Abstract
Purpose
Systemic inflammatory response influences cancer development and perioperative surgical stress can affect the survival of patients with colorectal cancer (CRC). We developed a system to cumulatively assess perioperative inflammatory response and compare the prognostic value of various cumulative inflammatory and nutritional markers in patients with CRC.
Methods
We assessed perioperative cumulative markers using the trapezoidal area method in 307 patients who underwent surgery for CRC and analyzed the results statistically.
Results
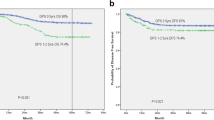
The cumulative lymphocyte to C-reactive protein (CRP) ratio (LCR) predicted survival more accurately than other well-established markers (sensitivity: 80.0%, specificity: 69.3%; area under the curve (AUC): 0.779; P < 0.001). A low cumulative LCR was correlated with factors associated with disease development, including undifferentiated histology, advanced T stage, lymph node metastasis, distant metastasis, and advanced TNM stage classification. A decreased cumulative LCR was an independent prognostic factor for both overall survival (OS) (Hazard Ratio (HR):5.21, 95% confidence interval [CI] 2.42–11.2; P < 0.0001) and disease-free survival (DFS) (HR: 1.88, 95% CI 1.07–3.31; P = 0.02), and its prognostic significance was verified in a different clinical setting. The cumulative LCR was correlated negatively with the intraoperative bleeding volume (P < 0.0001, R = −0.4). Combined analysis of cumulative and preoperative LCR could help stratify risk for the oncological outcomes of CRC patients.
Conclusions
The findings of this study demonstrate the value of the cumulative LCR in the postoperative management of patients with CRC.



Similar content being viewed by others
Availability of data and materials
Primary research data are presented in a summative fashion. No publicly available datasets have been generated as part of this work.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–503.
Zhang J, Zhang H-Y, Li J, Shao X-Y, Zhang C-X. The elevated NLR, PLR and PLT may predict the prognosis of patients with colorectal cancer: a systematic review and meta-analysis. Oncotarget. 2017;8(40):68837–46.
Koike Y, Miki C, Okugawa Y, Yokoe T, Toiyama Y, Tanaka K, et al. Preoperative C-reactive protein as a prognostic and therapeutic marker for colorectal cancer. J Surg Oncol. 2008;98(7):540–4.
Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Shibuya N, Kubota K. Clinical significance of the C-reactive protein to albumin ratio for survival after surgery for colorectal cancer. Ann Surg Oncol. 2016;23(3):900–7.
Liang L, Zhu J, Jia H, Huang L, Li D, Li Q, et al. Predictive value of pretreatment lymphocyte count in stage II colorectal cancer and in high-risk patients treated with adjuvant chemotherapy. Oncotarget. 2016;7(1):1014–28.
Okugawa Y, Toiyama Y, Yamamoto A, Shigemori T, Ide S, Kitajima T, et al. Lymphocyte-C-reactive protein ratio as promising new marker for predicting surgical and oncological outcomes in colorectal cancer. Annals Surg. 2019. https://doi.org/10.1097/SLA.0000000000003239.
Azab B, Kedia S, Shah N, Vonfrolio S, Lu W, Naboush A, et al. The value of the pretreatment albumin/globulin ratio in predicting the long-term survival in colorectal cancer. Int J Colorectal Dis. 2013;28(12):1629–36.
Tan D, Fu Y, Tong W, Li F. Prognostic significance of lymphocyte to monocyte ratio in colorectal cancer: A meta-analysis. Int J Surg. 2018;55:128–38.
Jian-Hui C, Iskandar EA, Cai S-I, Chen C-Q, Wu H, Xu J-B, et al. Significance of Onodera’s prognostic nutritional index in patients with colorectal cancer: a large cohort study in a single Chinese institution. Tumour Biol. 2016;37(3):3277–83.
Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints. preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69(3):89–95.
Yamamoto M, Saito H, Uejima C, Tanio A, Tada Y, Matsunaga T, et al. Estimation of Physiological Ability and Surgical Stress Score Is a Useful Prognostic Indicator for Elderly Patients with Colorectal Cancer. Digestive surgery. 2019:1–9.
Hirai T, Matsumoto H, Yamashita K, Urakami A, Iki K, Yamamura M, et al. Surgical oncotaxis–excessive surgical stress and postoperative complications contribute to enhancing tumor metastasis, resulting in a poor prognosis for cancer patients. Ann Thorac Cardiovasc Surg. 2005;11(1):4–6.
Keibel A, Singh V, Sharma MC. Inflammation, microenvironment, and the immune system in cancer progression. Curr Pharm Des. 2009;15(17):1949–55.
Hirai T, Yoshimoto A, Iwata T, Yamashita Y, Kuwahara M, Toge T. Enhancing effect of thoraco-laparotomy on liver metastasis and the role played by active oxygens in its mechanism. Surg Today. 1997;27(11):1040–5.
Ide S, Toiyama Y, Okugawa Y, Oki S, Yasuda H, Fujikawa H, et al. Clinical significance of C-reactive protein-to-albumin ratio with rectal cancer patient undergoing chemoradiotherapy followed by surgery. Anticancer Res. 2017;37(10):5797–804.
Yamamoto A, Toiyama Y, Okugawa Y, Oki S, Ide S, Saigusa S, et al. Clinical implications of pretreatment: lymphocyte-to-monocyte ratio in patients with rectal cancer receiving preoperative chemoradiotherapy. Dis Colon Rectum. 2019;62(2):171–80.
Okugawa Y, Toiyama Y, Oki S, Ide S, Yamamoto A, Ichikawa T, et al. Feasibility of assessing prognostic nutrition index in patients with rectal cancer who receive preoperative chemoradiotherapy. J Parenter Enteral Nutr. 2018;42(6):998–1007.
Edge SB BD CC, Fritz AG, Greene FL, Trotti A, eds. AJCC Cancer Staging Manual. 7th ed New York: Springer. 2010.
Okugawa Y, Toiyama Y, Yamamoto A, Shigemori T, Ichikawa T, Yin C, et al. Lymphocyte-to-C-reactive protein ratio and score are clinically feasible nutrition-inflammation markers of outcome in patients with gastric cancer. Clin Nutr. 2019;S0261–5614(19):30220–1.
van der Bij GJ, Oosterling SJ, Beelen RHJ, Meijer S, Coffey JC, van Egmond M. The perioperative period is an underutilized window of therapeutic opportunity in patients with colorectal cancer. Ann Surg. 2009;249(5):727–34.
Hirakawa S, Kodama S, Kunstfeld R, Kajiya K, Brown LF, Detmar M. VEGF-A induces tumor and sentinel lymph node lymphangiogenesis and promotes lymphatic metastasis. J Exp Med. 2005;201(7):1089–99.
Cao R, Björndahl MA, Religa P, Clasper S, Garvin S, Galter D, et al. PDGF-BB induces intratumoral lymphangiogenesis and promotes lymphatic metastasis. Cancer Cell. 2004;6(4):333–45.
Tsuchiya Y, Sawada S, Yoshioka I, Ohashi Y, Matsuo M, Harimaya Y, et al. Increased surgical stress promotes tumor metastasis. Surgery. 2003;133(5):547–55.
Toiyama Y, Fujikawa H, Koike Y, Saigusa S, Inoue Y, Tanaka K, et al. Evaluation of preoperative C-reactive protein aids in predicting poor survival in patients with curative colorectal cancer with poor lymph node assessment. Oncol Lett. 2013;5(6):1881–8.
Nozoe T, Matsumata T, Sugimachi K. Preoperative elevation of serum C-reactive protein is related to impaired immunity in patients with colorectal cancer. Am J Clin Oncol. 2000;23(3):263–6.
Sarraf KM, Belcher E, Raevsky E, Nicholson AG, Goldstraw P, Lim E. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg. 2009;137(2):425–8.
Kanda M, Mizuno A, Tanaka C, Kobayashi D, Fujiwara M, Iwata N, et al. Nutritional predictors for postoperative short-term and long-term outcomes of patients with gastric cancer. Medicine. 2016;95(24):e3781.
Kono Y, Saito H, Murakami Y, Shishido Y, Kuroda H, Matsunaga T, et al. Postoperative ratio of the maximum C-reactive protein level to the minimum peripheral lymphocyte count as a prognostic indicator for gastric cancer patients. Surg Today. 2019;49(3):206–13.
Kitano S, Inomata M, Mizusawa J, Katayama H, Watanabe M, Yamamoto S, et al. Survival outcomes following laparoscopic versus open D3 dissection for stage II or III colon cancer (JCOG0404): a phase 3, randomised controlled trial. Lancet Gastroenterol Hepatol. 2017;2(4):261–8.
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Jr., et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Annals of surgery. 2007;246(4):655–62; discussion 62–4.
Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10(1):44–52.
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ. Long-term results of laparoscopic colorectal cancer resection. The Cochrane database of systematic reviews. 2008;2008(2):Cd003432.
Funding
Source of financial support: None.
Author information
Authors and Affiliations
Contributions
Study concept and design (YO, YT); provision of samples (HF, MK, HY, TY, YO, MO); acquisition of data (YO, YT, HF, MK, HY, TY, IM, YO, MO, KN); analysis and interpretation of data (YO, YT, MO, KN); statistical analysis (YO, YT); drafting of the manuscript (YO, YT, KN).
Corresponding author
Ethics declarations
Conflict of interests
We have no conflict of interests to disclose for this study.
Ethics approval and consent to participate
This retrospective observational study was approved by the institutional review board of Mie University Hospital. We offered an opt-out for participants to provide the opportunity to decline participation in the study. This study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Okugawa, Y., Toiyama, Y., Fujikawa, H. et al. Cumulative perioperative lymphocyte/C-reactive protein ratio as a predictor of the long-term outcomes of patients with colorectal cancer. Surg Today 51, 1906–1917 (2021). https://doi.org/10.1007/s00595-021-02291-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02291-9