outcomes of robotic-assisted versus laparoscopic proctectomy for rectal cancer: a meta-analysis of randomized controlled studies. Asian J Surg. 2020;43:880–90.
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, et al. Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA. 2017;318:1569–80.
Shiomi A, Kinugasa Y, Yamaguchi T, Kagawa H, Yamakawa Y. Robot-assisted versus laparoscopic surgery for lower rectal cancer: the impact of visceral obesity on surgical outcomes. Int J Colorectal Dis. 2016;31:1701–10.
Hino H, Yamaguchi T, Kinugasa Y, Shiomi A, Kagawa H, Yamakawa Y, et al. Robotic-assisted multivisceral resection for rectal cancer: short-term outcomes at a single center. Tech Coloproctol. 2017;21:879–86.
Mesquita-Neto JWB, Mouzaihem H, Macedo FIB, Heilbrun LK, Weaver DW, Kim S. Perioperative and oncological outcomes of abdominoperineal resection in the prone position vs the classic lithotomy position: a systematic review with meta-analysis. J Surg Oncol. 2019;119:979–86.
van Leersum N, Martijnse I, den Dulk M, Kolfschoten N, Le Cessie S, van de Velde C, et al. Differences in circumferential resection margin involvement after abdominoperineal excision and low anterior resection no longer significant. Ann Surg. 2014;259:1150–5.
Imaizumi K, Nishizawa Y, Ikeda K, Tsukada Y, Sasaki T, Ito M. Extended pelvic resection for rectal and anal canal tumors is a significant risk factor for perineal wound infection: a retrospective cohort study. Surg Today. 2018;48:978–85.
West NP, Anderin C, Smith KJE, Holm T, Quirke P. European Extralevator Abdominoperineal Excision Study Group. Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. Br J Surg. 2010;97:588–99.
Moghadamyeghaneh Z, Phelan M, Smith BR, Stamos MJ. Outcomes of open, laparoscopic, and robotic abdominoperineal resections in patients with rectal cancer. Dis Colon Rectum. 2015;58:1123–9.
Kamali D, Reddy A, Imam S, Omar K, Jha A, Jha M. Short-term surgical outcomes and patient quality of life between robotic and laparoscopic extralevator abdominoperineal excision for adenocarcinoma of the rectum. Ann R Coll Surg Engl. 2017;99:607–13.
Fujita S, Akasu T, Mizusawa J, Saito N, Kinugasa Y, Kanemitsu Y, et al. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012;13:616–21.
Shiomi A, Kinugasa Y, Yamaguchi T, Tomioka H, Kagawa H. Robot-assisted rectal cancer surgery: short-term outcomes for 113 consecutive patients. Int J Colorectal Dis. 2014;29:1105–11.
Kagawa H, Kinugasa Y, Shiomi A, Yamaguchi T, Tsukamoto S, Tomioka H, et al. Robotic-assisted lateral lymph node dissection for lower rectal cancer: short-term outcomes in 50 consecutive patients. Surg Endosc. 2015;29:995–1000.
Kinugasa Y, Murakami G, Uchimoto K, Takenaka A, Yajima T, Sugihara K. Operating behind Denonvilliers’ fascia for reliable preservation of urogenital autonomic nerves in total mesorectal excision: a histologic study using cadaveric specimens, including a surgical experiment using fresh cadaveric models. Dis Colon Rectum. 2006;49:1024–32.
Kinugasa Y, Murakami G, Suzuki D, Sugihara K. Histological identification of fascial structures posterolateral to the rectum. Br J Surg. 2007;94:620–6.
Kinugasa Y, Arakawa T, Abe SI, Ohtsuka A, Suzuki D, Murakami G, et al. Anatomical reevaluation of the anococcygeal ligament and its surgical relevance. Dis Colon Rectum. 2011;54:232–7.
Clavien PA, Barkun J, De Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Ito M, Kobayashi A, Fujita S, Mizusawa J, Kanemitsu Y, Kinugasa Y, et al. Urinary dysfunction after rectal cancer surgery: Results from a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for clinical stage II or III lower rectal cancer (Japan Clinical Oncology Group Study, JCOG0212). Eur J Surg Oncol. 2018;44:463–8.
Yamaoka Y, Kagawa H, Shiomi A, Yamakawa Y, Hino H, Manabe S, et al. Robotic-assisted surgery may be a useful approach to protect urinary function in the modern era of diverse surgical approaches for rectal cancer. Surg Endosc. 2020;35:1317–23.
Black AJ, Karimuddin A, Raval M, Phang T, Brown C. The impact of laparoscopic technique on the rate of perineal hernia after abdominoperineal resection of the rectum. Surg Endosc. 2020. https://doi.org/10.1007/s00464-020-07746-7.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Kang SB, Park JW, Jeong SY, Nam B, Choi HS, Kim D-W, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010;11:637–45.
van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013;14:210–8.
Kim J, Baek SJ, Kang DW, Roh Y-E, Lee JW, Kwak H-D, et al. Robotic resection is a good prognostic factor in rectal cancer compared with laparoscopic resection: long-term survival analysis using propensity score matching. Dis Colon Rectum. 2017;60:266–73.
Yamaguchi T, Kinugasa Y, Shiomi A, Kagawa H, Yamakawa Y, Furuatni A, et al. Short- and long-term outcomes of robotic-assisted laparoscopic surgery for rectal cancer: results of a single high-volume center in Japan. Int J Colorectal Dis. 2018;33:1755–62.
Eftaiha SM, Pai A, Sulo S, Park JJ, Prasad LM, Marecik SJ. Robot-assisted abdominoperineal resection: clinical, pathologic, and oncologic outcomes. Dis Colon Rectum. 2016;59:607–14.
Kim JC, Lee JL, Kim CW. Comparative analysis of robot-assisted vs open abdominoperineal resection in terms of operative and initial oncological outcomes. Ann Surg Treat Res. 2018;95:37–44.
Kasparek MS, Hassan I, Cima RR, Larson DR, Gullerud RE, Wolff BG. Long-term quality of life and sexual and urinary function after abdominoperineal resection for distal rectal cancer. Dis Colon Rectum. 2012;55:147–54.
Marecik SJ, Zawadzki M, deSouza AL, Park JJ, Abcarian H, Prasad LM. Robotic cylindrical abdominoperineal resection with transabdominal levator transection. Dis Colon Rectum. 2011;54:1320–5.
Chi P, Chen ZF, Lin HM, Lu XR, Huang Y. Laparoscopic extralevator abdominoperineal resection for rectal carcinoma with transabdominal levator transection. Ann Surg Oncol. 2013;20:1560–6.
Wiatrek RL, Thomas JS, Papaconstantinou HT. Perineal wound complications after abdominoperineal resection. Clin Colon Rectal Surg. 2008;21:76–85.
Keller DS, Champagne BJ, Reynolds JHL, Stein SL, Delaney CP. Cost-effectiveness of laparoscopy in rectal cancer. Dis Colon Rectum. 2014;57:564–9.
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioki Y, Hamaguchi T, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1–42.
Acknowledgements
We wish to thank Takanori Kawabata, a biostatistician, for providing advice on the statistical analyses. We are grateful to Reiko Suzuki for her narration of Online Resource 1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in association with the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Online Resource 1: Dissection of the levator ani muscle in robotic abdominoperineal resection Robotic surgery typically enables dissection of the levator ani muscle in abdominoperineal resection. Reaching the ischiorectal fossa as deeply as possible in the abdominopelvic procedure allows better access for perineal dissection (MPG 5434 KB)
Rights and permissions
About this article
Cite this article
Kasai, S., Kagawa, H., Shiomi, A. et al. Advantages of robotic abdominoperineal resection compared with laparoscopic surgery: a single-center retrospective study. Surg Today 52, 643–651 (2022). https://doi.org/10.1007/s00595-021-02359-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02359-6