Abstract
Purposes
Postoperative complications are associated with poor overall and cancer-specific survival after resection of various types of cancer, including primary colorectal cancer. However, the oncological impact of surgical site infection (SSI) after liver resection for colorectal liver metastases (CLM) is unclear. The aim of this study was to investigate the oncological impact of SSI after liver resection for CLM.
Methods
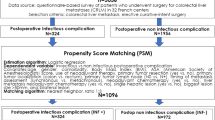
We reviewed data from 367 consecutive patients treated by curative liver resection for CLM between 1994 and 2015. Patients who underwent simultaneous resection of colorectal cancer and synchronous liver metastases (n = 86) were excluded from the analysis. Short- and long-term outcomes were analyzed.
Results
SSI developed in 18 (6.4%) of the 281 patients in the analytic cohort (SSI group). The remaining 93.6% (n = 263) did not suffer this complication (no-SSI group). The operative duration was significantly longer in the SSI group than in the No-SSI group (p = 0.002). The overall survival rates 5 years after liver resection for CLM were 33.3% in the SSI group vs. 50.7% in the No-SSI group (p = 0.043). Multivariate analysis indicated that a liver tumor size ≥ 5 cm, R1 resection, and SSI were independently associated with overall survival after liver resection.
Conclusions
SSI after liver resection for CLM is associated with adverse oncological outcomes.

Similar content being viewed by others
References
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–18.
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241:715–22.
Simmonds PC, Primrose JN, Colquitt JL, Garden OJ, Poston GJ, Rees M. Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies. Br J Cancer. 2006;94:982–99.
Are C, Gonen M, Zazzali K, Dematteo RP, Jarnagin WR, Fong Y, et al. The impact of margins on outcome after hepatic resection for colorectal metastasis. Ann Surg. 2007;246:295–300.
Muratore A, Ribero D, Zimmitti G, Mellano A, Langella S, Capussotti L. Resection margin and recurrence-free survival after liver resection of colorectal metastases. Ann Surg Oncol. 2010;17:1324–9.
Tanaka K, Matsuo K, Kawaguchi D, Murakami T, Hiroshima Y, Hirano A, et al. Randomized clinical trial of peritoneal lavage for preventing surgical site infection in elective liver surgery. J Hepatobiliary Pancreat Sci. 2015;22:446–53.
Kokudo T, Uldry E, Demartines N, Halkic N. Risk factors for incisional and organ space surgical site infections after liver resection are different. World J Surg. 2015;39:1185–92.
López-Ben S, Palacios O, Codina-Barreras A, Albiol MT, Falgueras L, Castro E, et al. Pure laparoscopic liver resection reduces surgical site infections and hospital stay. Results of a case-matched control study in 50 patients. Langenbecks Arch Surg. 2014;399:307–14.
Maehara Y, Shirabe K, Kohnoe S, Emi Y, Oki E, Kakeji Y, et al. Impact of intra-abdominal absorbable sutures on surgical site infection in gastrointestinal and hepato-biliary-pancreatic surgery: results of a multicenter, randomized, prospective, phase II clinical trial. Surg Today. 2017;47:1060–71.
Sakoda M, Iino S, Mataki Y, Kawasaki Y, Kurahara H, Maemura K, et al. Influence of a shorter duration of post-operative antibiotic prophylaxis on infectious complications in patients undergoing elective liver resection. Surg Infect (Larchmt). 2017;18:149–56.
Hirokawa F, Hayashi M, Miyamoto Y, Asakuma M, Shimizu T, Komeda K, et al. Evaluation of postoperative antibiotic prophylaxis after liver resection: a randomized controlled trial. Am J Surg. 2013;206:8–15.
Hill MV, Holubar SD, Garfield Legare CI, Luurtsema CM, Barth RJ Jr. Perioperative bundle decreases postoperative hepatic surgery infections. Ann Surg Oncol. 2015;22:1140–6.
Shwaartz C, Fields AC, Aalberg JJ, Divino CM. Role of drain placement in major hepatectomy: a NSQIP analysis of procedure-targeted hepatectomy cases. World J Surg. 2017;41:1110–8.
Law WL, Choi HK, Lee YM, Ho JW. The impact of postoperative complications on long-term outcomes following curative resection for colorectal cancer. Ann Surg Oncol. 2007;14:2559–66.
Chok KS, Ng KK, Poon RT, Lo CM, Fan ST. Impact of postoperative complications on long-term outcome of curative resection for hepatocellular carcinoma. Br J Surg. 2009;96:81–7.
de Melo GM, Ribeiro KC, Kowalski LP, Deheinzelin D. Risk factors for postoperative complications in oral cancer and their prognostic implications. Arch Otolaryngol Head Neck Surg. 2001;127:828–33.
Rizk NP, Bach PB, Schrag D, Bains MS, Turnbull AD, Karpeh M, et al. The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg. 2004;198:42–50.
Farid SG, Aldouri A, Morris-Stiff G, Khan AZ, Toogood GJ, Lodge JP, et al. Correlation between postoperative infective complications and long-term outcomes after hepatic resection for colorectal liver metastasis. Ann Surg. 2010;251:91–100.
Mavros MN, de Jong M, Dogeas E, Hyder O, Pawlik TM. Impact of complications on long-term survival after resection of colorectal liver metastases. Br J Surg. 2013;100:711–8.
Matsuda A, Matsumoto S, Seya T, Matsutani T, Kishi T, Yokoi K, et al. Does postoperative complication have a negative impact on long-term outcomes following hepatic resection for colorectal liver metastasis?: a meta-analysis. Ann Surg Oncol. 2013;20:2485–92.
Kulaylat AN, Bhayani NH, Stokes AL, Schubart JR, Wong J, Kimchi ET, et al. Determinants of repeat curative intent surgery in colorectal liver metastasis. J Gastrointest Surg. 2014;18:1894–901.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Lundy J, Ford CM. Surgery, trauma and immune suppression. Evolving the mechanism. Ann Surg. 1983;197:434–8.
Horn F, Henze C, Heidrich K. Interleukin-6 signal transduction and lymphocyte function. Immunobiology. 2000;202:151–67.
Wong VK, Malik HZ, Hamady ZZ, Al-Mukhtar A, Gomez D, Prasad KR, et al. C-reactive protein as a predictor of prognosis following curative resection for colorectal liver metastases. Br J Cancer. 2007;96:222–5.
Yoshimura Y, Kubo S, Hirohashi K, Ogawa M, Morimoto K, Shirata K, et al. Plastic iodophor drape during liver surgery operative use of the iodophor-impregnated adhesive drape to prevent wound infection during high risk surgery. World J Surg. 2003;27:685–8.
Scilletta R, Pagano D, Spada M, Mongiovì S, Pesce A, Portale TR, et al. Comparative analysis of the incidence of surgical site infections in patients with liver resection for colorectal hepatic metastases after neoadjuvant chemotherapy. J Surg Res. 2014;188:183–9.
Kobayashi S, Gotohda N, Nakagohri T, Takahashi S, Konishi M, Kinoshita T. Risk factors of surgical site infection after hepatectomy for liver cancers. World J Surg. 2009;33:312–7.
Fahy BN, Fischer CP. Synchronous resection of colorectal primary and hepatic metastasis. J Gastrointest Oncol. 2012;3:48–58.
Fukami Y, Kaneoka Y, Maeda A, Takayama Y, Onoe S, Isogai M. Simultaneous resection for colorectal cancer and synchronous liver metastases. Surg Today. 2016;46:176–82.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Fukami, Y., Maeda, A., Takayama, Y. et al. Adverse oncological outcome of surgical site infection after liver resection for colorectal liver metastases. Surg Today 49, 170–175 (2019). https://doi.org/10.1007/s00595-018-1715-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1715-y