Abstract
Purpose
An incisional surgical site infection (I-SSI) is a frequently observed complication following colorectal surgery. Intraoperative wound management is one of the most important factors that determine the incidence of postoperative I-SSI. The purpose of this study was to assess the impact of the methods used for intraoperative wound management on the incidence of I-SSI following elective surgery for colorectal cancer.
Methods
Between November 2009 and February 2011, the data of 1,980 consecutive patients who underwent elective colorectal resection for colorectal cancer were prospectively collected from 19 affiliated hospitals. The incidence of and risk factors for I-SSI were investigated.
Results
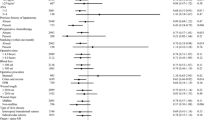
Overall, 233 I-SSIs were identified (11.7 %). Forty-two possible risk factors were analyzed. Using a multivariate analysis, the independent risk factors for I-SSI were identified to be a high body mass index, previous laparotomy, chronic liver disease, wound length, contaminated wound class, creation or closure of an ostomy, right hemicolectomy procedure, the suture material used for fascial closure and the incidence of organ/space SSI.
Conclusion
To prevent I-SSI following elective colorectal surgery, it is crucial to avoid making large incisions and reduce fecal contamination whenever possible. A high quality randomized control trial is necessary to confirm the definitive intraoperative procedure(s) that can minimize the incidence of I-SSI.
Similar content being viewed by others

Abbreviations
- ASA:
-
American Society of Anesthesia
- APR:
-
Abdominoperineal resection
- BMI:
-
Body mass index
- CDC:
-
The Centers for Disease and Control
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CT:
-
Computed tomography
- HAR:
-
High anterior resection
- ISR:
-
Internal sphincter resection
- I-SSI:
-
Incisional surgical site infection
- LAR:
-
Low anterior resection
- LHC:
-
Left hemicolectomy
- OR:
-
Odds ratio
- RCT:
-
Randomized control trial
- RHC:
-
Right hemicolectomy
- SSI:
-
Surgical site infection
- Sig:
-
Sigmoidectomy
References
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27:97–132.
Anderson DJ, Kaye KS, Classen D, Arias KM, Podgorny K, Burstin H, et al. Strategies to prevent surgical site infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29(Suppl 1):S51–61.
Konishi T, Watanabe T, Kishimoto J, Nagawa H. Elective colon and rectal surgery differ in risk factors for wound infection: results of prospective surveillance. Ann Surg. 2006;244:758–63.
Fujita S, Saito N, Yamada T, Takii Y, Kondo K, Ohue M, et al. Randomized, multicenter trial of antibiotic prophylaxis in elective colorectal surgery: single dose vs 3 doses of a second-generation cephalosporin without metronidazole and oral antibiotics. Arch Surg. 2007;142:657–61.
Fujii T, Tsutsumi S, Matsumoto A, Fukasawa T, Tabe Y, Yajima R, et al. Thickness of subcutaneous fat as a strong risk factor for wound infections in elective colorectal surgery: impact of prediction using preoperative CT. Dig Surg. 2010;27:331–5.
Kobayashi S, Ito M, Sugito M, Kobayashi A, Nishizawa Y, Saito N. Association between incisional surgical site infection and the type of skin closure after stoma closure. Surg Today. 2011;41:941–5.
Nakamura T, Kashimura N, Noji T, Suzuki O, Ambo Y, Nakamura F, et al. Triclosan-coated sutures reduce the incidence of wound infections and the costs after colorectal surgery: a randomized controlled trial. Surgery. 2013;153:576–83.
Romy S, Eisenring MC, Bettschart V, Petignat C, Francioli P, Troillet N. Laparoscope use and surgical site infections in digestive surgery. Ann Surg. 2008;247:627–32.
Smith RL, Bohl JK, McElearney ST, Friel CM, Barclay MM, Sawyer RG, et al. Wound infection after elective colorectal resection. Ann Surg. 2004;239:599–605.
Itani KM, Wilson SE, Awad SS, Jensen EH, Finn TS, Abramson MA. Ertapenem versus cefotetan prophylaxis in elective colorectal surgery. N Engl J Med. 2006;355:2640–51.
Blumetti J, Luu M, Sarosi G, Hartless K, McFarlin J, Parker B, et al. Surgical site infections after colorectal surgery: do risk factors vary depending on the type of infection considered? Surgery. 2007;142:704–11.
Tang R, Chen HH, Wang YL, Changchien CR, Chen JS, Hsu KC, et al. Risk factors for surgical site infection after elective resection of the colon and rectum: a single-center prospective study of 2,809 consecutive patients. Ann Surg. 2001;234:181–9.
Ortiz H, Armendariz P, Kreisler E, Garcia-Granero E, Espin-Basany E, Roig JV, et al. Influence of rescrubbing before laparotomy closure on abdominal wound infection after colorectal cancer surgery: results of a multicenter randomized clinical trial. Arch Surg. 2012;147:614–20.
Sorensen LT. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: a systematic review and meta-analysis. Arch Surg. 2012;147:373–83.
Darouiche RO, Wall MJ Jr, Itani KM, Otterson MF, Webb AL, Carrick MM, et al. Chlorhexidine-Alcohol versus Povidone-Iodine for Surgical-Site Antisepsis. N Engl J Med. 2010;362:18–26.
Young H, Knepper B, Moore EE, Johnson JL, Mehler P, Price CS. Surgical site infection after colon surgery: national healthcare safety Network risk factors and modeled rates compared with published risk factors and rates. J Am Coll Surg. 2012;214:852–9.
Fry DE. Preventive systemic antibiotics in colorectal surgery. Surg Infect (Larchmt). 2008;9:547–52.
Serra-Aracil X, Garcia-Domingo MI, Pares D, Espin-Basany E, Biondo S, Guirao X, et al. Surgical site infection in elective operations for colorectal cancer after the application of preventive measures. Arch Surg. 2011;146:606–12.
Rasic Z, Schwarz D, Adam VN, Sever M, Lojo N, Rasic D, et al. Efficacy of antimicrobial triclosan-coated polyglactin 910 (Vicryl* Plus) suture for closure of the abdominal wall after colorectal surgery. Coll Antropol. 2011;35:439–43.
McConnell YJ, Johnson PM, Porter GA. Surgical site infections following colorectal surgery in patients with diabetes: association with postoperative hyperglycemia. J Gastrointest Surg. 2009;13:508–15.
Sehgal R, Berg A, Figueroa R, Poritz LS, McKenna KJ, Stewart DB, et al. Risk factors for surgical site infections after colorectal resection in diabetic patients. J Am Coll Surg. 2011;212:29–34.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Weiss CA 3rd, Statz CL, Dahms RA, Remucal MJ, Dunn DL, Beilman GJ. Six years of surgical wound infection surveillance at a tertiary care center: review of the microbiologic and epidemiological aspects of 20,007 wounds. Arch Surg. 1999;134:1041–8.
Kobayashi M, Mohri Y, Tonouchi H, Miki C, Nakai K, Kusunoki M, et al. Randomized clinical trial comparing intravenous antimicrobial prophylaxis alone with oral and intravenous antimicrobial prophylaxis for the prevention of a surgical site infection in colorectal cancer surgery. Surg Today. 2007;37:383–8.
Hubner M, Diana M, Zanetti G, Eisenring MC, Demartines N, Troillet N. Surgical site infections in colon surgery: the patient, the procedure, the hospital, and the surgeon. Arch Surg. 2011;146:1240–5.
Aimaq R, Akopian G, Kaufman HS. Surgical site infection rates in laparoscopic versus open colorectal surgery. Am Surg. 2011;77:1290–4.
Manilich E, Vogel JD, Kiran RP, Church JM, Seyidova-Khoshknabi D, Remzi FH. Key factors associated with postoperative complications in patients undergoing colorectal surgery. Dis Colon Rectum. 2013;56:64–71.
Ortega G, Rhee DS, Papandria DJ, Yang J, Ibrahim AM, Shore AD, et al. An evaluation of surgical site infections by wound classification system using the ACS-NSQIP. J Surg Res. 2012;174:33–8.
Cima R, Dankbar E, Lovely J, Pendlimari R, Aronhalt K, Nehring S, et al. Colorectal surgery surgical site infection reduction program: a national surgical quality improvement program-driven multidisciplinary single-institution experience. J Am Coll Surg. 2013;216:23–33.
Mu Y, Edwards JR, Horan TC, Berrios-Torres SI, Fridkin SK. Improving risk-adjusted measures of surgical site infection for the national healthcare safety network. Infect Control Hosp Epidemiol. 2011;32:970–86.
Bull A, Wilson J, Worth LJ, Stuart RL, Gillespie E, Waxman B, et al. A bundle of care to reduce colorectal surgical infections: an Australian experience. J Hosp Infect. 2011;78:297–301.
Anthony T, Murray BW, Sum-Ping JT, Lenkovsky F, Vornik VD, Parker BJ, et al. Evaluating an evidence-based bundle for preventing surgical site infection: a randomized trial. Arch Surg. 2011;146:263–9.
Crolla RM, van der Laan L, Veen EJ, Hendriks Y, van Schendel C, Kluytmans J. Reduction of surgical site infections after implementation of a bundle of care. PLoS One. 2012;7:e44599.
Rosenberger LH, Politano AD, Sawyer RG. The surgical care improvement project and prevention of post-operative infection, including surgical site infection. Surg Infect (Larchmt). 2011;12:163–8.
Hodgson NC, Malthaner RA, Ostbye T. The search for an ideal method of abdominal fascial closure: a meta-analysis. Ann Surg. 2000;231:436–42.
van ‘t Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J. Meta-analysis of techniques for closure of midline abdominal incisions. Br J Surg. 2002;89:1350–6.
Diener MK, Voss S, Jensen K, Buchler MW, Seiler CM. Elective midline laparotomy closure: the INLINE systematic review and meta-analysis. Ann Surg. 2010;251:843–56.
Israelsson LA, Millbourn D. Closing midline abdominal incisions. Langenbecks Arch Surg. 2012;397:1201–7.
Seiler CM, Bruckner T, Diener MK, Papyan A, Golcher H, Seidlmayer C, et al. Interrupted or continuous slowly absorbable sutures for closure of primary elective midline abdominal incisions: a multicenter randomized trial (INSECT: ISRCTN24023541). Ann Surg. 2009;249:576–82.
Sajid MS, Parampalli U, Baig MK, McFall MR. A systematic review on the effectiveness of slowly-absorbable versus non-absorbable sutures for abdominal fascial closure following laparotomy. Int J Surg. 2011;9:615–25.
Justinger C, Moussavian MR, Schlueter C, Kopp B, Kollmar O, Schilling MK. Antibacterial [corrected] coating of abdominal closure sutures and wound infection. Surgery. 2009;145:330–4.
Justinger C, Schuld J, Sperling J, Kollmar O, Richter S, Schilling MK. Triclosan-coated sutures reduce wound infections after hepatobiliary surgery–a prospective non-randomized clinical pathway driven study. Langenbecks Arch Surg. 2011;396:845–50.
Galal I, El-Hindawy K. Impact of using triclosan-antibacterial sutures on incidence of surgical site infection. Am J Surg. 2011;202:133–8.
Wang ZX, Jiang CP, Cao Y, Ding YT. Systematic review and meta-analysis of triclosan-coated sutures for the prevention of surgical-site infection. Br J Surg. 2013;100:465–73.
Baracs J, Huszar O, Sajjadi SG, Horvath OP. Surgical site infections after abdominal closure in colorectal surgery using triclosan-coated absorbable suture (PDS Plus) vs. uncoated sutures (PDS II): a randomized multicenter study. Surg Infect (Larchmt) 2011; 12:483-9.
Chang WK, Srinivasa S, Morton R, Hill AG. Triclosan-impregnated sutures to decrease surgical site infections: systematic review and meta-analysis of randomized trials. Ann Surg. 2012;255:854–9.
Mullen JT, Davenport DL, Hutter MM, Hosokawa PW, Henderson WG, Khuri SF, et al. Impact of body mass index on perioperative outcomes in patients undergoing major intra-abdominal cancer surgery. Ann Surg Oncol. 2008;15:2164–72.
Haridas M, Malangoni MA. Predictive factors for surgical site infection in general surgery. Surgery. 2008;144:496–501.
Pessaux P, Msika S, Atalla D, Hay JM, Flamant Y. French Association for Surgical R. Risk factors for postoperative infectious complications in noncolorectal abdominal surgery: a multivariate analysis based on a prospective multicenter study of 4718 patients. Arch Surg. 2003;138:314–24.
van Dishoeck AM, Koek MB, Steyerberg EW, van Benthem BH, Vos MC, Lingsma HF. Use of surgical-site infection rates to rank hospital performance across several types of surgery. Br J Surg. 2013;100:628–36 (discussion 637).
Wilson J, Wloch C, Saei A, McDougall C, Harrington P, Charlett A, et al. Inter-hospital comparison of rates of surgical site infection following caesarean section delivery: evaluation of a multicentre surveillance study. J Hosp Infect. 2013;84:44–51.
Kao LS, Millas SG, Pedroza C, Tyson JE, Lally KP. Should perioperative supplemental oxygen be routinely recommended for surgery patients? A Bayesian meta-analysis. Ann Surg. 2012;256:894–901.
Acknowledgments
In addition to the authors listed on the title page, the following investigators participated in this study: Hitoshi Kubota, M.D., Handa City Hospital; Yuichiro Tojima, M.D., Social Insurance Chukyo Hospital; Yasuhiro Kurumiya, M.D., Toyota Kosei Hospital; Hiroshi Kono, M.D., Nagoya Ekisaikai Hospital; Hideo Yamamoto, M.D., Tokai Hospital; Kazuhisa Shirai, M.D., Yamashita Hospital; Satoaki Kamiya, M.D., Tsushima City Hospital; Akira Ishikawa, M.D., Chubu Rosai Hospital; Shinsuke Iyomasa, M.D., Yachiyo Hospital; Masaki Terasaki, M.D., Shizuoka Saiseikai General Hospital; Atsushi Morioka, M.D., Kumiai Kosei Hospital; and Makoto Kato, M.D., Kamiiida Daiichi General Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Itatsu, K., Sugawara, G., Kaneoka, Y. et al. Risk factors for incisional surgical site infections in elective surgery for colorectal cancer: focus on intraoperative meticulous wound management. Surg Today 44, 1242–1252 (2014). https://doi.org/10.1007/s00595-013-0677-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-013-0677-3