Abstract
Purpose
Laparoscopic hiatal hernia repair with additional fundoplication is a commonly recommended standard surgical treatment for symptomatic large hiatal hernias with paraesophageal involvement (PEH). However, due to the risk of persistent side effects, this method remains controversial. Laparoscopic mesh-augmented hiatoplasty without fundoplication (LMAH), which combines hiatal repair and mesh reinforcement, might therefore be an alternative.
Methods
In this retrospective study of 55 (25 male, 30 female) consecutive PEH patients, the perioperative course and symptomatic outcomes were analyzed after a mean follow-up of 72 months.
Results
The mean DeMeester symptom score decreased from 5.1 to 1.8 (P < 0.001) and the gas bloating value decreased from 1.2 to 0.5 (P = 0.001). The dysphagia value was 0.7 before surgery and 0.6 (P = 0.379) after surgery. The majority of the patients were able to belch and vomit (96 and 92 %, respectively). Acid-suppressive therapy on a regular basis was discontinued in 68 % of patients. In 4 % of patients, reoperation was necessary due to recurrent or persistent reflux. A mesh-related stenosis that required endoscopic dilatation occurred in 2 % of patients.
Conclusions
LMAH is feasible, safe and provides an anti-reflux effect, even without fundoplication. As operation-related side effects seem to be rare, LMAH is a potential treatment option for large hiatal hernias with paraesophageal involvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic fundoplication (LF) is recommended as an adjunct to the surgical treatment of symptomatic large hiatal hernias with paraesophageal involvement (PEH) [1–3]. However, there are a number of undesirable fundoplication-related side effects, such as gas bloating and dysphagia, which occur in up to 58 % of patients [4, 5]. Due to the presence of persistent side effects in about 20 % of patients, it is necessary to investigate whether PEH could be surgically treated without an additional fundoplication [6, 7]. An investigation of a simple laparoscopic mesh-augmented hiatoplasty without an additional fundoplication (LMAH) could answer this question.
Whether an adequate anti-reflux effect of LMAH can be achieved will depend on the reconstruction of the hiatus and the durable fixation of the esophagogastric junction below the diaphragm by mesh reinforcement, thereby lengthening the abdominal part of the esophagus. The latter is an important criterion for ensuring an adequate function of the lower esophageal sphincter [8].
The major problem associated with simple hiatoplasties in combination with some type of cardiopexy is that, while they provide a good anti-reflux effect in up to 90 % of cases, they have reflux recurrence rates of 60 % in the long term [9–11]. Styger et al. [3] have also shown that after repair of PEH without fundoplication, there was a new onset of gastroesophageal reflux in 32 % of patients. Consequently, cardiopexy procedures have been rejected in favor of fundoplication. However, all of these data originated from the time before mesh augmentation at the hiatus was used to prevent recurrences of hiatal hernias and the consequent gastroesophageal reflux. Therefore, recurrences after LMAH may be prevented by mesh augmentation even without additional fundoplication.
The aim of the present retrospective cohort study was to evaluate the feasibility, safety and efficiency of LMAH in terms of reflux control, side effects and recurrences after the treatment of PEH.
Methods
Patients
In the present retrospective follow-up study, the records of 55 consecutive patients who underwent LMAH for the repair of PEH at Bad Saulgau Hospital between July 1999 and July 2006 were reviewed for details on the perioperative course and the outcome after a long-term follow-up. All patients gave their informed consent. The patient characteristics are summarized in Table 1.
Preoperative assessment
Preoperatively, the patients were investigated for the type of hiatal hernia with an upper-gastrointestinal endoscopy in 47 (86 %) cases and/or a barium swallow in 39 (71 %) cases. Only large hiatal hernias defined as hernias with paraesophageal involvement (PEH) were included in the present study. Additionally, the patients were screened for evidence of gastroesophageal reflux disease (GERD), which was present in a total of 38 (69 %) patients, as confirmed by upper-gastrointestinal endoscopy in 28 (74 %) patients, by barium swallow in five (13 %) patients, by symptomatic voluminous reflux in three (8 %) patients and by a positive proton pump inhibitor test in two (5 %) patients. If apparent, esophagitis was graded according to the Savary and Miller or Los Angeles classification [12, 13]. The details of the hernias are given in Table 2. The main symptoms leading to the operation are summarized in Table 3.
Surgical technique
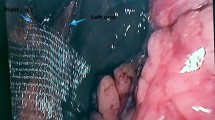
All procedures were performed as described previously [14]. All herniated structures were first repositioned (Fig. 1a). After incision of the lesser omentum and the peritoneum at the hiatus, the hernia sac was completely reduced. To identify the esophagus, a 32 Fr esophageal bougie was used. After complete mobilization of the hernia sac and the distal esophagus, the hiatus was narrowed with three to four non-absorbable, multifilament sutures (Fig. 1b), and a circular 8 × 8 cm heavyweight (85 g/m2) polypropylene mesh (Surgipro™, Tyco Healthcare, Neustadt, Germany) was applied from behind around the esophagus and fixed with 8–12 staples (Endo Universal™ 65°; Tyco Healthcare, Neustadt, Germany) towards the diaphragm (Fig. 1c). Finally, an anterior cardiophrenicopexy was routinely added with 5–7 non-absorbable, multifilament sutures (Fig. 1d).
The laparoscopic mesh-augmented hiatoplasty. a Repositioning of all herniated structures, mobilization of the hernia sac and the distal esophagus. b Crurorraphy: the hiatus is narrowed with 3–4 non-absorbable, multifilament sutures. c A circular 8 × 8 cm heavyweight polypropylene mesh is applied from behind around the esophagus, and fixed with staples towards the diaphragm. d An anterior cardiophrenicopexy is routinely added
Follow-up assessment
Forty-one of the 55 (75 %) patients were available for an objective follow-up (barium swallow and/or an upper-gastrointestinal endoscopy) after an average of 73 ± 26 (range 26–109) months. All patients received a standardized questionnaire (symptomatic follow-up), which was answered by 50 (91 %) patients after a mean of 72 ± 26 (range 25–109) months either by mail (n = 40), phone (n = 4) or during a follow-up examination (n = 6). All the questions focused on the time before the operation as well as the state at the time of the survey. The questionnaire included questions on reflux symptoms, such as heartburn and regurgitation, as well as side effects, such as dysphagia and gas bloating. The patients could rate their symptoms as none = 0, mild = 1, moderate = 2 and severe = 3. By adding up the values for heartburn, regurgitation and dysphagia, the DeMeester symptom score [15] was calculated. The total score ranged from 0 (no symptoms) to 9 (maximal symptoms). Treatment failure was defined according to the definition used by Lundell et al. [16]. One of the following criteria, therefore, had to be present: moderate or severe heartburn, moderate or severe acid regurgitation, esophagitis of at least grade II, the requirement of daily proton pump inhibitor (PPI) treatment or the need for reoperation because of GERD. Additionally, the symptomatic outcome was classified according to the modified Visick score (I = no symptoms; II = mild symptoms, no regular medication or physician’s help needed; III = significant symptoms, regular medication or physician’s help needed; IV = symptoms as bad as or worse than before surgery) [17]. The patients were asked whether they were able to belch and vomit, if they needed continuous PPI therapy, if endoscopy was necessary for any reason and if they had undergone a reoperation. Furthermore, the assessment included questions on the surgical success and the patients’ physical state. Finally, the patients were asked how satisfied they were with their surgical results and whether they would be willing to undergo the operation again.
Statistical analysis
The statistical analysis was performed using the SPSS 11.5 software program (SPSS Inc., Chicago, IL). The following tests were used: the Chi-square test or the Fisher exact test, as appropriate, for nominal data, and the Mann–Whitney U test and the Wilcoxon signed-rank test for comparisons of unrelated and related nonparametric data, respectively. The Spearman rank correlation was used for the correlation analysis. A two-sided P value <0.05 was considered to be statistically significant.
Results
Perioperative course
The mean length of the LMAH operation was 104 ± 67 (range 35–375) min. There was one (2 %; 95 % CI 0.3–13.0 %) intraoperative complication, with no need for conversion to open surgery. The patient had a gastric perforation, which had to be treated with a gastric wedge resection. Four of 55 (7 %; 95 % CI 2.4–17.7 %) patients had postoperative complications, including transient dysphagia (n = 2), delayed gastric emptying (n = 1) and a urinary tract infection (n = 1). The mortality rate was zero (95 % CI 0–7.8 %). The mean hospital stay was 8 ± 4 (range 4–25) days.
Long-term follow-up
Re-interventions and objective outcome
Using upper-gastrointestinal endoscopy, esophagitis and Barrett’s esophagus were each confirmed in three of 17 patients (18 %; 95 % CI 5.4–41.8 %). A sliding hiatal hernia was present in four of 41 patients, as confirmed by barium swallow and/or upper-gastrointestinal endoscopy, corresponding to an anatomical recurrence rate of 10 % (95 % CI 3.3–23.1 %). In three of 50 (6 %; 95 % CI 1.4–16.8 %) patients, a re-intervention was necessary. Two (4 %) of them were laparoscopically reoperated with the addition of a fundoplication due to reflux symptoms, and one needed endoscopic dilatation due to stenosis of the esophagus with severe dysphagia.
Symptomatic outcome
The DeMeester symptom score decreased from a preoperative score of 5.1 ± 2.1 to 1.8 ± 2.0 (P < 0.001) postoperatively. The reflux value decreased from 2.3 ± 0.9 to 0.6 ± 0.9 (P < 0.001).
According to the definition used by Lundell et al. [16], 17 of 50 (34 %; 95 % CI 22.4–47.9 %) patients showed a failure of reflux treatment. The details are given in Table 4. Sixteen of the 50 (32 %; 95 % CI 20.7–45.9 %) patients needed daily PPI treatment on a regular basis due to reflux symptoms. Regarding the side effects, the dysphagia value hardly changed, from 0.7 ± 1 to 0.6 ± 0.9 (P = 0.379). In terms of the gas bloating, a decrease was documented from 1.2 ± 1.2 to 0.5 ± 0.8 (P = 0.001). Two of the 50 (4 %; 95 % CI 0.3–14.2 %) patients who were available for follow-up reported an inability to belch, and four (8 %; 95 % CI 2.6–19.4 %) patients were unable to vomit. According to the Visick score, 19 of 50 (38 %) were classified as type I, 10 (20 %) patients as type II, 18 (36 %) patients as type III and 3 (6 %) patients as type IV.
Patients’ assessments
Forty of the 50 (80 %; 95 % CI 66.8–88.9 %) patients were satisfied with the result and would undergo LMAH again. Forty-one (82 %; 95 % CI 69.0–90.4 %) assessed the surgical result to be good or better, and 44 (88 %; 95 % CI 75.8–94.8 %) reported an improved physical state after LMAH. For details see Table 5.
Discussion
This study was planned to evaluate the feasibility, safety and efficiency of LMAH as a method to treat PEH without an additional fundoplication. In our study, the procedure could be performed at a reasonable time of 104 min on average. One (2 %) patient who had a gastric perforation without the need for conversion experienced complications during the surgical treatment. In our patient series, postoperative morbidity was observed in 7 % of patients and no postoperative mortality occurred. After an average of 72 months, 90 % of patients no longer had a PEH and two-thirds of patients were free of reflux symptoms. This is in line with the results of another prospective cohort study that was recently published by the last author. In that study, conducted at the cantonal hospital of St. Gallen/Switzerland, a significant decrease of reflux symptoms was shown 1 year postoperatively, with a recurrence rate of 9 % [14]. Thus, LMAH appears to be feasible and safe and to have an anti-reflux effect, even without fundoplication.
Based on the past and present experiences, it appears that an anti-reflux procedure during PEH repair is necessary to prevent hernia recurrence and postoperative gastroesophageal reflux. Allison [18] reviewed 421 of his own patients following hiatal hernia repair by hiatoplasty without fundoplication. Twenty-two years later, hiatal hernias or the presence of reflux were radiologically confirmed in 49 % after sliding hiatal hernia repair, and in 33 % after PEH repair. Styger et al. [3] reported a new occurrence of reflux in 32 % of patients after a repair of PEH without fundoplication, an observation which was also confirmed by other authors [19, 20]. On the other hand, in a non-randomized comparative study, Williamson et al. [7] presented a nearly identical reflux rate of 19 % without and 16 % with fundoplication. However, in both studies, the presence of a selection bias cannot be ruled out. The uncertainty regarding the need for a fundoplication in the repair of PEH is also illustrated by the fact that different patient groups, despite consistent fundoplication, have had postoperative reflux rates of 8–15 % [21–24]. In addition, in contrast to other patient groups, in which the fundoplication was only performed in patients with proven reflux, postoperative reflux was observed in 2–10 % of patients [25–29].
However, all of the publications mentioned above date to the time before mesh patches were available for reinforcement at the hiatus. In our opinion, the option of mesh augmentation at the hiatus, which has been proven to reduce the recurrence of hiatal hernias, justifies a re-evaluation of the need for a fundoplication during PEH repair [23, 30, 31]. Allison [18] reported a steady increase in recurrences in the years following simple hiatoplasties. In contrast, upon evaluating 306 patients following LMAH for GERD and sliding hiatal hernias, we observed no increase in the treatment failure after the first year [32]. The overall rate of anatomical hernia recurrence was 10 % in the present study. Recurrence rates of up to 42 % were seen with simple, primary suture repair of the hiatus in the previous studies [1, 31, 33]. Therefore, we feel that consistent mesh application is the best way to prevent recurrences after PEH repair, and that the procedure can be successful in the majority of cases, even without fundoplication.
Notably, the anti-reflux effect of LMAH does not appear to be as good as that of LF. In our study, one-third of the patients showed a failure of the treatment according to the definition provided by Lundell et al. [16], and two of these patients decided to undergo a reoperation due to reflux symptoms. When a reoperation is demanded because of persistent or new-onset GERD, we propose that fundoplication should be added to LMAH as a second-step procedure, as was done in the two patients who underwent reoperations in our cohort. Thus, a combination of LMAH and fundoplication seems to be the best option for the surgical treatment of PEH in terms of prevention of anatomical recurrence and postoperative reflux. However, the question remains whether the results are better with an additional fundoplication in terms of side effects and quality of life. This issue can only be resolved by future randomized controlled trials.
In our study, about 80 % of the patients were satisfied with their results, and almost 90 % reported that their condition had improved or normalized. About 80 % of the patients would undergo this operation again, and referred to the outcome of LMAH as good as or better than before the surgery. Regarding the side effects of LMAH, a significant decrease in gas bloating after surgery was noted. Only 8 % of patients were not able to vomit after surgery, and 4 % of patients reported that they could not belch. In studies with the main focus on side effects in the long-term follow-up after fundoplication, rates of gas bloating of 34 and 60 %, and rates of the inability to belch of 29 and 74 % were reported [4, 6, 34]. Similarly, more than 20 % of the patients were found to be unable to belch in the study reported by Lundell et al. [16]. Therefore, it can be assumed that LMAH has less negative effects, such as gas bloating, in comparison to LF. Regarding dysphagia, we found that 8 % of patients had serious complaints in our series without fundoplication. This value is not surprising, since dysphagia is a common problem associated with all forms of hiatoplasty, which is generally performed in combination with a fundoplication. In agreement with this, Granderath et al. [35] stated that dysphagia is more a problem of the narrowing of the hiatus than of the fundoplication itself. Consequently, it cannot be expected that the problem of dysphagia will be completely resolved by LMAH, but it could possibly be reduced by using calibration tubes larger than the 32 Fr tubes used in the present study.
LMAH implies that there is consistent mesh application at the hiatus. Therefore, one important factor to consider is mesh-related complications, such as erosions, migrations and stenoses. In our study, only one (2 %) patient experienced a relevant mesh-related complication, which was a stenosis of the esophagus that could be endoscopically dilated. Stadlhuber et al. [36] published a case series identifying 28 patients with mesh-related complications after hiatal repair. However, the true rate of mesh-related complications is unknown. Pooling all Medline-listed patient series from 1997 until 2009 with at least one mesh-related complication (n = 2392), 22 mesh-related complications were reported [32, 33, 37–42]. This correlates to a mesh-related complication rate of 0.9 %. In accordance with this finding, Targarona et al. [43] considered mesh reinforcement at the hiatus to be a safe procedure.
In summary, LMAH is a feasible and safe method to treat PEH. It seems that a durable anatomical reconstruction and a certain anti-reflux effect can also be achieved without fundoplication, with the benefit of fewer side effects. However, the procedure also has some drawbacks, such as the persistence or new onset of reflux and the risk of dysphagia. It is currently not possible to draw a final conclusion as to whether a fundoplication during PEH repair is necessary or not. Nevertheless, the present results warrant a randomized controlled trial evaluating the need for a fundoplication during mesh-augmented PEH repair in terms of reflux control, patient satisfaction and quality of life.
References
Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, et al. Laparoscopic repair of large type III hiatal hernia: objective follow-up reveals high recurrence rate. J Am Coll Surg. 2000;190:553–60.
Soper NJ. Laparoscopic management of hiatal hernia and gastroesophageal reflux. Curr Probl Surg. 1999;36:765–838.
Styger S, Ackermann C, Schuppisser JP, Tondelli P. Reflux disease following gastropexy for para-esophageal hiatal hernia. Schweiz Med Wochenschr. 1995;125:1213–5.
Catarci M, Gentileschi P, Papi C, Carrara A, Marrese R, Gaspari AL, et al. Evidence-based appraisal of antireflux fundoplication. Ann Surg. 2004;239:325–37.
Heikkinen TJ, Haukipuro K, Bringman S, Ramel S, Sorasto A, Hulkko A. Comparison of laparoscopic and open Nissen fundoplication 2 years after operation. A prospective randomized trial. Surg. Endosc. 2000;14:1019–23.
Booth MI, Jones L, Stratford J, Dehn TC. Results of laparoscopic Nissen fundoplication at 2–8 years after surgery. Br J Surg. 2002;89:476–81.
Williamson WA, Ellis FH Jr, Streitz JM Jr, Shahian DM. Paraesophageal hiatal hernia: is an antireflux procedure necessary? Ann Thorac Surg. 1993;56:447–51.
Bonavina L, Evander A, DeMeester TR, Walther B, Cheng SC, Palazzo L, et al. Length of the distal esophageal sphincter and competency of the cardia. Am J Surg. 1986;151:25–34.
Allison PR. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg. Gynecol. Obstet. 1951;92:419–31.
Hill LD. An effective operation for hiatal hernia: an eight year appraisal. Ann Surg. 1967;166:681–92.
Janssen IM, Gouma DJ, Klementschitsch P, van der Heyde MN, Obertop H. Prospective randomized comparison of teres cardiopexy and Nissen fundoplication in the surgical therapy of gastro-oesophageal reflux disease. Br J Surg. 1993;80:875–8.
Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–80.
Savary M, Miller G. The oesophagus. Handbook and atlas of endoscopy. Solothurn, Switzerland: Gassmann; 1978. p. 119–59.
Muller-Stich BP, Linke GR, Borovicka J, Marra F, Warschkow R, Lange J, et al. Laparoscopic mesh-augmented hiatoplasty as a treatment of gastroesophageal reflux disease and hiatal hernias-preliminary clinical and functional results of a prospective case series. Am J Surg. 2008;195:749–56.
DeMeester TR, Johnson LF, Joseph GJ, Toscano MS, Hall AW, Skinner DB. Patterns of gastroesophageal reflux in health and disease. Ann Surg. 1976;184:459–70.
Lundell L, Miettinen P, Myrvold HE, Hatlebakk JG, Wallin L, Malm A, et al. Seven-year follow-up of a randomized clinical trial comparing proton-pump inhibition with surgical therapy for reflux oesophagitis. Br J Surg. 2007;94:198–203.
Peterli R, Merki L, Schuppisser JP, Ackermann C, Herzog U, Tondelli P. Postcholecystectomy complaints one year after laparoscopic cholecystectomy. Results of a prospective study of 253 patients. Chirurg. 1998;69:55–60.
Allison PR. Hiatus hernia: (a 20-year retrospective survey). Ann Surg. 1973;178:273–6.
Treacy PJ, Jamieson GG. An approach to the management of para-oesophageal hiatus hernias. Aust N Z J Surg. 1987;57:813–7.
Willekes CL, Edoga JK, Frezza EE. Laparoscopic repair of paraesophageal hernia. Ann Surg. 1997;225:31–8.
Champion JK, Rock D. Laparoscopic mesh cruroplasty for large paraesophageal hernias. Surg Endosc. 2003;17:551–3.
Krahenbuhl L, Schafer M, Farhadi J, Renzulli P, Seiler CA, Buchler MW. Laparoscopic treatment of large paraesophageal hernia with totally intrathoracic stomach. J Am Coll Surg. 1998;187:231–7.
Muller-Stich BP, Holzinger F, Kapp T, Klaiber C. Laparoscopic hiatal hernia repair: long-term outcome with the focus on the influence of mesh reinforcement. Surg Endosc. 2006;20:380–4.
Swanstrom LL, Jobe BA, Kinzie LR, Horvath KD. Esophageal motility and outcomes following laparoscopic paraesophageal hernia repair and fundoplication. Am J Surg. 1999;177:359–63.
Ellis FH Jr, Crozier RE, Shea JA. Paraesophageal hiatus hernia. Arch Surg. 1986;121:416–20.
Geha AS, Massad MG, Snow NJ, Baue AE. A 32-year experience in 100 patients with giant paraesophageal hernia: the case for abdominal approach and selective antireflux repair. Surgery. 2000;128:623–30.
Myers GA, Harms BA, Starling JR. Management of paraesophageal hernia with a selective approach to antireflux surgery. Am J Surg. 1995;170:375–80.
Pitcher DE, Curet MJ, Martin DT, Vogt DM, Mason J, Zucker KA. Successful laparoscopic repair of paraesophageal hernia. Arch Surg. 1995;130:590–6.
Rakic S, Pesko P, Dunjic MS, Gerzic Z. Paraoesophageal hernia repair with and without concomitant fundoplication. Br J Surg. 1994;81:1162–3.
Frantzides CT, Madan AK, Carlson MA, Stavropoulos GP. A prospective, randomized trial of laparoscopic polytetrafluoroethylene (PTFE) patch repair vs simple cruroplasty for large hiatal hernia. Arch Surg. 2002;137:649–52.
Granderath FA, Schweiger UM, Kamolz T, Asche KU, Pointner R. Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg. 2005;140:40–8.
Muller-Stich BP, Koninger J, Muller-Stich BH, Schafer F, Warschkow R, Mehrabi A, et al. Laparoscopic mesh-augmented hiatoplasty as a method to treat gastroesophageal reflux without fundoplication: single-center experience with 306 consecutive patients. Am J Surg. 2009;198:17–24.
Zaninotto G, Portale G, Costantini M, Fiamingo P, Rampado S, Guirroli E, et al. Objective follow-up after laparoscopic repair of large type III hiatal hernia. Assessment of safety and durability. World J Surg. 2007;31:2177–83.
Spechler SJ, Lee E, Ahnen D, Goyal RK, Hirano I, Ramirez F, et al. Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: follow-up of a randomized controlled trial. JAMA. 2001;285:2331–8.
Granderath FA, Schweiger UM, Kamolz T, Pointner R. Dysphagia after laparoscopic antireflux surgery: a problem of hiatal closure more than a problem of the wrap. Surg Endosc. 2005;19:1439–46.
Stadlhuber RJ, Sherif AE, Mittal SK, Fitzgibbons RJ Jr, Michael BL, Hunter JG, et al. Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc. 2009;23:1219–26.
Baladas HG, Smith GS, Richardson MA, Dempsey MB, Falk GL. Esophagogastric fistula secondary to Teflon pledget: a rare complication following laparoscopic fundoplication. Dis Esophagus. 2000;13:72–4.
Carlson MA, Condon RE, Ludwig KA, Schulte WJ. Management of intrathoracic stomach with polypropylene mesh prosthesis reinforced transabdominal hiatus hernia repair. J Am Coll Surg. 1998;187:227–30.
Dally E, Falk GL. Teflon pledget reinforced fundoplication causes symptomatic gastric and esophageal lumenal penetration. Am J Surg. 2004;187:226–9.
Griffith PS, Valenti V, Qurashi K, Martinez-Isla A. Rejection of Goretex mesh used in prosthetic cruroplasty: a case series. Int. J. Surg. 2008;6:106–9.
Trus TL, Bax T, Richardson WS, Branum GD, Mauren SJ, Swanstrom LL, et al. Complications of laparoscopic paraesophageal hernia repair. J. Gastrointest. Surg. 1997;1:221–7.
Zilberstein B, Eshkenazy R, Pajecki D, Granja C, Brito AC. Laparoscopic mesh repair antireflux surgery for treatment of large hiatal hernia. Dis Esophagus. 2005;18:166–9.
Targarona EM, Bendahan G, Balague C, Garriga J, Trias M. Mesh in the hiatus: a controversial issue. Arch Surg. 2004;139:1286–96.
Conflict of interest
All the authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
G.R. Linke and T. Gehrig contributed equally to this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Linke, G.R., Gehrig, T., Hogg, L.V. et al. Laparoscopic mesh-augmented hiatoplasty without fundoplication as a method to treat large hiatal hernias. Surg Today 44, 820–826 (2014). https://doi.org/10.1007/s00595-013-0609-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-013-0609-2