Abstract
Aims
Common Psychiatric Disorders (CPDs) are associated with the development of overweight and obesity, the strongest risk factors for the onset and maintenance of Type 2 Diabetes mellitus (T2D). To the best of our knowledge, this is the first study to assess the prevalence of CPDs in patients with T2D in Italy.
Methods
This is a monocentric cross-sectional study; n = 184 T2D patients were screened for CPDs using the Patient Health Questionnaire (PHQ). Primary outcome was to evaluate the prevalence of CPDs. To assess association between CPDs and risk factors, we have utilized univariable logistic regression models.
Results
64.1% were men, median age was 67 (59–64) and median BMI 27 (25–30) kg/m2. The 42.9% tested positive for one or more mental disorders, 25.6% for depression. Patients with higher BMI (p = 0.04) had an increased likelihood of testing positive to the PHQ. Patients who had implemented lifestyle changes (p < 0.01) and were aware that mental health is linked to body health (p = 0.07) had a reduction in the likelihood of testing positive.
Conclusions
Prevalence of CPDs in T2D patients is higher than in the general population. Since CPDs favor the onset and subsistence of T2D, integrated diabetic-psychiatric therapy is required for improvement or remission of T2D in patients with comorbid CPDs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Across the world, both Diabetes and Psychiatric disorders are on the rise [1, 2]. A global Diabetes epidemic is ongoing, with 537 million of adult people currently affected, which is expected to reach 783 million by 2045 [1]. Diabetes strongly affects disability, mortality, and global health expenditure. It absorbs the 12% of global health expense [3] and has caused about 6.7 million deaths in 2021 [1]; Covid-19 in two years has caused 5.7 million of deaths [4]. Diabetes is one of the most important risk factors for cardiovascular disease, increasing cardiovascular risk in two- to fourfold [5], is the leading cause of blindness [6], chronic renal failure and dialysis [7], and of non-traumatic amputation of the lower limbs [8].
Type 2 Diabetes mellitus (T2D) determines the 95% of all cases of diabetes in the world [9]. In Italy, over 3 million 200 thousand people are affected by diabetes, 5.3% of the entire population [10].
About psychiatric disorders worldwide, it is estimated that 17.6% of population experienced a CPDs [11], and 4.4% suffer from depressive disorder [12].
Depression is the leading cause of disability worldwide [12], and over 700.000 people die due to suicide every year being the fourth leading cause of death in people aged 15–29 [13]. In primary care, in patients with physical illnesses, depression is one of the most frequent causes of consultation [14].
In Italy, 5.4% of the population suffer from a depressive disorder [15]and 7.3% experience a CPDs [16].
Regarding the connection between CPDs and T2D, it is recognized that CPDs are associated with the development of overweight and obesity[17], the strongest risk factors for the development of T2D [18,19,20].As the worldwide prevalence of both diabetes and mental health problems is increasing rapidly and is expected to do it further in the upcoming years [1] and given the link between these two classes of diseases, it is urgent to have studies evaluating the epidemiological situation of CPDs in patients with T2D.
The aim of this study was to assess the prevalence of the CPDs in patients with T2D, in a sample of patients numerically representative of the Italian population. Furthermore, we hypothesized that it would have been possible to identify factors that favor the positivity for a psychiatric disorder in the analyzed population. To the best of our knowledge, this is the first study to assess the prevalence of the CPDs in patients with T2D, in a sample of patients numerically representative of the Italian population.
Subjects, materials and methods
Monocentric cross-sectional study, conducted at the Fondazione Policlinico Universitario Agostino Gemelli IRCCS, UCSC, Rome, Italy (FPUAG).
A full description of the protocol used in the present study is provided in the Online Resource 1.
In brief, between October 2020 and November 2021 a sample of consecutive outpatient clinic attendees with T2D at the Diabetes Care Unit of the FPUAG was invited to participate in the study, with the aim of including 184 people with T2D.
Inclusion/exclusion criteria
Inclusion criteria were age between 18 and 85 years and diagnosis of T2D [21]. Exclusion criteria were diagnosis of Type 1 Diabetes mellitus (T1D); inability to complete the survey tools because of cognitive difficulties; to be very sick and unable to read and understand Italian. Women who were pregnant or had given birth in the last 6 months were also excluded.
Prior to interview, the site investigators fulfilled an information form for each patient. This form included socio-demographic information such as age, gender, civil status, residence location, educational level, and smoke status. T2D-specific information and anthropometric profile have been registered: duration of T2D, height, weight and BMI at diagnosis of T2D; actual height weight and BMI; antidiabetic drugs or insulin prescription; family history of T2D and history of T2D complications (cardiovascular disease, retinopathy, peripheral neuropathy, and renal disease); hypertension. Measurements of blood pressure, HbA1c, were also recorded. A section on past psychiatric history and on awareness of the importance of lifestyle changes and of mental health with respect to weight control and the prevention of physical diseases is also contained within the form; for more details, see Online resource 2. The patient's medical history was obtained before the PHQ administration to adequately attribute the presence of any physical symptoms to a medical condition or to the somatoform disorder. Any prescribed medicine for mental health problem was noted, as was any diagnosis or therapy of any psychiatric disorder. Patients were queried if they lived in a rural or an urban area and declared their highest level of education. Marital status was defined as married/co-habiting vs being single/widowed/divorced.
Each participant was requested to complete the Patient Health Questionnaire. The Italian full version of the PHQ [22] was used for psychiatric screening, as it covers the CPDs. The PHQ is a self-administered questionnaire that allows to evaluate the presence of specific disorders: major depressive disorder, other depressive disorders, panic attack disorder, other anxiety disorders, bulimia nervosa, binge eating disorder, dependence or alcohol abuse.
In this study, all the sections, from 1 to 11, of the official Italian version of the PHQ were used.
Subjects diagnosed with any psychiatric disorders were directed to consult their physician or the Psychiatric Unit of FPUAG for further evaluation and treatment.
Ethical approval
The study protocol was approved by the Ethics Committee (EC) of the FPUAG Università Cattolica del Sacro Cuore, on 08/08/2020 with number ID 3298 and protocol number 0040703/20. All procedures performed in the study were in accordance with the ethical standards of the institutional committee and with the Declaration of Helsinki and its later amendments. All participants signed a written informed consent form.
Statistical analysis
Sample size calculation was performed assuming an expected prevalence of psychiatric disorders of 37.5%, setting up an accuracy of 7% and a confidence level of 97%, thus calculating 184 patients to administer the PHQ. The expected prevalence was estimated from a previous study carried out in T2D patients [23].
Included patients were described in clinical and demographic characteristics through descriptive statistics techniques. Continuous variables had been checked for normality with Shapiro–Wilk test. Therefore, normally distributed data were expressed as mean and standard deviation (SD), and non-normally with median and first and third quartiles (q1–q3). Dichotomous variables, categorical variables, and scores were expressed as numbers and percentages.
Primary outcome was the prevalence of common psychiatric disorders in patients with T2D assessed through the Patient Health Questionnaire.
To evaluate potential risk/protective factors associated with patients’ psychiatric disorders positivity, we performed univariable logistic regression models. For each factor, we calculated the Odds Ratio (OR) with 95% Confidence Interval (CI) of being positive to PHQ. Statistical analyses were performed with Stata software, and statistical significance cut-off was set p < 0.05.
Data availability
The data associated with the study are available from the corresponding author on reasonable request.
Results
The results are based on the analysis of 240 patients enrolled in the study (Fig. 1-Online resource 3).
A total of 240 individuals recruited with T2D, agreed to participate in the study, with a response rate of 80%. The main reason for not participating was being too busy to undergo the examination; furthermore, 31 patients were excluded due to uncertain T2D diagnosis, whereas other 25 were excluded because they left the PHQ incomplete. Thus, 184 patients were analyzed.
Baseline characteristics
The demographic characteristics of the patients interviewed are reported in Table 1. Patients were 118 men (64.1%) and 66 women (35.9%), the median age was 67 years (q1–q3: 59–64), and 139 were married/co-habiting (75.5%). About the residence location, 116 (63.1%) were living in Urban location, while 68 (36.9%) in rural area. It was also recorded that patients had an average 11-year study education (± 4 years of study) and 162 (88.0%) were no current smoker.
The population evaluated have (Table 2): T2D on average from 10 years (q1–q3: 5–17). The median weight recorded was 80 kg (69–87) with a median height of 170 cm (162–176), median BMI 27 kg/m2 (25–30), of which 53 patients (28.8%) had a BMI in the obesity range. The weight and BMI of the patients at the time of T2D diagnosis were also collected and were: median weight 80 kg (q1–q3: 70–92) median BMI: 29 kg/m2 (25–31), of which 73 patients (39.7%) had a BMI in the obesity range. Additional values collected at the time of test administration were: median HbA1c and pharmacological therapy. Patients had median HbA1c of 6.8 (q1–q3: 6.1–7.6), 51 mmol/mol, and 146 patients (79.4%) were taking some type of oral and injectable (non-insulin) antidiabetic agents for the treatment of T2D, while 64 (34.8%) patients were taking insulin. A total number of 118 (64.1%) persons have at the time of the interview at least one complication related to T2D: 81 (44%) patients have CVD, 32 (17.4%) had neuropathy, 57 (40%) patients have retinopathy, 27 (14.7%) patients have Chronic Kidney Disease (CKD), and 140 (76.1%) suffer from hypertension.
Patient health questionnaire results
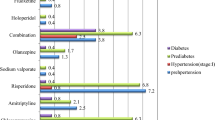
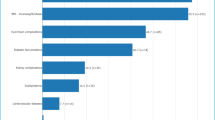
The prevalence of the different psychiatric disorders evaluated through the PHQ is provided in Fig. 1–2 and Table 3.
Of the sample examined, 79 people out of 184 tested positives for the PHQ, namely 42.9%, and 25.6% tested positive for a depressive disorder (percentage derived from the sum of Other Depressive Syndrome and Major Depressive Syndrome). The last question of the PHQ is: "If you checked off any problems on this questionnaire, how difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?" to this question alternatives answer are: not difficult at all, somewhat difficult, very difficult, extremely difficult. 144 (78.3%) patients answered: not difficult at all.
In addition to the collection of socio-demographic data, and to the administration of the PHQ, patients were asked about their awareness of the importance of weight loss in the remission of T2D [24, 25] and if they “are aware about the importance of mental health in controlling body weight and in prevention of physical diseases?”.
On the importance of lifestyle changes in the T2D remission, 174 people (94.6% of patients) replied that they received this information from their treating physician, while the percentage dropped to 134 patients (72.8%) when they were asked if, besides the importance of physical health, they know the importance of mental health in body weight control and prevention of physical diseases.
The patients were also asked whether they presented a psychiatric diagnosis in medical history, or if they had ever been treated by a psychiatrist or a psychotherapist and/or if they ever took psychopharmacological treatments in the past. The 46 patients (25.0%) had been treated by a psychiatrist or psychotherapist, and among them, 38 patients (20.6%) had undertaken psychopharmacological treatments.
Factors associated with positivity to the PHQ
Demographic and lifestyle predictors of current common psychiatric disorder are shown in Table 4 in Online resource 3.
Among all demographic and lifestyle variables we have analyzed, our results showed that female in comparison with males had 72% higher probability of testing positive to PHQ (OR = 1.72; 95%CI: 0.94–3.17), even if the result was not significant (p = 0.08). For every increase of 1 year in patients’ age, we noticed a 2% of reduction in developing positivity to the questionnaire (OR = 0.98; 95%CI: 0.95–1.00), but the result is not statistically significant (p = 0.07). BMI is a risk factor associated with a greater likelihood of testing positive for PHQ, indeed for every 1-point increase in current BMI there is a 7% increased risk (OR = 1.07; 95%CI: 1.00–1.14, p = 0.04), and for every 1-point increase in BMI at diagnosis the OR is equal to 1.05 (95%CI: 1.00–1.10, p = 0.06). Urban residence location, in comparison with rural, showed a 42% probability reduction in association with CPDs (OR = 0.58; 95%CI: 0.31–1.06), but it was not statistically significant (p = 0.07). Civil status and educational level did not show significant results.
Diabetes specific and psychosocial predictors of current common psychiatric disorder are shown in Table 5–6 in Online resource 3. Among those, antidiabetic drugs (non-insulin) use was associated with a 30% reduction in probability of having some common psychiatric disorder (OR = 0.70; 95%CI:0.34–1.43, p = 0.32), but the result was not statistically significant. Patients taking insulin, in comparison with patients that did not, had an 89% increase in the likelihood of testing positive to the PHQ (OR = 1.89; 95%CI: 1.02–3.49, p = 0.04), and this finding is likely related to the severity of the diabetic disease. Other interesting results are that patients who had implemented lifestyle changes showed a 62% odds reduction in being diagnosed of psychiatric disorders (OR = 0.38; 95%CI: 0.18–0.79, p < 0.01), patients who are aware that mental health is linked to body health had a 46% odds reduction (OR = 0.54; 95%CI: 0.28–1.04, p = 0.07), and patients who had Previous or actual Pharmaco-PSY treatment had a 246% probability increase in testing positive to the PHQ (OR = 2.46; 95%CI: 1.19–5.12, p = 0.02).
Discussion
We have observed substantial rates of mental health problems, that is, the 43% of patients treated at the FPUAG Diabetes Care Unit tested positive for a CPDs. The most common disorders detected were depressive syndrome, in almost 26% of patients, anxiety syndromes (11.4%) and binge eating (10.3%). Other psychiatric disorders less frequently present were: bulimia (4.3%), alcohol abuse (3.3%), somatoform disorder (3.3%), panic syndrome (1.6%).
The risk factors probably associated with the positivity to the test were: female sex, higher BMI, insulin intake, previous psychopharmacological treatment. Protective factors were aging, lifestyle changes implementation, awareness that mental health is related to body health.
Patients taking insulin and patients with higher BMI showed a statistically significant increase in the odds of testing positive for PHQ. These findings could suggest that people with psychiatric disorders are less able to adhere to prescriptions for T2D therapy and remission [26].
Other interesting results were that patients who had implemented lifestyle changes (p < 0.01) and patients who were aware that mental health is linked to body health were less likely to test positive to the PHQ, while patients who had previous or actual psychopharmacological treatment had a 246% probability increase in testing positive to the PHQ. These data seem to confirm that patients who were not affected by a mental disorder and were aware that mental health is linked to body health showed better adherence to lifestyle changes and therapies necessary for T2D treatment and remission.
Furthermore, the proportion of the DIA2PSI sample who had been or was still being treated by a mental health professional was 25%. At least 18% of the sample was neither diagnosed nor treated for a psychiatric disorder. These data confirm that people with T2D are underdiagnosed and undertreated for psychiatric disorders [26].
It is important to assess the prevalence of CPDs in T2D patients as it is recognized that a wide range of psychiatric disorders have a higher prevalence in subjects with T2D than in the general population [27]. Furthermore, most of the studies so far have focused their attention on the coexistence of T2D and depression, not evaluating other CPDs [28]. DIA2PSI is one of the few studies to address this topic. DIA2PSI results on depression are in line with other studies in the literature which found that depressive disorders are more common in people with T2D than in the general population [29]. Indeed, we have observed substantial higher rate of CPDs and depression in T2D patients (42.9% and 29%) then in the general Italian population (17.6% and 4.4%). Instead, making a comparison between the results of our study and other studies that have evaluated the presence of eating disorders, anxiety disorders, somatoform disorder and alcohol abuse in patients with T2D is difficult because studies on this type of disorders are rare in the literature [17, 27, 28]. In particular, lack of studies evaluating eating disorders appears quite surprising given that overeating is one of the fundamental factors underlying the onset and maintenance of T2D [18, 19].
It is necessary to assess psychiatric comorbidity in patients with T2D since CPDs are able to induce overweight, obesity the strongest risk factors for T2D [17,18,19]. Clinical trials have shown that weight loss ≥ 15% is necessary in the first years of T2D diagnosis to achieve disease remission [24, 25]. Nevertheless, the incidence of T2D remission in routine care settings is infrequent (< 1%) [30], in particular in patients with depressive symptoms [31]. Indeed, depression favors weight gain and determines a 60% increased risk of developing T2D [32,33,34] directly through three of its symptoms that we have re-named Bridge Symptoms (BS): alteration of eating behavior [35, 36], reduced physical activity [37, 38] and inadequate sleep duration [39, 40].
Also in CPDs, Bridge Symptoms are present increasing the risk of developing T2D [17]. In both depression and CPDs, there are other pathological mechanisms that can lead to increased risk of developing T2D: systemic chronic inflammation, increased insulin resistance, decreased insulin release from pancreatic beta cells and cognitive mechanisms like decreased ability to think and to focus, anhedonia, weariness, and lack of motivation that negatively affect the probability of attending medical examination and check-up or sustaining a physically active lifestyle [17].
Furthermore, people with T2D are responsible for much of the management of their disease,but if they have depressive symptoms, these lead to poor self-managementand early development of negative outcomes including early mortality [26, 41].
Conclusions
Performing psychiatric screening in patients with T2D is needed to intercept cases of mental disorder that might otherwise remain unknown and to intervene on the development of T2D and its remission, considering how CPDs favor its onset and maintenance [17, 30, 42]. This could help reduce the T2D epidemic, driving a reduction in Years of Life Lost (YLL) given that Diabetes is the 9th cause of death worldwide, and it is an important contributing cause to the first and second cause of death globally (ischemic heart disease and stroke).
Moreover, this can lead to substantial economic savings given that T2D absorbs 12% of global health expenditure [3].
Limitations
The population analyzed was mainly Caucasian, which limits generalization to non-Caucasian populations such as South Asians, who tend to develop T2D with less weight gain. Quality and robustness of our findings are limited by cross-sectional study design, restricted sample size, monocentric study, and the lack of multivariable analysis. Also, as with any diagnostic test, the PHQ does not detect all cases of mental disorders.
Data availability
The data associated with the study are available from the corresponding author on reasonable request.
References
International Diabetes mellitus Federation (2021) IDF Diabetes atlas—10th edition. https://diabetesatlas.org/#:~:text=Diabetes%20around%20the%20world%20in%202021%3A,%2D%20and%20middle%2Dincome%20countries. (Accessed 09 Jul 2022).
WHO (2022) Mental Health. https://www.who.int/health-topics/mental-health#tab=tab_2. (Accessed 09 Jul 2022).
Zheng Y, Ley SH, Hu FB (2018) Global aetiology and epidemiology of type 2 diabetes mellitus mellitus and its complications. Nat Rev Endocrinol 14(2):88–98. https://doi.org/10.1038/nrendo.2017.151
Johns Hopkins University & Medicine (2022) Coronavirus resource center. https://coronavirus.jhu.edu/map.html. (Accessed 09 Jul 2022).
Sattar N (2013) Revisiting the links between glycaemia, diabetes and cardiovascular disease. Diabetologia 56(4):686–695. https://doi.org/10.1007/s00125-012-2817-5
Lee R, Wong TY, Sabanayagam C (2015) Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond) 30(2):17. https://doi.org/10.1186/s40662-015-0026-2
Koye DN, Magliano DJ, Nelson RG, Pavkov ME (2018) The global epidemiology of diabetes and kidney disease. Adv Chronic Kidney Dis 25(2):121–132. https://doi.org/10.1053/j.ackd.2017.10.011
Calle-Pascual AL, Garcia-Torre N, Moraga I, Diaz JA, Duran A, Moñux G et al (2001) Epidemiology of nontraumatic lower-extremity amputation in area 7, Madrid, between 1989 and 1999: a population-based study. Diabetes mellitus Care 24(9):1686–1689. https://doi.org/10.2337/diacare.24.9.1686
Chen L, Magliano DJ, Zimmet PZ (2011) The worldwide epidemiology of type 2 diabetes mellitus-present and future perspectives. Nat Rev Endocrinol. https://doi.org/10.1038/nrendo.2011.183
Diabetes mellitus in Italy Years 2000–2016 (2017). https://www.istat.it/it/files//2017/07/Report_Diabetes_En_def.pdf. (Accessed 09 Jul 2022)
Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V et al (2014) The global prevalence of common mental disorders: a systematic review and meta- analysis 1980–2013. Int J Epidemiol 43(2):476–493. https://doi.org/10.1093/ije/dyu038
WHO (2022) Depression and Other Common Mental Disorders. Global Health Estimates https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf. (Accessed 09 Jul 2022).
WHO (2022) Depression. https://www.who.int/news-room/fact-sheets/detail/depression. (Accessed 09 July 2022)
Rucci P, Gherardi S, Tansella M, Piccinelli M, Berardi D, Bisoffi G et al (2003) Subthreshold psychiatric disorders in primary care: prevalence and associated characteristics. J Affect Disord 76(1–3):171–181. https://doi.org/10.1016/s0165-0327(02)00087-3
ISTAT (2018) Mental health at various stages of life. https://www.istat.it/it/files//2018/07/Mental-health.pdf. (Accessed 09 Jul 2022)
Ministero della Salute (2012) The Mental health system in Italy: an overview focused in regional experiences. https://www.salute.gov.it/imgs/C_17_notizie_841_listaFile_itemName7_file.pdf. (Accessed 09 Jul 2022)
Lindekilde N, Rutters F, Erik Henriksen J, Lasgaard M, Schram MT, Rubin KH et al (2021) Psychiatric disorders as risk factors for type 2 diabetes mellitus: an umbrella review of systematic reviews with and without meta- analyses. Diabetes mellitus Res Clin Pract 176:108855. https://doi.org/10.1016/j.diabres.2021.108855
Schnurr TM, Jakupović H, Carrasquilla GD, Ängquist L, Grarup N, Sørensen TIA et al (2020) Obesity, unfavourable lifestyle and genetic risk of type 2 diabetes: a case-cohort study. Diabetologia 63(7):1324–1332. https://doi.org/10.1007/s00125-020-05140-5
US Preventive Services Task Force (2021) Screening for prediabetes mellitus and type 2 diabetes mellitus: US preventive services task force recommendation statement. JAMA. 24;326(8):736-743. https://doi.org/10.1001/jama.2021.12531.
Lean ME, Powrie JK, Anderson AS, Garthwaite PH (1990) Obesity, weight loss and prognosis in type 2 diabetes mellitus. Diabet Med 7(3):228–233. https://doi.org/10.1111/j.1464-5491.1990.tb01375.x
American Diabetes Association (2018) 2. Classification and Diagnosis of Diabetes: standards of Medical Care in Diabetes-2018. Diabetes Care. 41(Suppl 1):S13-S27. https://doi.org/10.2337/dc18-S002
PHQ Screeners Website (2022). https://www.phqscreeners.com/images/sites/g/files/g10060481/f/201412/PHQ_Italian%20for%20Italy.pdf. Accessed 09 July 2022.
Avasthi A, Grover S, Bhansali A, Kate N, Kumar V, Das EM et al (2015) Presence of common mental disorders in patients with diabetes mellitus using a two-stage evaluation method. Indian J Med Res 141(3):364–367. https://doi.org/10.4103/0971-5916.156580
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K et al (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA. https://doi.org/10.1001/jama.292.14.1724
Lean ME, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L et al (2018) Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. https://doi.org/10.1016/S0140-6736(17)33102-1
Owens-Gary MD, Zhang X, Jawanda S, Bullard KM, Allweiss P, Smith BD (2019) The Importance of Addressing Depression and Diabetes Distress in Adults with Type 2 Diabetes. J Gen Intern Med 34(2):320–324. https://doi.org/10.1007/s11606-018-4705-2
Diabetes Canada Clinical Practice Guidelines Expert Committee (2018) Diabetes and Mental Health. Can J Diabetes 42(Suppl 1):S130–S141. https://doi.org/10.1016/j.jcjd.2017.10.031
de Groot M, Golden SH, Wagner J (2016) Psychological conditions in adults with diabetes. Am Psychol 71(7):552–562. https://doi.org/10.1037/a0040408
Khaledi M, Haghighatdoost F, Feizi A, Aminorroaya A (2019) The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol 56(6):631–650. https://doi.org/10.1007/s00592-019-01295-9
Holman N, Wild SH, Khunti K, Knighton P, OKeefe, Bakhai JC et al (2022) Incidence and characteristics of remission of type 2 diabetes mellitus in England: a Cohort study using the national diabetes mellitus audit. Diabetes mellitus Care. https://doi.org/10.2337/dc21-2136
Wing RR, Phelan S (2005) Long-term weight loss maintenance. Am J Clin Nutr 82(1 Suppl):222S-225S. https://doi.org/10.1093/ajcn/82.1.222S
Rotella F, Mannucci E (2013) Depression as a risk factor for diabetes mellitus: a meta- analysis of longitudinal studies. J Clin Psychiatry 74(1):31–37. https://doi.org/10.4088/JCP.12r07922
Mezuk B, Eaton WW, Albrecht S, Golden SH (2008) Depression and type 2 diabetes mellitus over the lifespan: a meta-analysis. Diabetes mellitus Care 31(12):2383–2390. https://doi.org/10.2337/dc08-0985
Velapati SR, Shah M, Kuchkuntla AR, Abu-Dayyeh B, Grothe K, Hurt RT et al (2018) weight regain after bariatric surgery: prevalence, Etiology, and Treatment. Curr Nutr Rep 7(4):329–334. https://doi.org/10.1007/s13668-018-0243-0
Barrea L, Pugliese G, Framondi L, Di Matteo R, Laudisio D, Savastano S et al (2020) Does Sars-Cov-2 threaten our dreams? Effect of quarantine on sleep quality and body mass index. J Transl Med 18(1):318. https://doi.org/10.1186/s12967-020-02465-y
Claro AE, Palanza C, Tartaglione L, Mazza M, Janiri L, Pitocco D (2022) COVID-19 and the role of chronic inflammation in patients with type 2 diabetes and depression. Minerva Endocrinol (Torino) 47(1):128–129. https://doi.org/10.23736/S2724-6507.21.03492-8
Lloyd CE, Nouwen A, Sartorius N, Ahmed HU, Alvarez A, Bahendeka S, Basangwa D et al (2018) Prevalence and correlates of depressive disorders in people with Type 2 diabetes: results from the international prevalence and treatment of diabetes and depression (INTERPRET-DD) study, a collaborative study carried out in 14 countries. Diabet Med 35(6):760–769. https://doi.org/10.1111/dme.13611
Brazeau AS, Hajna S, Joseph L, Dasgupta K (2015) Correlates of sitting time in adults with type 2 diabetes mellitus. BMC Public Health 15:793. https://doi.org/10.1186/s12889-015-2086-6
Lee SWH, Ng KY, Chin WK (2017) The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: a systematic review and meta-analysis. Sleep Med Rev 31:91–101. https://doi.org/10.1016/j.smrv.2016.02.001
Thomson CA, Morrow KL, Flatt SW, Wertheim BC, Perfect MM, Ravia JJ et al (2012) Relationship between sleep quality and quantity and weight loss in women participating in a weight-loss intervention trial. Obesity 20(7):1419–1425. https://doi.org/10.1038/oby.2012.62
Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, Safren SA (2008) Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care 31(12):2398–2403. https://doi.org/10.2337/dc08-1341
Hert M, Correll CU, Bobes J, CetkovichBakmas M, Cohen D, Asai I et al (2011) Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 10(1):52–77. https://doi.org/10.1002/j.2051-5545.2011.tb00014.x
Acknowledgements
We are grateful to Maria Rita Scardocci and Paolo Palanza for their technical support.
Funding
Open access funding provided by Università Cattolica del Sacro Cuore within the CRUI-CARE Agreement. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AEC and CP designed the study and wrote the first draft of the manuscript. MR and CdW were responsible for the statistical part of the study. AEC, SP and AC administered the PHQ. AEC was the coordinator of the project. MM, AC, AR, LT, CdW, GM, SP, GEUMS, MR, PM, AP, LJ, GS, DP supervised and added important contributions to the paper. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the institutional committee and with the Declaration of Helsinki and its later amendments. The study protocol was approved by the Ethics Committee (EC) of the FPUAG Università Cattolica del Sacro Cuore, on 08/08/2020 with number ID 3298 and protocol number 0040703/20.
Informed consent
Informed consent was obtained from all participants in this study.
Additional information
Managed by Massimo Porta.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Claro, A.E., Palanza, C., Mazza, M. et al. Evaluation of the prevalence of the most common psychiatric disorders in patients with type 2 diabetes mellitus using the patient health questionnaire: results of the cross-sectional “DIA2PSI” study. Acta Diabetol 60, 247–255 (2023). https://doi.org/10.1007/s00592-022-01993-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-022-01993-x