Abstract
Purpose
To evaluate the characteristics of lymph node assessment in the Spanish Colorectal Metastasectomy Registry (GECMP-CCR) and to analyze and compare the survival of patients with pathological absence or presence of lymph node metastases (LNM) with the survival of those with uncertain lymph node status (uLNs).
Methods
A total of 522 patients with lung metastases from colorectal carcinoma were prospectively registered from 2008 to 2010. To confirm the pathologic absence of LNM, systematic nodal dissection or systematic sampling was required, or the lymph node status was coded as uncertain. Disease-specific survival and disease-free survival were calculated by the Kaplan–Meier method with the log-rank test for comparisons.
Results
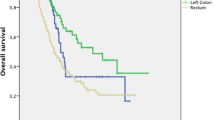
Lymphadenectomy was performed in 250 (48 %) patients. LNM was found in 25 (10 %) of the patients who had lymph node assessment done. The 3- and 5-year disease-specific survival rates according to lymph node status were 73.5 and 58.3 % in the absence of LNM, 50.5 and 24.8 % when LNM was confirmed, and 69 and 44 % for those with uLNs, respectively (p = 0.006).
Conclusions
The presence of LNM and uLNs is associated with an increased risk of death. The association of nodal assessment at the time of metastasectomy to identify LNM helps us to refine the postoperative prognosis; therefore, its impact should be properly studied in a prospective clinical trial.



Similar content being viewed by others
References
Pastorino U, Buyse M, Friedel G. Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. The International Registry of Lung Metastases. J Thorac Cardiovasc Surg. 1997;113:37–49.
Dominguez-Ventura A, Nichols FC. Lymphadenectomy in metastasectomy. Thorac Surg Clin. 2006;16:139–43.
Gonzalez M, Poncet A, Combescure C, Robert J, Ris HB, Gervaz P. Risk factors for survival after lung metastasectomy in colorectal cancer patients: a systematic review and meta-analysis. Ann Surg Oncol. 2012;20:572–9.
Embun R, Fiorentino F, Treasure T, Rivas JJ, Molins L. Pulmonary metastasectomy in colorectal cancer: a prospective study of demography and clinical characteristics of 543 patients in the Spanish colorectal metastasectomy registry (GECMP-CCR). BMJ Open. 2013;3(5):e002787. doi:10.1136/bmjopen-2013-002787.
Grupo Cooperativo de Carcinoma Broncogénico de la Sociedad Española de Neumología y Cirugía Torácica GCCB-S. Estadificación ganglionar intraoperatoria en la cirugía del carcinoma broncogénico. Documento de consenso. Arch Bronconeumol. 2001;37:495–503.
Martini N, McCormack PM. Evolution of the surgical management of pulmonary metastases. Chest Surg Clin N Am. 1998;8:13–27.
Treasure T, Milosevic M, Fiorentino F, Macbeth F. Pulmonary metastasectomy: what is the practice and where is the evidence for effectiveness? Thorax. 2014;69:946–9.
Rami-Porta R, Wittekind C, Goldstraw P; International Association for the lung cancer (IASLC) Staging Comitee. Complete resection in lung cancer surgery: proposed definition. Lung Cancer. 2005;49:25–33.
Internullo E, Cassivi SD, Van Raemdonck D, Friedel G, Treasure T. Pulmonary metastasectomy: a survey of current practice amongst members of the European Society of Thoracic Surgeons. J Thorac Oncol. 2008;3:1257–66.
Pfannschmidt J, Klode J, Muley T, Dienemann H, Hoffmann H. Nodal involvement at the time of pulmonary metastasectomy: experiences in 245 patients. Ann Thorac Surg. 2006;81:448–54.
Renaud S, Alifano M, Falcoz PE, Magdeleinat P, Santelmo N, Pagès O, et al. Does nodal status influence survival? Results of a 19-year systematic lymphadenectomy experience during lung metastasectomy of colorectal cancer. Interact CardioVasc Thorac Surg. 2014;18:482–7.
Pfannschmidt J, Hoffmann H, Dienemann H. Reported outcome factors for pulmonary resection in metastatic colorectal cancer. J Thorac Oncol. 2010;5(6 Suppl 2):S172–8.
Hirosawa T, Itabashi M, Ohnuki T, Yamaguchi N, Sugihara K, Kameoka S, et al. Prognostic factors in patients undergoing complete resection of pulmonary metastases of colorectal cancer: amulti-institutional cumulative follow-up study. Surg Today. 2013;43:494–9.
Shibutani M, Maeda K, Nagahara H, Noda E, Ohtani H, Nishiguchi Y, et al. Prognostic significance of the preoperative serum C-reactive protein level in patients with stage IV colorectal cancer. Surg Today. 2015;45:315–21.
Welter S, Jacobs J, Krbek T, Poettgen C, Stamatis G. Prognostic impact of lymph node involvement in pulmonary metastases from colorectal cancer. Eur J Cardiothorac Surg. 2007;31:167–72.
Hamaji M, Cassivi SD, Shen KR, Shen R, Allen M, Nichols FC, et al. Is lymph node dissection required in pulmonary metastasectomy for colorectal adenocarcinoma? Ann Thorac Surg. 2012;94:1796–800.
Garcia-Yuste M, Cassivi S, Paleru C. Thoracic lymphatic involvement in patients having pulmonary metastasectomy: incidence and the effect on prognosis. J Thorac Oncol. 2010;5(6 Suppl 2):S166–9.
Osarogiagbon RU, Yu X. Nonexamination of lymph nodes and survival after resection of non-small cell lung cancer. Ann Thorac Surg. 2013;96:1178–89.
Allen MS, Darling GE, Pechet TT, Mitchell JD, Herndon JE 2nd, Landreneau RJ, et al. Morbidity and mortality of major pulmonary resections in patients with early-stage lung cancer: initial results of the randomized, prospective ACOSOG Z0030 trial. Ann Thorac Surg. 2006;81:1013–9.
Maniwa T, Okumura T, Isaka M, Nakagawa K, Ohde Y, Kondo H. Recurrence of mediastinal node cancer after lobe-specific systematic nodal dissection for non-small-cell lung cancer. Eur J Cardiothorac Surg. 2013;44:e59–64.
Kamiyoshihara M, Hirai T, Kawashima O, Ishikawa S, Morishita Y. The surgical treatment of metastatic tumors in the lung: is lobectomy with mediastinal lymph node dissection suitable treatment? Oncol Rep. 1998;5:453–7.
Okumura S, Kondo H, Tsuboi M, Nakayama H, Asamura H, Tsuchiya R, et al. Pulmonary resection for metastatic colorectal cancer: experiences with 159 patients. J Thorac Cardiovasc Surg. 1996;112:867–74.
Treasure T, Fallowfield L, Lees B, Farewell V. Pulmonary metastasectomy in colorectal cancer: the PulMiCC trial. Thorax. 2012;67:185–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding source
The GECMP-CCR-SEPAR database and the statistic analyses were funded by Ethicon Endosurgery. The sponsor had no input in the design and analysis of this study or in the decision to publish it.
Conflict of interest
There are no conflicts of interest to report for any of the authors affiliated with this paper.
Additional information
On behalf of the Spanish Group of Lung Metastases of Colo-Rectal Cancer (GECMP-CCR) of the Spanish Society of Pneumology and Thoracic Surgery (SEPAR).
The members of “Spanish Group of Lung Metastases of Colo-Rectal Cancer (GECMP-CCR) of the Spanish Society of Pneumology and Thoracic Surgery (SEPAR)” are listed in Appendix
Appendix
Appendix
Members of the Spanish Group for Surgery of Lung Metastases from Colorectal Carcinoma GECMP-CCR-SEPAR:
Coordinators: Juan J. Rivas (Miguel Servet University Hospital, Zaragoza) and Laureano Molins (Sagrat Cor University Hospital, Barcelona).
Secretary: Raul Embún (Miguel Servet University Hospital, Zaragoza).
Local heads and departments: Francisco Rivas (H.U. de Bellvitge, Hospitalet de Llobregat, Barcelona); Raul Embún (H.U. Miguel Servet, Zaragoza); Jorge Hernández (H.U. Sagrat Cor, Barcelona); Félix Heras (H.G.U. de Valladolid); Javier de la Cruz (H.U. Virgen del Rocío, Sevilla); Matilde Rubio (H.U. Josep Trueta, Girona); Esther Fernández (H.U. Germans Trias i Pujol, Badalona, Barcelona); Miguel Carbajo (H.U. Marqués de Valdecilla, Santander); Rafael Peñalver (H.U. Gregorio Marañón, Madrid); José Ramón Jarabo (H.C. San Carlos, Madrid); Diego González-Rivas (C.H.U. de A Coruña); Sergio Bolufer (H.G.U. de Alicante); Carlos Pagés (H.G.U. Carlos Haya, Málaga); Sergi Call (H.U. Mutua Terrassa, Barcelona); David Smith (H. Italiano, Buenos Aires, Argentina); Richard Wins (H.C.U. de Valencia); Antonio Arnau (H.G.U. de Valencia); Andrés Arroyo (H.U. Virgen de la Arrixaca, Murcia); Ma Carmen Marrón (H.U. 12 de Octubre, Madrid); Akiko Tamura (Clínica U. de Navarra, Pamplona); Montse Blanco (C.H.U. de Vigo, Pontevedra); Beatriz de Olaiz (H.U. de Getafe, Madrid); Gemma Muñoz (H.U. Ramón y Cajal, Madrid); José M. García Prim (H.C.U. de Santiago de Compostela, A Coruña); Carlos Rombolá (H.G.U de Albacete); Santiago García Barajas (H.U. Infanta Cristina, Badajoz); Alberto Rodríguez (H.U. del Mar, Barcelona); Jorge Freixinet (H.U. Dr. Negrín, Las Palmas); Javier Ruiz (H.U. Virgen de las Nieves, Granada); Guillermo Carriquiry (H. Maciel, Universidad de la República, Montevideo, Uruguay); Moisés Rosenberg (Instituto Oncológico Alexander Fleming, Buenos Aires, Argentina); Emilio Canalís (H.U. Juan XXIII, Tarragona).
Rights and permissions
About this article
Cite this article
Call, S., Rami-Porta, R., Embún, R. et al. Impact of inappropriate lymphadenectomy on lung metastasectomy for patients with metastatic colorectal cancer. Surg Today 46, 471–478 (2016). https://doi.org/10.1007/s00595-015-1214-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-015-1214-3