Abstract
Purpose
To analyze the impact of postoperative remote infections (PRIs) on medical expenditure.
Methods
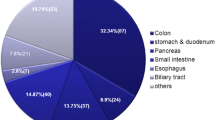
The subjects of this retrospective study were 338 patients who had undergone gastroenterological surgery at one of the 20 Japanese institutions within the Japan Society for Surgical Infection (JSSI) and mainly authorized as educational institutions. The patients were allocated to 169 pairs of those with a PRI (PRI (+) group) matched with those without a PRI (PRI (−) group). PRIs included pneumonia, urinary tract infection (UTI), catheter-associated blood stream infection (CA-BSI), and antibiotic-associated enteritis.
Results
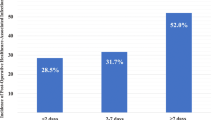
SSI developed in 74 of the 338 patients (22 without PRI and 52 with PRI). The SSI incidence was significantly higher in the PRI (+) group (p < 0.001). The difference in the median postoperative length of hospital stay was 15 days, indicating a significant prolongation in the PRI (+) group (p < 0.001). The PRI (+) group also had a higher rate of inter-hospital transfer (p < 0.01) and mortality (p < 0.001). Similarly, the difference in median postoperative medical fees was $6832.3, representing a significant increase in the PRI (+) group (p < 0.001).
Conclusions
The postoperative length of hospital stay is longer and the postoperative medical expenditure is higher for patients with a PRI than for those without a PRI.



Similar content being viewed by others
References
Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. 2017;96:1–15.
de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009;37:387–97.
Kusachi S, Kashimura N, Konishi T, Shimizu J, Kusunoki M, Oka M, et al. Length of stay and cost for surgical site infection after abdominal and cardiac surgery in Japanese hospitals: multi-center surveillance. Surg Infect (Larchmt). 2012;13:257–65.
Kashimura N, Kusachi S, Konishi T, Shimizu J, Kusunoki M, Oka M, Wakatsuki T, Sumiyama Y. Impact of surgical site infection after colorectal surgery on hospital stay and medical expenditure in Japan. Surg Today. 2012;42(7):639–45. https://doi.org/10.1007/s00595-012-0126-8.
Kobayashi J, Kusachi S, Sawa Y, Motomura N, Imoto Y, Makuuchi H, Tanemoto K, Shimahara Y, Sumiyama Y. Socioeconomic effects of surgical site infection after cardiac surgery in Japan. Surg Today. 2015;45(4):422–8. https://doi.org/10.1007/s00595-014-0969-2 Epub 2014 Jun 28.
Niitsuma T, Kusachi S, Takesue Y, Mikamo H, Asai K, Watanabe M. Current status of postoperative infections after digestive surgery in Japan: the Japan Postoperative Infectious Complications Survey in 2015. Ann Gastroenterol Surg. 2019;3:276–84.
Overview of Medical Service Regime in Japan. 2015. https://www.mhlw.go.jp/bunya/iryouhoken/iryouhoken01/dl/01_eng.pdf#search='medical+service+fees+grade+table.
JHPN (Japan Health Policy Now) Payment system. 2016. https://japanhpn.org/en/finan2/.
Soma D, Kawamura YI, Yamashita S, Wake H, Nohara K, Yamada K, et al. Sarcopenia, the depletion of muscle mass, an independent predictor of respiratory complications after oncological esophagectomy. Dis Esophagus. 2019. https://doi.org/10.1093/dote/doy092.
Berlth F, Plum PS, Chon SH, Gutschow CA, Bollschweiler E, Holscher AH. Total minimally invasive esophagectomy for esophageal adenocarcinoma reduces postoperative pain and pneumonia compared to hybrid esophagectomy. Surg Endosc. 2018;32:4957–65.
Hochreiter M, Uhling M, Sisic L, Bruckner T, Heininger A, Hohn A, et al. Prolonged antibiotic prophylaxis after thoracoabdominal esophagectomy does not reduce the risk of pneumonia in the first 30 days: a retrospective before-and-after analysis. Infection. 2018;46:617–24.
Kusachi S, Nagao J, Saida Y, Watanabe M, Nakamura Y, Asai K, et al. Twenty years of countermeasures against postoperative methicillin-resistant Staphylococcus aureus infections. Surg Today. 2011;41:630–6.
Kusachi S, Sumiyama Y, Nagao J, Kawai K, Arima Y, Yoshida Y, et al. New methods of control against postoperative methicillin-resistant Staphylococcus aureus infection. Surg Today. 1999;29:724–9.
Klionsky DJ, Abdelmohsen K, Abe A, Abedin MJ, Abeliovich H, Acevedo Arozena A, et al. Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy. 2016;12:1–222.
Kusachi S, Sumiyama Y, Arima Y, Yoshida Y, Tanaka H, Nakamura Y, et al. Success of countermeasures against respiratory infection after digestive surgery by strict blood and fluid resuscitation. J Infect Chemother. 2007;13:172–6.
Acknowledgements
We thank Prof. Yoshitaka Murakami (Department of Medical Statistics, Toho University), whose comments and suggestions for statistics analysis were of inestimable value. We also express our sincere gratitude for the excellent cooperation provided by the collaborators and personnel in charge of information provision in the medical information departments and medical affairs divisions at the information provision medical institutions. Personnel in charge of providing information from the medical institutions (Honorific titles omitted): Eiji Tsujita, National Hospital Organization Kyushu Cancer Center; Junzo Shimizu and Ryohei Kawabata, Osaka Rosai Hospital; Yoshihiro Edamoto, National Center for Global Health and Medicine; Tsukasa Takayashiki, Chiba University; Masaru Koizumi, Jichi Medical University; Akihisa Matsuda, Nippon Medical School, Chiba Hokusoh Hospital; Makoto Nagashima, Toho University Sakura Hospital; Masamichi Mizuma, Tohoku University Hospital; Takehiro Wakasugi, Takeshi Yanagida and Nobuko Yamada, Nagoya City University; Mami Ikeda, JCHO Tokyo Takanawa Hospital; Minako Kobayashi, Mie University; Yukiko Kato, Aichi Medical University Hospital; Hitoshi Kanno, Nippon Medical School; Hiroshi Maruyama, Nippon Medical School Tama Nagayama Hospital; Kazuhiko Yoshimatsu, Saitama Prefecture Saiseikai Kurihashi Hospital; Hiroyuki Kasajima, Hakodate Municipal Hospital; Futoshi Teranishi, Toyokawa City Hospital; Masahiko Sakoda, Kagoshima University School of Medicine; Michinori Matsumoto, The Jikei University School of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hironobu Nishimuta and the co-authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nishimuta, H., Kusachi, S., Watanabe, M. et al. Impact of postoperative remote infection on length of stay and medical costs in hospitals in Japan. Surg Today 51, 212–218 (2021). https://doi.org/10.1007/s00595-020-02113-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-02113-4